Abstract
Purpose
Bilateral mastectomy (BM) is traditionally performed using a single-surgeon (SS) technique (SST); a co-surgeon (CS) technique (CST), where each attending surgeon concurrently performs a unilateral mastectomy, offers an alternative approach. We sought to compare the CST and SST for BM with respect to operative times and complications.
Methods
Patients undergoing BM without reconstruction at our institution between 2005 and 2015 were identified using operative caselogs and stratified into CS- and SS-cohorts. Operative time (OT; incision to closure) was calculated. Patient age, cancer presence/stage, hormone receptor/BRCA status, breast weight, axillary procedure, and 30-day complications were extracted. Differences in OT, complications, and demographics between cohorts were assessed with t tests and Chi-square tests. A multivariate linear regression model was fit to identify factors independently associated with OT.
Results
Overall, 109 BM cases were identified (CS, n = 58 [53.2%]; SS, n = 51 [46.8%]). Average duration was significantly shorter for the CST by 33 min (21.6% reduction; CS: 120 min vs. SS: 153 min, p < 0.001), with no difference in complication rates (p = 0.65). Demographic characteristics did not differ between cohorts except for total breast weight (TBW) (CS: 1878 g vs. SS: 1452 g, p < 0.05). Adjusting for TBW, CST resulted in a 27.8% reduction in OT (44-min savings, p < 0.001) compared to SST.
Conclusions
The CST significantly reduces OT for BM procedures compared to the SST without increasing complication rates. While time-savings was < 50% and may not be ideal for every patient, the CST offers an alternative BM approach potentially best-suited for large TBW patients and those undergoing axillary procedures.
Similar content being viewed by others
Introduction
Bilateral mastectomy (BM) operations are increasingly being performed across the United States with rates tripling over the last decade [1, 2]. While some BMs are performed for bilateral disease, many BMs involve a therapeutic mastectomy coupled with a contralateral prophylactic mastectomy. With recent rates of these procedures on the rise, BMs have become an increasingly important operation for breast surgeons, and techniques aimed at improving operative efficiency without sacrificing patient outcomes are in demand [1, 3]. The traditional surgical approach for BM operations involves a single surgeon removing both breasts in succession. Recently, our group suggested the co-surgeon technique (CST) as an alternative method for performing BMs, in which two attending surgeons simultaneously perform one side of the operation. While the CST has been suggested within other surgical subspecialties as a way of effectively reducing operative times and complications and potentially improving outcomes associated with lengthy or complex bilateral procedures, our study was the first to investigate the CST in breast surgery, specifically in cases of BM followed by immediate tissue-expander reconstruction (BMTR) [4,5,6,7,8,9]. While subsequent research has suggested that this approach offers improved operative efficiency for breast reconstruction procedures, further investigation into the role of the CST in reconstruction-free mastectomies has yet to be published [10, 11]. Here, we sought to examine the role of the CST in operations in which no immediate reconstruction was performed, to specifically determine if this approach can afford comparable improvements in operative durations without concurrently increasing complication rate, similar to the results observed in the BMTR cohort.
Methods
We performed a single-center retrospective analysis of consecutive patients undergoing BM without immediate reconstruction at our institution after receiving approval from the institutional review board at Brigham and Women’s Faulkner Hospital (BWFH).
Setting
We examined BM without immediate reconstruction procedures in women at BWFH, a Harvard-affiliated non-profit community teaching hospital associated with Brigham and Women’s Hospital (BWH) and the Dana-Farber Cancer Institute. Approximately 1200 breast surgeries are performed at BWFH annually by BWH staff. A total of 11 high-volume breast surgeons (those performing ≥ 150 breast surgeries annually) performed the BM procedures without immediate reconstruction in our analysis.
Cohort selection
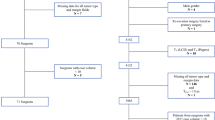
Utilizing ICD-9 codes for BM procedures, we searched billing records to identify patients undergoing BM without reconstruction between June 2005 and October 2015 at BWFH, and subsequently utilized operating room case logs to obtain the following data: breast surgeon(s), surgery start (incision) time, and surgery end time. We additionally searched BWFH tumor registry for patients undergoing bilateral mastectomy operations during this same time period. Patients who had immediate breast reconstruction, aborted breast reconstruction, or incision closure by plastic surgeons were not included in this cohort. A total of 109 women made up the final cohort. In all cases, the surgical team consisted of either one or two attending breast surgeons performing the BMs; surgical fellow, surgical resident, and/or surgical physician assistant participation was not examined and did not warrant exclusion from our study.
From the final dataset of 109 patients, retrospective chart review was conducted to extract the following demographic data: patient age at operation, presence of cancer, hormone receptor status (estrogen receptor [ER], progesterone receptor [PR], human epidermal growth factor receptor 2 [HER2]), use of neoadjuvant therapy, presence of genetic mutation (BRCA1/2), type of axillary surgery performed (sentinel lymph node biopsy [SLNB], axillary lymph node dissection [ALND], none), excised breast weight, and presence of 30-day postoperative complications. Cases were noted to include a SLNB even if the biopsy was attempted but no lymph nodes were found as long as the incision was made. The following postoperative complications were searched for by manual retrospective review of electronic medical records/chart : abscess, cellulitis, deep vein thrombosis, hematoma (non-operative and operative), skin ischemia, pulmonary embolism, skin necrosis, surgical site infection, venous thromboembolism, and wound dehiscence. Tumor stage was obtained from BWFH’s tumor registry for each case. Surgical team members, including primary and co-surgeon (if applicable), were verified for each case. The dataset was then subdivided into co-surgeon (CS) and single-surgeon (SS) groups. The final cohort consisted of 58 CS and 51 SS cases for analysis.
Statistical analysis
Operative time (OT) was calculated as the time between incision and end of the procedure. Bivariate analysis was performed to assess for differences between the CS and SS cohorts. Variables included age, presence of cancer at the time of operation, use of neoadjuvant therapy, presence of genetic mutations, total breast weight (TBW), presence of postoperative complications, type of axillary surgery performed (if applicable), and operative time.
A multivariate linear regression model was fit to examine factors associated with operative time for BMs without immediate reconstructions. Factors included use of a CS, presence of cancer, use of neoadjuvant therapy, presence of genetic mutation, breast weight, and type of axillary surgery performed (if applicable).
The dataset was built using Microsoft Excel (2011), and analyses performed using Stata 14.1 (StataCorp, College Station, TX). Student’s t test was used to calculate p values and a p value of < 0.05 was considered statistically significant. Beta and 95% confidence intervals are presented.
Results
We identified 109 patients undergoing BMs without immediate reconstruction between June 1, 2005 and October 31, 2015 at BWFH. CSs performed 58 of these cases and SSs performed the remaining 51. Amongst the entire cohort, BMs were performed most often in the setting of a cancer diagnosis (94.8% of CS and 94.1% of SS operations were performed in the setting of either unilateral or bilateral breast cancer). Stage I disease was found most frequently in both the CS (29.3%) and SS (41.2%) groups (Table 1). Among the 109 procedures, 48.6% included a SLNB and 30% included an ALND; there was no statistically significant difference found in number of axillary procedures between the CS and SS cohorts (Table 2). TBW was the only statistically significant difference in the demographic characteristics between cohorts (CS: 1878 g vs. SS 1452 g, p < 0.05, Table 2). The overall 30-day postoperative complication rate was 16.5% (n = 18). There were no statistically significant differences in the number of complications between CS and SS groups (p = 0.65). The most common complication in the CS group was cellulitis (n = 5), whereas cellulitis (n = 3) and hematoma (n = 3) were the most common in the SS group. Although cohorts were screened for additional postoperative complications including deep vein thrombosis, skin ischemia, and pulmonary embolism, there were no cases of these in the study period and, therefore, are not presented in Table 3.
The average OT for CS cases (120 min) was significantly shorter than for SS cases (153 min, p < 0.01), demonstrating a time-savings for the CS group of 33 min on average compared to the SS group (Table 3). Results of the multivariate linear regression model are presented in Table 4. A significant decrease in BM duration was observed when the procedure was performed by CSs (β = − 44.10, p < 0.001). TBW (β = 0.01, p < 0.001); the addition of unilateral and bilateral SLNB (unilateral β = 23 p < 0.01; bilateral β = 52.48, p < 0.05) and ALND (unilateral β = 34.22, p < 0.01; bilateral β = 89.16 p < 0.05) also significantly impacted operative time. The model accounted for 39% of variability in BM duration (R2 = 0.3910).
Discussion
The present study is the first to investigate the impact of an additional attending surgeon on the overall OT and the short-term postoperative complications associated with BM procedures without immediate reconstruction, in an effort to compare the CST to the single-surgeon technique (SST). The main findings are that the CST affords a reduction in OT without increasing complication rates for BM procedures. The degree of time-savings for CS procedures in the unadjusted regression was approximately 33 min, which increased to 44 min corresponding to a 27.8% reduction (p < 0.001) when adjusting for TBW on multivariate linear regression analysis. Although the addition of a second surgeon did not proportionally reduce OT (i.e., did not afford a 50% time-savings) and may not ultimately prove cost-effective for all situations, certain patient scenarios (namely those patients with large TBW and those undergoing axillary nodal procedures) were afforded a greater time benefit and the CST may be worth considering in these cases.
Our results expand upon our initial work in which the CST was originally proposed [9]. In our original cohort of 116 patients undergoing BM with immediate reconstruction, we found a 41-min time-savings for the mastectomy portion of the procedure when done with the CST, representing a 35.1% reduction over the SST. Here, time-savings was similar, representing an adjusted overall time-savings of 44 min, or a reduction of 27.8% in a cohort of 109 patients undergoing BM without any reconstruction. Taken together, it appears consistent that the presence of a second surgeon may be able to reduce the duration of BM procedures by close to one-third. This degree of time-savings appears similar to that associated with application of the CST within other surgical subspecialties [4, 8, 12, 13].
The benefit of the CST appeared to increase with the type and extent of nodal procedure performed, with ALND affording a greater impact on time than SLNB, and bilateral procedures within both categories offering a greater impact on time than their unilateral counterparts (Table 4). These results are not surprising, and not only echo but further elaborate upon our prior work on this topic and suggest a cohort of patients in which the CST may be best suited.
Other considerations for cases best-suited for the CST include surgeon and concomitant operating room block time availability, as well as patient comfort with involving two surgeons in their care. At our institution, there are multiple breast surgeons sharing clinic and operative space making it relatively easy to find a second surgeon to operate with at any given time; however, one could imagine this coordination to be challenging in a smaller practice or one with more constraints on operative room utilization. Patients must also be comfortable with the CST in order for it to succeed, and while we have found that most patients are open to and even pleased by having two surgeons involved in their care, some patients will certainly prefer to remain with a single-surgeon approach. At our institution, the second co-surgeon usually meets the patient prior to the procedure in the preoperative holding area and not as an additional preoperative consultation.
Time-savings in the operative setting are important not only for patient outcomes, given the long accepted association between longer surgical duration and morbidity, but also with respect to operating room utilization, as operating room time is expensive [14,15,16,17]. While we have observed that the CST appears to improve operative time compared to the SST, we have also noticed that it requires additional resources that must not be overlooked when considering the financial incentives of this procedure, such as additional surgical and nursing staff and additional surgical setup. One of the potential benefits reduced operative time is a reduction in complications, a connection which has been well cited in the surgical literature [16, 18, 19]. Ultimately, however, we have found no significant difference in complication rates between the SST and CST cohorts in our analyses. It is possible that this is related to the relatively small study sizes involved and the infrequency of overall complications associated with these cases, but ultimately, a larger study is warranted to determine the final impact of the CST on patient outcomes. As was noted in a recent study investigating the role of the CST in bilateral microsurgical breast reconstructions, the financial impact of the CST on the healthcare system needs further consideration and further research into these varying financial tradeoffs is required to better understand the potential cost-effectiveness of the CST compared to the traditional SST [11].
Other benefits, as well as drawbacks, of this alternative method of BM are still unknown. Reduced work/stress for the primary surgeon, perceived improved safety/reduced complication rates, and perceived improved outcomes were cited as reasons to use two surgeons in Scheer et al’s survey of neurosurgeons performing spinal deformity surgery [20]. We are currently attempting to ascertain the utilization patterns, perceived benefits, and barriers to implementation of the CST in the wider breast surgery community with a survey we administered to the members of the American Society of Breast Surgeons designed to investigate nationwide BM practice-patterns.
There are strengths and limitations to this study. It was performed in a retrospective fashion, and only includes cases of BM performed at a single institution. In order to obtain a statistically significant sample size, the study period spans a large number of years, during which the rates for both BM procedures and nodal procedures fluctuated. We did not include patient comorbidities as part of our analysis, such as BMI or Charlson/Deyo score, for example, that could have potentially influenced operative times and/or complications. Other factors, such as influence of other providers on overall operative time (i.e., residents, fellows, surgical PAs), are also not accounted for here as we did not specifically examine their participation during data collection. While there was no surgical PA or fellow involvement during our study period, residents (mostly PGY1 or 2) may have taken part in some of these cases as an assistant. While a prior study examining the influence of resident participation on mastectomy operations concluded resident-participation usually increases mean operative time for a variety of mastectomy procedures, there was no statistically significant difference found between attending-alone and attending-with-resident bilateral mastectomy cases performed without reconstruction [21].Overall, with the incidence of BM procedures on the rise, further investigation into the CST, and into the influence of other providers on the single-surgeon versus CST operative times and outcomes, is warranted.
Conclusion
A CST for performing BM operations appears to reduce overall operative time without significantly increasing postoperative complications compared to the traditional SST. While time-savings is not directly proportional (i.e., addition of a second surgeon does not halve the operative time), benefits appear to be greater in those with larger TBWs and those requiring nodal procedures, suggesting a unique patient-cohort where the CST may be best suited. This co-surgeon model is worth further exploration as it may offer additional benefits beyond time-savings, making it an appealing alternative operative approach for certain patients.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M (2017) Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Ann Surg 265(3):581–589. https://doi.org/10.1097/SLA.0000000000001698
Kwok AC, Goodwin IA, Ying J, Agarwal JP (2015) National trends and complication rates after bilateral mastectomy and immediate breast reconstruction from 2005 to 2012. Am J Surg 210(3):512–516. https://doi.org/10.1016/j.amjsurg.2015.03.019
Tuttle TM, Abbott A, Arrington A, Rueth N (2010) The increasing use of prophylactic mastectomy in the prevention of breast cancer. Curr Oncol Rep 12(1):16–21. https://doi.org/10.1007/s11912-009-0070-y
Ludwig AT, Inampudi L, O’Donnell MA, Kreder KJ, Williams RD, Konety BR (2005) Two-surgeon versus single-surgeon radical cystectomy and urinary diversion: impact on patient outcomes and costs. Urology 65(3):488–492. https://doi.org/10.1016/j.urology.2004.10.012
Takatsuki M, Eguchi S, Yamanouchi K, Tokai H, Hidaka M, Soyama A, Miyazaki K, Hamasaki K, Tajima Y, Kanematsu T (2009) Two-surgeon technique using saline-linked electric cautery and ultrasonic surgical aspirator in living donor hepatectomy: its safety and efficacy. Am J Surg 197(2):e25-27. https://doi.org/10.1016/j.amjsurg.2008.01.019
Gomez JA, Lafage V, Scuibba DM, Bess S, Mundis GM Jr, Liabaud B, Hanstein R, Shaffrey C, Kelly M, Ames C, Smith JS, Passias PG, Errico T, Schwab F, International Spine Study Group (2017) Adult scoliosis deformity surgery: comparison of outcomes between one versus two attending surgeons. Spine (Phila Pa 1976) 42(13):992–998. https://doi.org/10.1097/BRS.0000000000002071
Kwan MK, Chiu CK, Chan CY (2017) Single vs two attending senior surgeons: assessment of intra-operative blood loss at different surgical stages of posterior spinal fusion surgery in Lenke 1 and 2 adolescent idiopathic scoliosis. Eur Spine J 26(1):155–161. https://doi.org/10.1007/s00586-016-4803-y
Aloia TA, Zorzi D, Abdalla EK, Vauthey JN (2005) Two-surgeon technique for hepatic parenchymal transection of the noncirrhotic liver using saline-linked cautery and ultrasonic dissection. Ann Surg 242(2):172–177
Mallory MA, Losk K, Camuso K, Caterson S, Nimbkar S, Golshan M (2016) Does “Two is Better Than One” apply to surgeons? Comparing single-surgeon versus co-surgeon bilateral mastectomies. Ann Surg Oncol 23(4):1111–1116. https://doi.org/10.1245/s10434-015-4956-7
Haddock NT, Kayfan S, Pezeshk RA, Teotia SS (2017) Co-surgeons in breast reconstructive microsurgery: What do they bring to the table? Microsurgery. https://doi.org/10.1002/micr.30191
Razdan SN, Panchal HJ, Hespe GE, Disa JJ, McCarthy CM, Allen RJ Jr, Dayan JH, Pusic A, Mehrara B, Cordeiro PG, Matros E (2017) The impact of the cosurgeon model on bilateral autologous breast reconstruction. J Reconstr Microsurg 33(9):624–629. https://doi.org/10.1055/s-0037-1604106
Ames CP, Barry JJ, Keshavarzi S, Dede O, Weber MH, Deviren V (2013) Perioperative outcomes and complications of pedicle subtraction osteotomy in cases with single versus two attending surgeons. Spine Deform 1(1):51–58. https://doi.org/10.1016/j.jspd.2012.10.004
Halanski MA, Elfman CM, Cassidy JA, Hassan NE, Sund SA, Noonan KJ (2013) Comparing results of posterior spine fusion in patients with AIS: are two surgeons better than one? J Orthop 10(2):54–58. https://doi.org/10.1016/j.jor.2013.03.001
Chatterjee A, Chen L, Goldenberg EA, Bae HT, Finlayson SR (2010) Opportunity cost in the evaluation of surgical innovations: a case study of laparoscopic versus open colectomy. Surg Endosc 24(5):1075–1079. https://doi.org/10.1007/s00464-009-0728-4
Daley BJ, Cecil W, Clarke PC, Cofer JB, Guillamondegui OD (2015) How slow is too slow? Correlation of operative time to complications: an analysis from the Tennessee Surgical Quality Collaborative. J Am Coll Surg 220(4):550–558. https://doi.org/10.1016/j.jamcollsurg.2014.12.040
Kim JY, Khavanin N, Rambachan A, McCarthy RJ, Mlodinow AS, De Oliveria GS Jr, Stock MC, Gust MJ, Mahvi DM (2015) Surgical duration and risk of venous thromboembolism. JAMA Surg 150(2):110–117. https://doi.org/10.1001/jamasurg.2014.1841
Macario A (2010) What does one minute of operating room time cost? J Clin Anesth 22(4):233–236. https://doi.org/10.1016/j.jclinane.2010.02.003
Procter LD, Davenport DL, Bernard AC, Zwischenberger JB (2010) General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surg 210(1):60–65, e61–62. https://doi.org/10.1016/j.jamcollsurg.2009.09.034
Nwaogu I, Yan Y, Margenthaler JA, Myckatyn TM (2015) Venous thromboembolism after breast reconstruction in patients undergoing breast surgery: an American College of Surgeons NSQIP analysis. J Am Coll Surg 220(5):886–893. https://doi.org/10.1016/j.jamcollsurg.2015.01.031
Scheer JK, Hey L, LaGrone M, Daubs M, Ames CP (2016) 343 results of the 2015 SRS survey on single versus two attending surgeon approach for adult spinal deformity surgery. Neurosurgery 63(Suppl 1):201. https://doi.org/10.1227/01.neu.0000489832.09131.d2
Chamberlain RS, Patil S, Minja EJ, Kordears K (2012) Does residents’ involvement in mastectomy cases increase operative cost? If so, who should bear the cost? J Surg Res 178:18–27. https://doi.org/10.1016/j.jss.2012.08.027
Acknowledgements
We would like to acknowledge the following individuals who contributed to making this work possible: Kristen Camuso, Fred Syllien, Kaitlyn Bifolck, Katya Losk, Linda Cutone, Ingrid Stendhal, Lawanda Dixon, Ritam Chowdhury, and William Davis.
Funding
This study was funded in part by the National Institute of Health Grant R25 CA089017 and the Breast Cancer Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
The content is solely the responsibility of the authors and does not necessarily represent the official views of Brigham and Women’s Hospital or the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Mallory, M.A., Tarabanis, C., Schneider, E. et al. Bilateral mastectomies: can a co-surgeon technique offer improvements over the single-surgeon method?. Breast Cancer Res Treat 170, 641–646 (2018). https://doi.org/10.1007/s10549-018-4794-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-018-4794-y