Abstract
Purpose
To examine associations between the UGT2B17 gene deletion and exemestane metabolites, and commonly reported side effects (fatigue, hot flashes, and joint pain) among postmenopausal women participating in the MAP.3 chemoprevention trial.
Methods
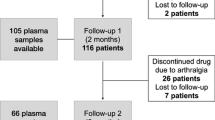
The analytical samples for the UGT2B17 analysis comprised 1752 women on exemestane and 1721 women on placebo; the exemestane metabolite analysis included 1360 women on exemestane with one-year serum samples. Both the UGT2B17 gene deletion and metabolites were measured in blood. The metabolites were conceptualized as a ratio (17-DHE-Gluc:17-DHE). Symptoms were assessed using the CTCAE v4.0 at approximately 1-year intervals. Log-binomial regression was used to examine the associations between UGT2B17 deletion, exemestane metabolites and each side effect at 1 and up to 5-year follow-up, adjusting for potential confounders.
Results
Among individuals on exemestane with the UGT2B17 gene deletion (i.e., lower detoxification), a higher risk of severe fatigue (RR = 2.59 95% CI: 1.14–5.89) was observed at up to 5-year follow-up. Among individuals on placebo, those with the UGT2B17 gene deletion had a higher risk of any fatigue (RR = 1.39, 95% CI: 1.02–1.89) at year 1. A lower metabolite ratio (poor detoxification) was associated with a higher risk of any fatigue, hot flashes and joint pain at year 1 (fatigue: RR = 1.89, 95% CI: 1.16–3.09; hot flashes: RR = 1.77, 95% CI: 1.40–2.24; joint pain: RR = 2.05, 95% CI: 1.35–3.12); similar associations were observed at 5-year follow-up.
Conclusion
Variation in the metabolism of exemestane through the UGT2B17-mediated pathway is associated with subsequent risk of commonly reported symptoms in MAP.3.

Similar content being viewed by others
References
Goss PE, Ingle JN, Ales-Martinez JE, Cheung AM, Chlebowski RT, Wactawski-Wende J, McTiernan A, Robbins J, Johnson KC, Martin LW et al (2011) Exemestane for breast-cancer prevention in postmenopausal women. N Engl J Med 364(25):2381–2391
Gatti-Mays ME, Venzon D, Galbo CE, Singer A, Reynolds J, Makariou E, Kallakury B, Heckman-Stoddard BM, Korde L, Isaacs C et al (2016) Exemestane use in postmenopausal women at high risk for invasive breast cancer: evaluating biomarkers of efficacy and safety. CancerPrevRes(Phila) 9(3):225–233
Breast Cancer Risk Reduction [https://www2.tri-kobe.org/nccn/guideline/breast/english/breast_risk.pdf]
Chouinard S, Pelletier G, Bélanger A, Barbier O (2005) Cellular specific expression of the androgen-conjugating enzymes UGT2B15 and UGT2B17 in the human prostate epithelium. Endocr Res 30(4):717–725
Lazarus P, Zheng Y, Aaron Runkle E et al (2006) Genotype-phenotype correlation between the polymorphic UGT2B17 gene deletion and NNAL glucuronidation activities in human liver microsomes. Pharmacogenet Genomics 15(11):769–778
Sun D, Chen G, Dellinger RW, Sharma AK, Lazarus P (2010) Characterization of 17-dihydroexemestane glucuronidation: potential role of the UGT2B17 deletion in exemestane pharmacogenetics. Pharmacogenet Genom 20(10):575–585
Luo S, Chen G, Truica C, Baird CC, Leitzel K, Lazarus P (2018) Role of the UGT2B17 deletion in exemestane pharmacogenetics. Pharmacogenomics J 18(2):295–300
McCarroll SA, Hadnott TN, Perry GH, Sabeti PC, Zody MC, Barrett JC, Dallaire S, Gabriel SB, Lee C, Daly MJ et al (2006) Common deletion polymorphisms in the human genome. Nat Genet 38(1):86–92
Lazarus P, Sun D (2010) Potential role of UGT pharmacogenetics in cancer treatment and prevention: focus on tamoxifen and aromatase inhibitors. Drug Metab Rev 42(1):182–194
Gauthier-Landry L, Belanger A, Barbier O (2015) Multiple roles for UDP-glucuronosyltransferase (UGT)2B15 and UGT2B17 enzymes in androgen metabolism and prostate cancer evolution. J Steroid Biochem Mol Biol 145:187–192
Giroux S, Bussieres J, Bureau A, Rousseau F (2012) UGT2B17 gene deletion associated with an increase in bone mineral density similar to the effect of hormone replacement in postmenopausal women. Osteoporos Int 23:1163–1170
Yang TL, Chen XD, Guo Y, Lei SF, Wang JT, Zhou Q, Pan F, Chen Y, Zhang ZX, Dong SS et al (2008) Genome-wide copy-number-variation study identified a susceptibility gene, UGT2B17, for osteoporosis. Am J Hum Genet 83:663–674
Kamdem LK, Xi J, Clark BL et al (2019) Exemestane may be less detrimental than letrozole to bone health in women homozygous for the UGT2B17*2 gene deletion. Breast Cancer Res Treat 175:297–303
Chavez-MacGregor M, Elias SG, Onland-Moret NC, van der Schouw YT, Van Gils CH, Monninkhof E, Grobbee DE, Peeters PHM (2005) Postmenopausal breast cancer risk and cumulative number of menstrual cycles. Cancer Epidemiol Biomarkers Prev 14(4):799–804
Barron TI, Connolly R, Bennett K, Feely J, Kennedy MJ (2007) Early discontinuation of tamoxifen: a lesson for oncologists. Cancer 109(5):832–839
Chlebowski RT, Geller ML (2006) Adherence to endocrine therapy for breast cancer. Oncology 71(1–2):1–9
Fontein DB, Nortier JW, Liefers GJ, Putter H, Meershoek-Klein Kranenbarg E, van den Bosch J, Maartense E, Rutgers EJ, van de Velde CJ (2012) High non-compliance in the use of letrozole after 2.5 years of extended adjuvant endocrine therapy.s Results from the IDEAL randomized trial. Eur J Surg Oncol. 38(2):110–117
Hadji P (2010) Improving compliance and persistence to adjuvant tamoxifen and aromatase inhibitor therapy. Crit Rev Oncol Hematol 73(2):156–166
Partridge AH, LaFountain A, Mayer E, Taylor BS, Winer E, Asnis-Alibozek A (2008) Adherence to initial adjuvant anastrozole therapy among women with early-stage breast cancer. J Clin Oncol 26(4):556–562
Aiello Bowles EJ, Boudreau DM, Chubak J, Yu O, Fujii M, Chestnut J, Buist DS (2012) Patient-reported discontinuation of endocrine therapy and related adverse effects among women with early-stage breast cancer. J Oncol Pract 8(6):e149–157
Fallowfield L (2007) Quality of life issues in relation to the aromatase inhibitor. J Steroid Biochem Mol Biol 106(1–5):168–172
Henry NL, Azzouz F, Desta Z, Li L, Nguyen AT, Lemler S, Hayden J, Tarpinian K, Yakim E, Flockhart DA et al (2012) Predictors of aromatase inhibitor discontinuation as a result of treatment-emergent symptoms in early-stage breast cancer. J Clin Oncol 30(9):936–942
Kyvernitakis I, Ziller V, Hars O, Bauer M, Kalder M, Hadji P (2014) Prevalence of menopausal symptoms and their influence on adherence in women with breast cancer. Climacteric 17(3):252–259
Hershman DL, Shao T, Kushi LH, Buono D, Tsai WY, Fehrenbacher L, Kwan M, Gomez SL, Neugut AI (2011) Early discontinuation and non-adherence to adjuvant hormonal therapy are associated with increased mortality in women with breast cancer. Breast Cancer Res Treat 126(2):529–537
Makubate B, Donnan PT, Dewar JA, Thompson AM, McCowan C (2013) Cohort study of adherence to adjuvant endocrine therapy, breast cancer recurrence and mortality. Br J Cancer 108(7):1515–1524
Maunsell E, Goss PE, Chlebowski RT, Ingle JN, Ales-Martinez JE, Sarto GE, Fabian CJ, Pujol P, Ruiz A, Cooke AL et al (2014) Quality of life in MAP.3 (Mammary Prevention 3): a randomized, placebo-controlled trial evaluating exemestane for prevention of breast cancer. J Clin Oncol 32(14):1427–1436
Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, Guyatt GH, Norton PG, Dunn E (1996 Jul) A menopause-specific quality of life questionnaire: development and psychometric properties. Maturitas. 24(3):161–75
Cella D, Hahn EA, Dineen K (2002) Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res 11:207–221
Osoba D, Bezjak A, Brundage M, Zee B, Tu D, Pater J (2005) Analysis and interpretation of health-related quality-of-life data from clinical trials: basic approach of the National Cancer Institute of Canada Clinical Trials Group. Eur J Cancer 41:280–287
Wilson W, Pardo-Manuel De Villena F, Lyn-Cook BD et al (2004) Characterization of a common deletion polymorphism of the UGT2B17 gene linked to UGT2B15. Genomics 84:707–714
Lazarus P, Zheng Y, Aaron Runkle E, Muscat JE, Wiener D (2005) Genotype-phenotype correlation between the polymorphic UGT2B17 gene deletion and NNAL glucuronidation activities in human liver microsomes. Pharmacogenet Genom 15:769–778
Wang LZ, Goh SH, Wong ALA et al (2015) Validation of a rapid and sensitive LC-MS/MS method for determination of exemestane and its metabolites, 17β-hydroxyexemestane and 17β-hydroxyexemestane-17-O-β-D-glucuronide: application to human pharmacokinetics study. PLoS One 10:e0118553. https://doi.org/10.1371/journal.pone.0118553
Acknowledgements
We thank the 4560 women who agreed to participate in this study; the trial committee; the many investigators, pharmacists, and clinical research associates involved in the trial; the Central Office staff of the Canadian Clinical Trials Group who contributed to the conduct of the main trial and Pfizer Pharmaceuticals for support and for providing exemestane and placebo. We also thank the entire Mammary Prevention 3 (MAP.3) investigator group. Finally, we thank the Mass Spectrometry Core facility and the Genomic Core facility at Washington State University-Spokane for their help with UPLC-MS and genotyping, respectively. We are also very grateful to Zuping Xia in the Department of Pharmaceutical Sciences at Washington State University for providing 17β-DHE as a standard for these studies.
Author information
Authors and Affiliations
Consortia
Contributions
PG, HR and the MAP3 Investigators directed the MAP.3 trial. Each author has directly participated in the planning, execution, or analysis of the current study. VH, RP, PL and HR designed the study’s analytic strategy and interpreted the results. DT and HR provided advice on study design or data analysis. VH, RP and HR drafted the manuscript. All authors critically revised and commented on the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
This study was funded by a grant (RO1-CA164366) from the National Cancer Institute at the National Institutes of Health to P. Lazarus (PI) and H. Richardson (Sub-award PI). Employment or Leadership Position: None; Consultant or Advisory Role: None; Stock Ownership: None; Honoraria: None; Expert Testimony: None; Patents, Royalties, and Licenses: None; Other Remuneration: None. Research Funding from company: Harriet Richardson and the CCTG held an IIR grant from Pfizer for the MAP.3 trial (2004–2016); Vikki Ho holds a Sex and Gender Science Chair in Cancer Research from the Canadian Institutes for Health Research and is currently supported by the Cancer Research Society, Fonds de recherche du Québec – Santé (FRQS) and Ministère de l'Économie, de la Science et de l'Innovation du Québec (MESI). Shaman Luo received a China Scholarship Council grant (File No. 201406600026). Romain Pasque declares that he has no conflict of interest. Gang Chen declares that he has no conflict of interest. Paul Goss declares that he has no conflict of interest. Dongsheng Tu declares that he has no conflict of interest. Philip Lazarus declares that he has no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study and only those that also consented to genetic testing were included in the analyses presented in this paper.
Research involving human participants
All procedures performed in this study were in accordance with the ethical standards of the Queens’s Health Sciences Research Ethics Board and with the 1964 Helsinki declaration on medical research in human subjects and the Canadian Tri-Council Policy Statement on the Ethical Conduct for Research Involving Humans (TCPS).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ho, V., Pasquet, R., Luo, S. et al. Variation in the UGT2B17 genotype, exemestane metabolism and menopause-related toxicities in the CCTG MAP.3 trial. Breast Cancer Res Treat 183, 705–716 (2020). https://doi.org/10.1007/s10549-020-05812-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05812-1