Abstract
Purpose
Although there has been a significant increase in the use of oncoplastic surgery (OPS), data on the postoperative safety of this approach are limited compared to traditional lumpectomy. This study aimed to compare the immediate (30-day) postoperative complications associated with OPS and traditional lumpectomy.
Methods
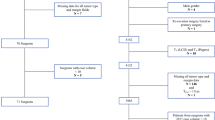
An analysis of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database was performed on women with breast cancer who underwent OPS or traditional lumpectomy. Logistic regression was used to explore the effect of type of surgery on the outcome of interest.
Results
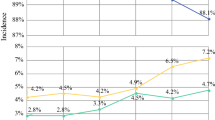
A total of 109,487 women were analyzed of whom 8.3% underwent OPS. OPS had a longer median operative time than traditional lumpectomy. The unadjusted immediate (30-day) overall complication rate was significantly higher with OPS than traditional lumpectomy (3.8% versus 2.6%, p < 0.001). After adjusting for baseline differences, overall 30-day postoperative complications were significantly higher amongst women undergoing OPS compared with traditional lumpectomy (OR 1.41, 95%CI 1.24–1.59). Factors that were independent predictors of overall 30-day complications included higher age, higher BMI, race, smoking status, lymph node surgery, neoadjuvant chemotherapy, ASA class ≥ 3, in situ disease, and year of operation. The interaction term between type of surgery and operative time was not statistically significant, indicating that operative time did not modify the effect of type of surgery on immediate postoperative complications.
Conclusions
Although there were slightly higher overall complication rates with OPS, the absolute rates remained quite low for both groups. Therefore, OPS may be performed in women with breast cancer who are suitable candidates.

Similar content being viewed by others
Abbreviations
- ACS NSQIP:
-
American College of Surgeons National Surgical Quality Improvement Program
- ASA:
-
American Society of Anesthesiology
- ALND:
-
Axillary lymph node dissection
- CHF:
-
Congestive heart failure
- COPD:
-
Chronic obstructive pulmonary disease
- CPT:
-
Current procedural terminology
- ICD-9:
-
International Classification of Diseases Ninth Revision
- OPS:
-
Oncoplastic surgery
- PCI:
-
Percutaneous coronary intervention
- PUF:
-
Participant user data file
- SLNB:
-
Sentinel lymph node biopsy
- TIA:
-
Transient ischemic attack
- UTI:
-
Urinary tract infection
References
Chatterjee A, Gass J, Patel K, Holmes D, Kopkash K, Peiris L, Peled A, Ryan J, El-Tamer M, Reiland J (2019) A consensus definition and classification system of oncoplastic surgery developed by the American Society of Breast Surgeons. Ann Surg Oncol 26:3436–3444
El-Tamer M (2012) Principles and techniques in oncoplastic breast cancer surgery. World Scientific Publishing Co Inc., Singapore
Kelsall J, McCulley S, Brock L, Akerlund MTE, Macmillan RD (2017) Comparing oncoplastic breast conserving surgery with mastectomy and immediate breast reconstruction: case-matched patient reported outcomes. J Plastic Reconstr Aesthetic Surg 70:1377–1385
Palsdottir E, Lund L, Asgeirsson A (2018) Oncoplastic breast-conserving surgery in Iceland: a population-based study. Scand J Surg 107:224–229
Santos G, Urban C, Edelweiss MI, Zucca-Matthew G, de Oliveira VM, Arana GH, Iera M, Rietiens M, de Lima RS, Spautz C, Kuroda F, Anselmi K, Cappo E (2015) Long term comparison of aesthetical outcomes after oncoplastic surgery and lumpectomy in breast cancer. Ann Surg Oncol 22:2500–2508
De La Cruz L, Blankenship SA, Chatterjee A, Geha R, Nocera N, Czerniecki BJ, Tchou J, Fisher CS (2016) Outcomes after oncoplastic breast-conserving surgery in breast cancer patients: a systematic literature review. Ann Surg Oncol 23:3247–3258
Losken A, Dugal CS, Styblo TM, Carlson GW (2014) A meta-analysis comparing breast conservation therapy alone to the oncoplastic technique. Ann Plast Surg 72:145–149
Brouwer de Koning SG, Vrancken Peeters MTFD, Jóźwiak K, Bhairosing PA, Ruers TJM (2018) Tumor resection margin definitions in breast-conserving surgery: systematic review and meta-analysis of the current literature. Clin Breast Cancer 18:595–600
De Lorenzi F, Loschi P, Bagnardi V, Rotmensz N, Hubner G, Mazzarol G, Orecchia R, Galimberti V, Veronesi P, Colleoni MA, Toesca A, Peradze N, Mario R (2016) Oncoplastic breast-conserving surgery for tumors larger than 2 centimeters: is it oncologically safe? A matched-cohort analysis. Ann Surg Oncol 23:1852–1859
Asban A, Homsy C, Chen L, Fisher C, Losken A, Chatterjee A (2018) A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with single stage implant reconstruction in the treatment of breast cancer. Breast 41:159–164
Chatterjee A, Asban A, Jonczyk M, Chen L, Czerniecki B, Fisher CS (2019) A cost-utility analysis comparing large volume displacement oncoplastic surgery to mastectomy with free flap reconstruction in the treatment of breast cancer. Am J Surg 218:597–604
Xue DQ, Qian C, Yang L, Wang XF (2012) Risk factors for surgical site infections after breast surgery: a systematic review and metaanalysis. Eur J Surg Oncol 38:375–381
Nizet J-L, Maweja S, Lakosi F, Lifrange E, Scagnol I, Seidel L, Albert A, Jerusalem G (2015) Oncological and surgical outcome after oncoplastic breast surgery. Acta Chir Belg 115:33–41
Cil TD, Cordeiro E (2016) Complications of oncoplastic breast surgery involving soft tissue transfer versus breast-conserving surgery: an analysis of the NSQIP database. Ann Surg Oncol 23:3266–3271
Mattingly AE, Ma Z, Smith PD, Kiluk JV, Khakpour N, Hoover SJ, Laronga C, Lee MC (2017) Early postoperative complications after oncoplastic reduction. South Med J 110:660–666
Kelemen P, Pukancsik D, Újhelyi M, Sávolt Á, Kovács E, Ivády G, Kenessey I, Kovács T, Stamatiou A, Smanykó V, Mátrai Z (2019) Comparison of clinicopathologic, cosmetic and quality of life outcomes in 700 oncoplastic and conventional breast-conserving surgery cases: a single-centre retrospective study. Eur J Surg Oncol 45:118–124
Carter SA, Lyons GR, Kuerer HM, Bassett RL Jr, Oates S, Thompson A, Caudle AS, Mittendorf EA, Bedrosian I, Lucci A, DeSnyder SM, Babiera G, Yi M, Baumann DP, Clemens MW, Garvey PB, Hunt KK, Hwang RF (2016) Operative and oncologic outcomes in 9861 patients with operable breast cancer: single-institution analysis of breast conservation with oncoplastic reconstruction. Ann Surg Oncol 23:3190–3198
Jonczyk MM, Jean J, Graham R, Chatterjee A (2019) Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat 173:267–274
Crown A, Scovel LG, Rocha FG, Scott EJ, Wechter DG, Grumley JW (2019) Oncoplastic breast conserving surgery is associated with a lower rate of surgical site complications compared to standard breast conserving surgery. Am J Surg 217:138–141
Wijgman DJ, Ten Wolde B, van Groesen NR, Keemers-Gels ME, van den Wildenberg FJ, Strobbe LJ (2017) Short term safety of oncoplastic breast conserving surgery for larger tumors. Eur J Surg Oncol 43:665–671
Maxwell J, Roberts A, Cil T, Somogyi R, Osman F (2016) Current practices and barriers to the integration of oncoplastic breast surgery: a Canadian perspective. Ann Surg Oncol 23:3259–3265
Blankensteijn LL, Crystal DT, Egeler SA, Varkevisser RRB, Ibrahim AMS, Sharma R, Lee BT, Lin SJ (2019) The influence of surgical specialty on oncoplastic breast reconstruction. Plast Reconstr Surg Glob Open 7:e2248
Tenofsky PL, Dowell P, Topalovski T, Helmer SD (2014) Surgical, oncologic, and cosmetic differences between oncoplastic and nononcoplastic breast conserving surgery in breast cancer patients. Am J Surg 207:398–402. discussion 402.
Behluli I, Le Renard PE, Rozwag K, Oppelt P, Kaufmann A, Schneider A (2019) Oncoplastic breast surgery versus conventional breast-conserving surgery: a comparative retrospective study. ANZ J Surg 89:1236–1241
Jonczyk MM, Jean J, Graham R, Chatterjee A (2019) Trending towards safer breast cancer surgeries? Examining acute complication rates from a 13-year NSQIP analysis. Cancers 11:253
Chand ND, Browne V, Paramanathan N, Peiris LJ, Laws SA, Rainsbury RM (2017) Patient reported outcomes are better after oncoplastic breast conservation than after mastectomy and autologous reconstruction. Plast Reconstr Surg Glob Open 5:e1419
Funding
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FAA declares that he has no conflict of interest. SAA declares that he has no conflict of interest. EC declares that she has no conflict of interest. DRM declares that he has no conflict of interest. TC declares that she has no conflict of interest.
Ethical approval
The Ethics Review Board has deemed this retrospective review of de-identified data exempt from institutional review. De-identified patient information is freely available to all institutional members who comply with the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) data use agreement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Angarita, F.A., Acuna, S.A., Cordeiro, E. et al. Does oncoplastic surgery increase immediate (30-day) postoperative complications? An analysis of the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database. Breast Cancer Res Treat 182, 429–438 (2020). https://doi.org/10.1007/s10549-020-05665-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05665-8