Abstract
Purpose
To compare ultrasound visibility of selected biopsy markers in animal tissue models simulating axillary echotexture.
Methods
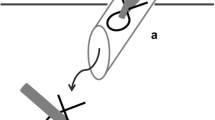
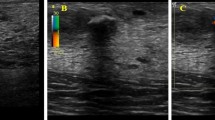
Four breast biopsy markers were selected based on size, shape, and composition and compared to an institutional standard for testing in beef steak and pork loin phantoms. BD® UltraCor™ Twirl™; Hologic® Tumark® Professional series Q, Vision, and X; and BD® UltraClip™ Dual Trigger wing-shaped (institutional standard) biopsy markers were deployed at superficial (0–2.0 cm) and deep (2.1–4.0 cm) depths in the animal models. An animal model without a biopsy marker served as control. Four participating breast imagers blinded to marker shape and location assessed ultrasound visibility of each biopsy marker using a handheld 5–12 MHz linear array transducer with a 4-point grading system (0, not visible; 1, unsure if visible; 2, visible with difficulty; 3, definite visibility). Each breast imager was asked to select the three most easily visualized biopsy markers.
Results
Total visibility scores with the four-point grading system demonstrate highest score for the Twirl™ (48/48 points), followed by the Tumark® Q (42/48) and Tumark® Vision (41/48) biopsy markers. Overall individual accuracy scores across all biopsy marker types ranged from 83.3 to 95.8%. Visibility scores based on subjective radiologist assessment also demonstrate the highest vote for the Twirl™ (11), followed by the Tumark® Vision (7) and Tumark® Q (6) biopsy markers. The wing-shaped biopsy marker had the lowest visibility and voter score.
Conclusion
The Twirl™ followed by the Tumark® Q and Vision biopsy markers demonstrates the highest visibility scores using a four-point grading system and by radiologist vote.


Similar content being viewed by others
References
Pilewskie M, Morrow M (2017) Axillary nodal management following neoadjuvant chemotherapy: a review. JAMA Oncol 3(4):549–555. https://doi.org/10.1001/jamaoncol.2016.4163
Rastogi P, Anderson SJ, Bear HD et al (2008) Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol 26(5):778–785. https://doi.org/10.1200/JCO.2007.15.0235
Schwentner L, Helms G, Nekljudova V et al (2017) Using ultrasound and palpation for predicting axillary lymph node status following neoadjuvant chemotherapy—results from the multi-center SENTINA trial. Breast 31:202–207. https://doi.org/10.1016/j.breast.2016.11.012
Hunt KK, Yi M, Mittendorf EA et al (2009) Sentinel lymph node surgery after neoadjuvant chemotherapy is accurate and reduces the need for axillary dissection in breast cancer patients. Ann Surg 250(4):558–566. https://doi.org/10.1097/SLA.0b013e3181b8fd5e
Mamounas EP, Anderson SJ, Dignam JJ et al (2012) Predictors of locoregional recurrence after neoadjuvant chemotherapy: results from combined analysis of National Surgical Adjuvant Breast and Bowel Project B-18 and B27. JCO 30(32):3960–3966. https://doi.org/10.1200/JCO.2011.40.8369
Giuliano AE, Hunt KK, Hallman KV et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6):569–575. https://doi.org/10.1001/jama.2011.90
Boughey JC, Suman VJ, Mittendorf EA et al (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) Clinical Trial. JAMA 310(14):1455–1461. https://doi.org/10.1001/jama.2013.278932
Boughey JC, Ballman KV, Le-Petross HT et al (2016) Identification and resection of clipped node decreases the false-negative rate of sentinel lymph node surgery in patients presenting with node-positive breast cancer (T0–T4, N1–N2) who receive neoadjuvant chemotherapy: results from ACOSOG Z1071 (Alliance). Ann Surg 263(4):802–807. https://doi.org/10.1097/SLA.0000000000001375
Caudle AS, Yang WT, Krishnamurthy S et al (2016) Improved axillary evaluation following neoadjuvant therapy for patients with node-positive breast cancer using selective evaluation of clipped nodes: implementation of targeted axillary dissection. J Clin Oncol 34(10):1072–1078. https://doi.org/10.1200/JCO.2015.64.0094
Diego EJ, McAuliffe PF, Soran A et al (2016) Axillary staging after neoadjuvant chemotherapy for breast cancer: a pilot study combining sentinel lymph node biopsy with radioactive seed localization of pre-treatment positive axillary lymph nodes. Ann Surg Oncol 23(5):1549–1553. https://doi.org/10.1245/s10434-015-5052-8
Shin K, Caudle AS, Kuerer HM et al (2016) Radiologic mapping for targeted axillary dissection: needle biopsy to excision. AJR 207(6):1372–1379. https://doi.org/10.2214/AJR.16.16545
Nguyen TT, Hieken TJ, Glazebrook KN, Boughey JC (2017) Localizing the clipped node in patients with node-positive breast cancer treated with neoadjuvant chemotherapy: early learning experience and challenges. Ann Surg Oncol 24(10):3011–3016. https://doi.org/10.1245/s10434-017-6023-z
Seow JHS, Phillips M, Taylor D (2012) Sonographic visibility of breast tissue markers: a tissue phantom comparison study. AJUM 15(4):149–157. https://doi.org/10.1002/j.2205-0140.2012.tb00198.x
Sakamoto N, Ogawa Y, Tsunoda Y, Fukuma E (2017) Evaluation of the sonographic visibility and sonographic appearance of the breast biopsy marker (UltraClip®) placed in phantoms and patients. Breast Cancer 24(4):585–592. https://doi.org/10.1007/s12282-016-0741-0
Sakamoto N, Fukuma E, Tsunoda Y, Teraoka K, Koshida Y (2018) Evaluation of the dislocation and long-term sonographic detectability of a hydrogel-based breast biopsy site marker. Breast Cancer 25(5):575–582. https://doi.org/10.1007/s12282-018-0854-8
Georgian-Smith D, Shiels WE (1996) From the RSNA refresher courses. Freehand interventional sonography in the breast: basic principles and clinical applications. Radiographics 16:149–161
Gresens AA, Britt RC, Feliberti EC, Britt LD (2012) Ultrasound-guided breast biopsy for surgical residents: evaluation of a phantom model. J Surg Educ 69(3):411–415. https://doi.org/10.1016/j.jsurg.2011.10.015
Nicotra JJ, Ga SB, Wallace KK, McNulty BC, Dameron RD (1994) Evaluation of a breast biopsy phantom for learning freehand ultrasound-guided biopsy of the liver. Acad Radiol 1(4):385–387
Harvey JA, Moran RE, Hamer MM, DeAngelis GA, Omary RA (1997) Evaluation of a Turkey-breast phantom for teaching freehand, US-guided core-needle breast biopsy. Acad Radiol 4(8):565–569. https://doi.org/10.1016/S1076-6332(97)80206-1
Mendelson EB, Böhm-Vélez M, Berg WA et al (2013) ACR BI-RADS® ultrasound. In: ACR BI-RADS® atlas, breast imaging reporting and data system. American College of Radiology, Reston
Becton, Dickinson, and Co. UltraClip™ dual trigger breast tissue marker. https://www.crbard.com/Biopsy/en-US/Products/ULTRACLIP-Breast-Tissue-Marker-Bard-Biopsy. Accessed 9 Jan 2019
Becton, Dickinson, and Co. UltraCor™ Twirl™ breast tissue marker. https://www.crbard.com/Biopsy/en-US/Products/ULTRACOR-TWIRL-Breast-Tissue-Marker-Bard-Biopsy. Accessed 9 Jan 2019
Hologic, Inc. Biopsy site marking solutions. Breast biopsy markers. https://www.hologic.com/hologic-products/breast-skeletal/breast-biopsy-markers#resources. Accessed 9 Jan 2019
Plecha D, Bai S, Patterson H, Thompson C, Shenk R (2015) Improving the accuracy of axillary lymph node surgery in breast cancer with ultrasound-guided wire localization of biopsy proven metastatic lymph nodes. Ann Surg Oncol 22:4241–4246
Siso C, de Torres J, Esgueva-Colmenarego A et al (2018) Intraoperative ultrasound-guided excision of axillary clip in patients with node-positive breast cancer treated with neoadjuvant therapy (ILINA trial): a new tool to guide the excision of the clipped node after neoadjuvant treatment. Ann Surg Oncol 25:784–791
Hartmann S, Reimer T, Gerber B, Stubert J, Stengel B, Staches A (2018) Wire localization of clip-marked axillary lymph nodes in breast cancer patients treated with primary systemic therapy. Eur J Surg Oncol 44:1307–1311
Goudreau SH, Joseph JP, Seiler SJ (2015) Preoperative radioactive seed localization for nonpalpable breast lesions: techniques, pitfalls, and solutions. Radiographics 35:1319–1334
Rüland AM, Hagemann F, Reinisch M et al (2018) Using a new marker clip system in breast cancer: Tumark® Vision® clip—feasibility testing in everyday clinical practice. Breast Care 13(2):116–120. https://doi.org/10.1159/000486388
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or live animals performed by any of the authors.
Informed consent: Informed consent is not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Portnow, L.H., Kwak, E., Senapati, G.M. et al. Ultrasound visibility of select breast biopsy markers for targeted axillary node localization following neoadjuvant treatment: simulation using animal tissue models. Breast Cancer Res Treat 184, 185–192 (2020). https://doi.org/10.1007/s10549-020-05840-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05840-x