Abstract
Purpose
We estimated average medical costs due to metastatic breast cancer (mBC) among younger (aged 18–44), midlife (aged 45–64), and older women (aged 65 and older) by phase of care: initial, continuing, and terminal.
Methods
We used 2003–2014 North Carolina cancer registry data linked with administrative claims from public and private payers. We developed a claims-based algorithm to identify breast cancer patients who progressed to metastatic disease. We matched breast cancer patients (mBC and earlier stage) to non-cancer patients on age group, county of residence, and insurance plan. Outcomes were average monthly medical expenditures and expected medical expenditures by phase. We used regression to estimate excess costs attributed to mBC as the difference in mean payments between patients with mBC (N = 4806) and patients with each earlier-stage breast cancer (stage 1, stage 2, stage 3, and unknown stage; N = 21,772) and non-cancer controls (N = 109,631) by treatment phase and age group.
Results
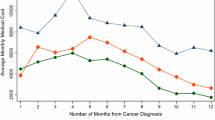
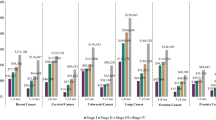
Adjusted monthly costs for women with mBC were significantly higher than for women with earlier-stage breast cancer and non-cancer controls for all age groups and treatment phases except the initial treatment among women with stage 3 breast cancer at diagnosis. The largest expected total costs were for women aged 18–44 with mBC during the continuing phase ($209,961 95% Confidence Interval $165,736–254,186).
Conclusions
We found substantial excess costs for mBC among younger women and during the continuing and terminal phases of survivorship. It is important to assess whether this care is high value for these women.



Similar content being viewed by others
References
American Cancer Society How Common is Breast Cancer? (2017). https://www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer.html. Accessed 30 July 2018
Johnson RH, Chien FL, Bleyer A (2013) Incidence of breast cancer with distant involvement among women in the United States, 1976 to 2009. JAMA J Am Med Assoc. https://doi.org/10.1001/jama.2013.776
Chollet-Hinton L, Anders CK, Tse CK et al (2016) Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina breast cancer study: a case-control study. Breast Cancer Res. https://doi.org/10.1186/s13058-016-0736-y
Anders CK, Johnson R, Litton J et al (2009) Breast cancer before age 40 years. Semin Oncol. https://doi.org/10.1053/j.seminoncol.2009.03.001
Lee HB, Han W (2014) Unique features of young age breast cancer and its management. J Breast Cancer. https://doi.org/10.4048/jbc.2014.17.4.301
Maggard MA, O’Connell JB, Lane KE et al (2003) Do young breast cancer patients have worse outcomes? J Surg Res. https://doi.org/10.1016/S0022-4804(03)00179-3
Fredholm H, Eaker S, Frisell J et al (2009) Breast cancer in young women: poor survival despite intensive treatment. PLoS ONE. https://doi.org/10.1371/journal.pone.0007695
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL (2012) Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst 104:386
Trivers KF, Fink AK, Partridge AH et al (2014) Estimates of young breast cancer survivors at risk for infertility in the US. Oncologist. https://doi.org/10.1634/theoncologist.2014-0016
Allaire BT, Ekwueme DU, Guy GP et al (2016) Medical care costs of breast cancer in privately insured women aged 18–44 years. Am J Prev Med. https://doi.org/10.1016/j.amepre.2015.08.035
Ekwueme DU, Allaire BT, Guy GP et al (2016) Treatment Costs of breast cancer among younger women aged 19–44 years enrolled in medicaid. Am J Prev Med. https://doi.org/10.1016/j.amepre.2015.10.017
Allaire BT, Ekwueme DU, Poehler D et al (2017) Breast cancer treatment costs in younger, privately insured women. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-017-4249-x
Trogdon JG, Ekwueme DU, Poehler D et al (2017) Medical costs of treating breast cancer among younger Medicaid beneficiaries by stage at diagnosis. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-017-4386-2
Surveillance Research Program NCI (2019) SEER*Explorer: an interactive website for SEER cancer statistics. https://seer.cancer.gov/explorer/. Accessed 30 Sept 2019
O’Shaughnessy J (2005) Extending survival with chemotherapy in metastatic breast cancer. Oncologist. https://doi.org/10.1634/theoncologist.10-90003-20
Campbell JD, Ramsey SD (2009) The costs of treating breast cancer in the US: a synthesis of published evidence. Pharmacoeconomics 273:199
Mariotto AB, Robin Yabroff K, Shao Y et al (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djq495
Meyer AM, Olshan AF, Green L et al (2014) Big data for population-based cancer research: the integrated cancer information and surveillance system. N C Med J. https://doi.org/10.18043/ncm.75.4.265
Short PF, Graefe DR, Schoen C (2003) Churn, churn, churn: how instability of health insurance shapes America’s uninsured problem. Issue Brief (Commonw Fund)
Primary Care Case Management in North Carolina. https://www.cga.ct.gov/2008/rpt/2008-R-0622.htm. Accessed 30 July 2018
Chubak J, Yu O, Pocobelli G et al (2012) Administrative data algorithms to identify second breast cancer events following early-stage invasive breast cancer. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djs233
Iacus SM, King G, Porro G (2012) Causal inference without balance checking: coarsened exact matching. Polit Anal. https://doi.org/10.1093/pan/mpr013
Civic Impulse L (2009) H.R. 1740 (111th): Breast Cancer Education and Awareness Requires Learning Young Act of 2009
Iacus SM, King G, Porro G (2009) Software for coarsened exact matching. J Stat Softw. https://doi.org/10.18637/jss.v030.i09
Centers for Medicare & Medicaid Services (2019) Medicare Provider Utilization and Payment Data. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/medicare-provider-charge-data. Accessed 30 Sept 2019
Dalton K, Freeman S, Bragg A (2008) Refining cost to charge ratios for calculating APC and MS-DRG relative payment weights final report. RTI International, Research Triangle Park
Smith MW, Friedman B, Karaca Z, Wong HS (2015) Predicting inpatient hospital payments in the United States: a retrospective analysis. BMC Health Serv Res. https://doi.org/10.1186/s12913-015-1040-8
Buntin MB, Zaslavsky AM (2004) Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. https://doi.org/10.1016/j.jhealeco.2003.10.005
Klabunde CN, Potosky AL, Legler JM, Warren JL (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol. https://doi.org/10.1016/S0895-4356(00)00256-0
FRED Graph Observations (2019) In: Federal Reserve Economic Data. https://fred.stlouisfed.org/series/CPIMEDSL. Accessed 30 Sept 2019
Blumen H, Fitch K, Polkus V (2016) Comparison of treatment costs for breast cancer, by tumor stage and type of service. Am Heal Drug Benefits 9:23
Edwards BK, Noone AM, Mariotto AB et al (2014) Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer 120:1290
Dusetzina SB (2016) Drug pricing trends for orally administered anticancer medications reimbursed by commercial health plans, 2000–2014. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2016.0648
Centers for Disease Control and Prevention (2019) DP19–1906: multiple approaches to support young breast cancer survivors and metastatic breast cancer patients. https://www.cdc.gov/cancer/ncccp/dp19-1906.htm. Accessed 20 Dec 2019
Franc BL, Copeland TP, Thombley R et al (2018) Geographic variation in postoperative imaging for low-risk breast cancer. JNCCN J Natl Compr Cancer Netw. https://doi.org/10.6004/jnccn.2018.7024
Rotter J, Spencer JC, Wheeler SB (2019) Financial toxicity in advanced and metastatic cancer: overburdened and underprepared. J Oncol Pract. https://doi.org/10.1200/jop.18.00518
Funding
This research was support by the Centers for Disease Control and Prevention (SIP 17–004; PIs: Trogdon and Wheeler). The database infrastructure used for this project was supported through the UNC Lineberger Comprehensive Cancer Center, University Cancer Research Fund via the State of North Carolina.
Author information
Authors and Affiliations
Contributions
Conceptualization: JGT, DUE, TLF, SBW; Data curation: CDB, XZ; Formal analysis: AG, JR, XZ; Funding acquisition: JGT, DUE, TLF, SBW; Investigation: JGT, KERH, SBW; Methodology: JGT, KERH, JR, SBW; Project administration: JGT, CDB, DUE, SBW; Resources: CDB, DUE, TLF; Software: CDB, XZ; Supervision: JGT, DUE, SBW; Validation: JGT, CDB, JR, XZ, SBW; Visualization: JGT, JR, SBW; Writing—original draft: JGT, AG, JR, SBW; Writing—review and editing: JGT, AG, KERH, JR, DUE, TLF, SBW.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Trogdon worked with the Centers for Disease Control and Prevention under Intergovernmental Personnel Act 15IPA1504755. Drs. Wheeler and Reeder-Hayes received grant funding paid to their institution from Pfizer Foundation in the past 3 years. Ms. Gogate holds a pre-doctoral fellowship position with Bristol-Myers Squibb Company for work external to this study. All other authors report no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the University of North Carolina IRB #17-2604.
Research involving human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Trogdon, J.G., Baggett, C.D., Gogate, A. et al. Medical costs associated with metastatic breast cancer in younger, midlife, and older women. Breast Cancer Res Treat 181, 653–665 (2020). https://doi.org/10.1007/s10549-020-05654-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05654-x