Abstract
Purpose
Breast cancer treatment-related lymphedema (BCRL) evaluation is frequently performed using portable measures of limb volume and bioimpedance asymmetry. Here quantitative magnetic resonance imaging (MRI) is applied to evaluate deep and superficial tissue impairment, in both surgical and contralateral quadrants, to test the hypothesis that BCRL impairment is frequently bilateral and extends beyond regions commonly evaluated with portable external devices.
Methods
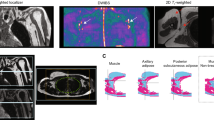
3-T MRI was applied to investigate BCRL topographical impairment. Female BCRL (n = 33; age = 54.1 ± 11.2 years; stage = 1.5 ± 0.8) and healthy (n = 33; age = 49.4 ± 11.0 years) participants underwent quantitative upper limb MRI relaxometry (T2), bioimpedance asymmetry, arm volume asymmetry, and physical evaluation. Parametric tests were applied to evaluate study measurements (i) between BCRL and healthy participants, (ii) between surgical and contralateral limbs, and (iii) in relation to clinical indicators of disease severity. Two-sided p-value < 0.05 was required for significance.
Results
Bioimpedance asymmetry was significantly correlated with MRI-measured water relaxation (T2) in superficial tissue. Deep muscle (T2 = 37.6 ± 3.5 ms) and superficial tissue (T2 = 49.8 ± 13.2 ms) relaxation times were symmetric in healthy participants. In the surgical limbs of BCRL participants, deep muscle (T2 = 40.5 ± 4.9 ms) and superficial tissue (T2 = 56.0 ± 14.8 ms) relaxation times were elevated compared to healthy participants, consistent with an edematous micro-environment. This elevation was also observed in contralateral limbs of BCRL participants (deep muscle T2 = 40.3 ± 5.7 ms; superficial T2 = 56.6 ± 13.8 ms).
Conclusions
Regional MRI measures substantiate a growing literature speculating that superficial and deep tissue, in surgical and contralateral quadrants, is affected in BCRL. The implications of these findings in the context of titrating treatment regimens and understanding malignancy recurrence are discussed.






Similar content being viewed by others
References
DiSipio T, Rye S, Newman B, Hayes S (2013) Incidence of unilateral arm lymphoedema after breast cancer: a systematic review and meta-analysis. Lancet Oncol 14(6):500–515
He L, Qu H, Wu Q, Song Y (2020) Lymphedema in survivors of breast cancer. Oncology letters 19(3):2085–2096
Morgan PA, Franks PJ, Moffatt CJ (2005) Health-related quality of life with lymphoedema: a review of the literature. International wound journal 2(1):47–62
Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol 26(21):3536–3542
Ridner SH, Sinclair V, Deng J, Bonner CM, Kidd N, Dietrich MS (2012) Breast cancer survivors with lymphedema: glimpses of their daily lives. Clinical journal of oncology nursing 16(6):609–614
Armer JM, Radina ME, Porock D, Culbertson SD (2003) Predicting breast cancer-related lymphedema using self-reported symptoms. Nurs Res 52(6):370–379
Asdourian MS, Swaroop MN, Sayegh HE, Brunelle CL, Mina AI, Zheng H, Skolny MN, Taghian AG (2017) Association between precautionary behaviors and breast cancer-related lymphedema in patients undergoing bilateral surgery. Journal of clinical 35(35):3934–3941
Bradley JA, Bellon JR (2020) Quality of Life and Limb: Reducing Lymphedema Risk After Breast Cancer Therapy. Int J Radiat Oncol Biol Phys 106(2):225–229
Shah C, Arthur DW, Wazer D, Khan A, Ridner S, Vicini F (2016) The impact of early detection and intervention of breast cancer-related lymphedema: a systematic review. Cancer Med 5(6):1154–1162
Soran A, Ozmen T, McGuire KP, Diego EJ, McAuliffe PF, Bonaventura M, Ahrendt GM, DeGore L, Johnson R (2014) The importance of detection of subclinical lymphedema for the prevention of breast cancer-related clinical lymphedema after axillary lymph node dissection; a prospective observational study. Lymphatic research and biology 12(4):289–294
Stout Gergich NL, Pfalzer LA, McGarvey C, Springer B, Gerber LH, Soballe P (2008) Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer 112(12):2809–2819
Stout NL, Pfalzer LA, Levy E, McGarvey C, Gerber L, Springer B, Soballe P (2011) Five Year Preliminary Outcomes of a Prospective Surveillance Model To Reduce Upper Extremity Morbidity Related to Breast Cancer Treatment. Cancer Research
Korteweg MA, Zwanenburg JJ, Hoogduin JM, van den Bosch MA, van Diest PJ, van Hillegersberg R, Eijkemans MJ, Mali WP, Luijten PR, Veldhuis WB (2011) Dissected sentinel lymph nodes of breast cancer patients: characterization with high-spatial-resolution 7-T MR imaging. Radiology 261(1):127–135
Korteweg MA, Zwanenburg JJ, van Diest PJ, van den Bosch MA, Luijten PR, van Hillegersberg R, Mali WP, Veldhuis WB (2011) Characterization of ex vivo healthy human axillary lymph nodes with high resolution 7 Tesla MRI. Eur Radiol 21(2):310–317
Crescenzi R, Donahue PMC, Mahany H, Lants SK, Donahue MJ (2020) CEST MRI quantification procedures for breast cancer treatment-related lymphedema therapy evaluation. Magn Reson Med 83(5):1760–1773
Rane S, Donahue PM, Towse T, Ridner S, Chappell M, Jordi J, Gore J, Donahue MJ (2013) Clinical feasibility of noninvasive visualization of lymphatic flow with principles of spin labeling MR imaging: implications for lymphedema assessment. Radiology 269(3):893–902
Donahue MJ, Donahue PC, Rane S, Thompson CR, Strother MK, Scott AO, Smith SA (2016) Assessment of lymphatic impairment and interstitial protein accumulation in patients with breast cancer treatment-related lymphedema using CEST MRI. Magn Reson Med 75(1):345–355
Crescenzi R, Donahue PM, Braxton VG, Scott AO, Mahany HB, Lants SK, Donahue MJ (2018) 30 T relaxation time measurements of human lymph nodes in adults with and without lymphatic insufficiency: Implications for magnetic resonance lymphatic imaging. NMR Biomed 31(12):4009
Crescenzi R, Donahue PMC, Hartley KG, Desai AA, Scott AO, Braxton V, Mahany H, Lants SK, Donahue MJ (2017) Lymphedema evaluation using noninvasive 3T MR lymphangiography. Journal of magnetic resonance imaging : JMRI 46(5):1349–1360
Kim G, Smith MP, Donohoe KJ, Johnson AR, Singhal D, Tsai LL (2020) MRI staging of upper extremity secondary lymphedema: correlation with clinical measurements. European radiology
Pons G, Clavero JA, Alomar X, Rodriguez-Bauza E, Tom LK, Masia J (2019) Preoperative planning of lymphaticovenous anastomosis: The use of magnetic resonance lymphangiography as a complement to indocyanine green lymphography. J Plastic Reconstructive Aesthetic Surg 72(6):884–891
Donahue PM, Crescenzi R, Scott AO, Braxton V, Desai A, Smith SA, Jordi J, Meszoely IM, Grau AM, Kauffmann RM, Sweeting RS, Spotanski K, Ridner SH, Donahue MJ (2017) Bilateral changes in deep tissue environment after manual lymphatic drainage in patients with breast cancer treatment-related lymphedema. Lymphat Res Biol 15(1):45–56
Santyr GE (1994) MR imaging of the breast Imaging and tissue characterization without intravenous contrast. Magn Reson Imaging Clin N Am 2(4):673–690
Stanton AW, Northfield JW, Holroyd B, Mortimer PS, Levick JR (1997) Validation of an optoelectronic limb volumeter (Perometer). Lymphology 30(2):77–97
Warren AG, Janz BA, Slavin SA, Borud LJ (2007) The use of bioimpedance analysis to evaluate lymphedema. Ann Plast Surg 58(5):541–543
Burnand KM, Glass DM, Mortimer PS, Peters AM (2012) Lymphatic dysfunction in the apparently clinically normal contralateral limbs of patients with unilateral lower limb swelling. Clin Nucl Med 37(1):9–13
Ancukiewicz M, Russell TA, Otoole J, Specht M, Singer M, Kelada A, Murphy CD, Pogachar J, Gioioso V, Patel M, Skolny M, Smith BL, Taghian AG (2011) Standardized method for quantification of developing lymphedema in patients treated for breast cancer. Int J Radiat Oncol Biol Phys 79(5):1436–1443
Ridner SH, Bonner CM, Doersam JK, Rhoten BA, Schultze B, Dietrich MS (2014) Bioelectrical impedance self-measurement protocol development and daily variation between healthy volunteers and breast cancer survivors with lymphedema. Lymphat Res Biol 12(1):2–9
Fu MR, Cleland CM, Guth AA, Kayal M, Haber J, Cartwright F, Kleinman R, Kang Y, Scagliola J, Axelrod D (2013) L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology 46(2):85–96
Donahue PMC, Crescenzi R, Du L, Donahue MJ (2019) Implementation of Single-Tab Electrodes for Bioimpedance Spectroscopy Measures. Lymphat Res Biol
Lu H, Nagae-Poetscher LM, Golay X, Lin D, Pomper M, van Zijl PC (2005) Routine clinical brain MRI sequences for use at 3.0 Tesla. J Magnetic Resonance Imaging 22(1):13–22
Donahue MJ, Lu H, Jones CK, Edden RA, Pekar JJ, van Zijl PC (2006) Theoretical and experimental investigation of the VASO contrast mechanism. Magn Reson Med 56(6):1261–1273
Donahue MJ, Achten E, Cogswell PM, De Leeuw FE, Derdeyn CP, Dijkhuizen RM, Fan AP, Ghaznawi R, Heit JJ, Ikram MA, Jezzard P, Jordan LC, Jouvent E, Knutsson L, Leigh R, Liebeskind DS, Lin W, Okell TW, Qureshi AI, Stagg CJ, van Osch MJ, van Zijl PC, Watchmaker JM, Wintermark M, Wu O, Zaharchuk G, Zhou J, Hendrikse J (2018) Consensus statement on current and emerging methods for the diagnosis and evaluation of cerebrovascular disease. J Cerebral Blood Flow Metabol 38(9):1391–1417
Aldrich MB, Guilliod R, Fife CE, Maus EA, Smith L, Rasmussen JC, Sevick-Muraca EM (2012) Lymphatic abnormalities in the normal contralateral arms of subjects with breast cancer-related lymphedema as assessed by near-infrared fluorescent imaging. Biomedical optics express 3(6):1256–1265
Tan IC, Maus EA, Rasmussen JC, Marshall MV, Adams KE, Fife CE, Smith LA, Chan W, Sevick-Muraca EM (2011) Assessment of lymphatic contractile function after manual lymphatic drainage using near-infrared fluorescence imaging. Arch Phys Med Rehabil 92(5):756–764
Sato A, Sakai T, Iwase T, Kano F, Kimura K, Ogiya A, Koizumi M, Tanabe M, Horii R, Akiyama F, Ueno T, Ohno S (2019) Altered lymphatic drainage patterns in re-operative sentinel lymph node biopsy for ipsilateral breast tumor recurrence. Radiation Oncol 14(1):159
van der Ploeg IM, Oldenburg HS, Rutgers EJ, Baas-Vrancken Peeters MJ, Kroon BB, Valdes Olmos RA, Nieweg OE (2010) Lymphatic drainage patterns from the treated breast. Ann Surg Oncol 17(4):1069–1075
Kiluk JV, Prowler V, Lee MC, Khakpour N, Laronga C, Cox CE (2014) Contralateral axillary nodal involvement from invasive breast cancer. Breast 23(3):291–294
Shieh AC, Swartz MA (2011) Regulation of tumor invasion by interstitial fluid flow. Phys Biol 8(1):015012
Shields JD, Fleury ME, Yong C, Tomei AA, Randolph GJ, Swartz MA (2007) Autologous chemotaxis as a mechanism of tumor cell homing to lymphatics via interstitial flow and autocrine CCR7 signaling. Cancer Cell 11(6):526–538
Wigg J, Cooper G (2017) How is lymphofluoroscopy mapping altering lymphoedema management? Br J Community Nurs 22(Sup10):S16–S20
Kilgore LJ, Korentager SS, Hangge AN, Amin AL, Balanoff CR, Larson KE, Mitchell MP, Chen JG, Burgen E, Khan QJ, O'Dea AP, Nye L, Sharma P, Wagner JL (2018) Reducing Breast Cancer-Related Lymphedema (BCRL) Through Prospective Surveillance Monitoring Using Bioimpedance Spectroscopy (BIS) and Patient Directed Self-Interventions. Ann Surg Oncol 25(10):2948–2952
Whitworth PW, Cooper A (2018) Reducing chronic breast cancer-related lymphedema utilizing a program of prospective surveillance with bioimpedance spectroscopy. Breast J 24(1):62–65
Ridner SH, Dietrich MS, Cowher MS, Taback B, McLaughlin S, Ajkay N, Boyages J, Koelmeyer L, DeSnyder SM, Wagner J, Abramson V, Moore A, Shah C (2019) A Randomized Trial Evaluating Bioimpedance Spectroscopy Versus Tape Measurement for the Prevention of Lymphedema Following Treatment for Breast Cancer: Interim Analysis. Ann Surg Oncol 26(10):3250–3259
Torres Lacomba M, Yuste Sanchez MJ, Zapico Goni A, Prieto Merino D, Mayoral del Moral O, Cerezo Tellez E, Minayo Mogollon E (2010) Effectiveness of early physiotherapy to prevent lymphoedema after surgery for breast cancer: randomised, single blinded, clinical trial. BMJ 340:b5396
Huang TW, Tseng SH, Lin CC, Bai CH, Chen CS, Hung CS, Wu CH, Tam KW (2013) Effects of manual lymphatic drainage on breast cancer-related lymphedema: a systematic review and meta-analysis of randomized controlled trials. World J Surg Oncol 11:15
Badger C, Preston N, Seers K, Mortimer P (2004) Physical therapies for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev (4):CD003141
Belgrado JP, Vandermeeren L, Vankerckhove S, Valsamis JB, Malloizel-Delaunay J, Moraine JJ, Liebens F (2016) Near-Infrared Fluorescence Lymphatic Imaging to Reconsider Occlusion Pressure of Superficial Lymphatic Collectors in Upper Extremities of Healthy Volunteers. Lymphat Res Biol 14(2):70–77
Angooti Oshnari L, Hosseini SA, Haghighat S, Hossein Zadeh S (2016) The Effect of Complete Decongestive Therapy on Edema Volume Reduction and Pain in Women With Post Breast Surgery Lymph Edema. Iran J Cancer Prev 9(2):e4209
Armer JM, Hulett JM, Bernas M, Ostby P, Stewart BR, Cormier JN (2013) Best Practice Guidelines in Assessment, Risk Reduction, Management, and Surveillance for Post-Breast Cancer Lymphedema. Curr Breast Cancer Rep 5(2):134–144
Ezzo J, Manheimer E, McNeely ML, Howell DM, Weiss R, Johansson KI, Bao T, Bily L, Tuppo CM, Williams AF, Karadibak D (2015) Manual lymphatic drainage for lymphedema following breast cancer treatment. Cochrane Database Syst Rev 5:CD003475
Aldrich MB, Marshall MV, Sevick-Muraca EM, Lanza G, Kotyk J, Culver J, Wang LV, Uddin J, Crews BC, Marnett LJ, Liao JC, Contag C, Crawford JM, Wang K, Reisdorph B, Appelman H, Turgeon DK, Meyer C, Wang T (2012) Seeing it through: translational validation of new medical imaging modalities. Biomed Opt Express 3(4):764–776
Aldrich MB, Gross D, Morrow JR, Fife CE, Rasmussen JC (2017) Effect of pneumatic compression therapy on lymph movement in lymphedema-affected extremities, as assessed by near-infrared fluorescence lymphatic imaging. Journal of innovative optical health sciences 10(2)
Munn LL, Padera TP (2014) Imaging the lymphatic system. Microvasc Res 96:55–63
Giacalone GBJP, Bourgeois P, Bracale P, Roeh N, Moraine JJ (2011) A New Dynamic Imaging Tool to Study Lymphoedema and Associated Treatments. Eu J Lymphol 22(62):11–14
Acknowledgements
Research funding provided by the National Institutes of Health National Institute for Nursing Research 1R01NR015079 and the Lipedema Foundation postdoctoral fellowship
Funding
This study was funded by the National Institutes of Health (NIH) National Institute for Nursing Research (NINR) grant number 1R01NR015079.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Author Manus J. Donahue has received research-related funding from the NIH, receives research-related support from Philips Healthcare, is a paid consultant for Global Blood Therapeutics, Pfizer, and bluebird bio, and is the CEO of biosight, LLC which provides healthcare technology consulting services.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
All human subjects provided informed, written consent (IRB #181698).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Donahue, P.M.C., Crescenzi, R., Lee, C. et al. Magnetic resonance imaging and bioimpedance evaluation of lymphatic abnormalities in patients with breast cancer treatment-related lymphedema. Breast Cancer Res Treat 183, 83–94 (2020). https://doi.org/10.1007/s10549-020-05765-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05765-5