Abstract
Purpose
Despite benefits for patients, sustainability of breast cancer navigation programs is challenging due to the lack of reimbursement for navigators. This analysis describes distress reported by breast cancer patients to navigators and the impact of navigation on healthcare utilization for older adults with breast cancer.
Methods
We conducted a retrospective cohort study of Medicare administrative claims data and patient-reported distress assessments. The primary outcome was Medicare spending per beneficiary per quarter. Secondary outcomes included (1) the number of hospitalizations or ER visits in each quarter; (2) distress levels; and (3) causes of distress reported by patients to their navigators. A subset analysis was conducted for stage I/II/III versus stage IV patients.
Results
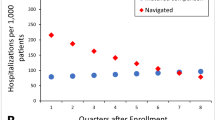
776 navigated and 776 control patients were included in the analysis. The average age at diagnosis was 74 years; 13% of the subjects were African American; 95% of patients had stage I–III. Medicare spending declined faster for the navigated group than the matched comparison group by $528 per quarter per patient (95% CL −$667, −$388). Stage I/II/III navigated patients showed a statistically significant decline in Medicare spending, ER visits, and hospitalizations over time compared to the matched comparison group. No differences were observed for stage IV patients. Eighteen percent of patients reported moderate distress. Informational and physical distress were more common in late stage than in early-stage breast cancer.
Conclusions
Lay navigation reduced healthcare utilization in older adults with breast cancer, with the greatest impact observed in early-stage breast cancer patients.



Similar content being viewed by others
References
Freeman HP (2006) Patient navigation: a community centered approach to reducing cancer mortality. J Cancer Educ 21(1 Suppl):S11–S14
Freeman HP (2013) The history, principles, and future of patient navigation: commentary. Semin Oncol Nurs 29(2):72–75
Paskett ED, Harrop JP, Wells KJ (2011) Patient navigation: an update on the state of the science. CA Cancer J Clin 61(4):237–249
Natale-Pereira A et al (2011) The role of patient navigators in eliminating health disparities. Cancer 117(15 Suppl):3543–3552
Krok-Schoen JL et al (2015) Participants’ barriers to diagnostic resolution and factors associated with needing patient navigation. Cancer 121:2757
Fouad M et al (2010) Patient navigation pilot project: results from the Community Health Advisors in Action Program (CHAAP). Ethn Dis 20(2):155–161
Post DM et al (2015) Effects of patient navigation on patient satisfaction outcomes. J Cancer Educ 30(4):728–735
Freund KM et al (2014) Impact of patient navigation on timely cancer care: the Patient Navigation Research Program. J Natl Cancer Inst 106(6):dju115
Marshall JK et al (2015) Effect of patient navigation on breast cancer screening among African American Medicare Beneficiaries: a randomized controlled trial. J Gen Intern Med 31:68
Rodday AM et al (2015) Impact of patient navigation in eliminating economic disparities in cancer care. Cancer 121(22):4025–4034
Rocque GB et al (2016) The Patient Care Connect Program: Transforming Health Care Through Lay Navigation. J Oncol Pract 12:e633
Rocque GB et al (2016) Guiding Lay Navigation in Geriatric Patients With Cancer Using a Distress Assessment Tool. J Natl Compr Canc Netw 14(4):407–414
Berenson RA, Horvath J (2003) Confronting the barriers to chronic care management in Medicare. Health Aff Suppl Web Exclusives: p. W3-37-53
Wolff JL, Starfield B, Anderson G (2002) Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med 162(20):2269–2276
Coleman EA (2003) Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 51(4):549–555
Mohile SG et al (2009) Association of a cancer diagnosis with vulnerability and frailty in older medicare beneficiaries. J Natl Cancer Inst 101(17):1206–1215
Rocque GB et al (2017) Resource use and medicare costs during lay navigation for geriatric patients with cancer. JAMA Oncol 3:817
Colligan EM et al (2017) Innovative oncology care models improve end-of-life quality, reduce utilization and spending. Health Aff 36(3):433–440
Rocque GB et al (2017) Implementation and impact of patient lay navigator-led advance care planning conversations. J Pain Symptom Manag 53(4):682–692
Harvey R, Jankus DD, Mosley D (2012) Random assignment of proxy event dates to unexposed individuals in observational studies: an automated technique using SAS®. http://www.mwsug.org/proceedings/2012/PH/MWSUG-2012-PH02.pdf
National Comprehensive Cancer Network, NCCN Guidelines: Distress Management (Version 2.2013)
Vitek L, Rosenzweig MQ, Stollings S (2007) Distress in patients with cancer: definition, assessment, and suggested interventions. Clin J Oncol Nurs 11(3):413–418
Mohile SG et al (2015) Geriatric assessment-guided care processes for older adults: a delphi consensus of geriatric oncology experts. J Natl Compr Cancer Netw 13(9):1120–1130
Wildiers H et al (2014) International society of geriatric oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol 32:2595
Klabunde CN et al (2000) Development of a comorbidity index using physician claims data. J Clin Epidemiol 53(12):1258–1267
Charlson ME et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Mariotto AB et al (2011) Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst 103(2):117–128
Murphy B, Fraeman KH (2017) A general SAS® macro to implement optimal N:1 propensity score matching within a maximum radius. http://support.sas.com/resources/papers/proceedings17/0812-2017.pdf
Hassett MJ et al (2006) Frequency and cost of chemotherapy-related serious adverse effects in a population sample of women with breast cancer. J Natl Cancer Inst 98(16):1108–1117
Schilling MB, Parks C, Deeter RG (2011) Costs and outcomes associated with hospitalized cancer patients with neutropenic complications: a retrospective study. Exp Ther Med 2(5):859–866
Dulisse B et al (2013) A retrospective study of the clinical and economic burden during hospitalizations among cancer patients with febrile neutropenia. J Med Econ 16(6):720–735
Jolly TA et al (2015) Geriatric assessment-identified deficits in older cancer patients with normal performance status. Oncologist 20(4):379–385
Hurria A et al (2012) Senior adult oncology. J Natl Compr Canc Netw 10(2):162–209
Magnuson A et al (2016) Geriatric assessment with management in cancer care: current evidence and potential mechanisms for future research. J Geriatr Oncol 7(4):242–248
Stanton AL et al (2015) Depressive episodes, symptoms, and trajectories in women recently diagnosed with breast cancer. Breast Cancer Res Treat 154(1):105–115
Deckx L et al (2015) A cohort study on the evolution of psychosocial problems in older patients with breast or colorectal cancer: comparison with younger cancer patients and older primary care patients without cancer. BMC Geriatr 15:79
Gabitova G, Burke NJ (2014) Improving healthcare empowerment through breast cancer patient navigation: a mixed methods evaluation in a safety-net setting. BMC Health Serv Res 14:407
Gunn CM et al (2014) An assessment of patient navigator activities in breast cancer patient navigation programs using a nine-principle framework. Health Serv Res 49(5):1555–1577
Balducci L, Extermann M (2000) Management of cancer in the older person: a practical approach. Oncologist 5(3):224–237
Bluethmann SM, Mariotto AB, Rowland JH (2016) Anticipating the “Silver Tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev 25(7):1029–1036
Hanchate AD et al (2010) Longitudinal patterns in survival, comorbidity, healthcare utilization and quality of care among older women following breast cancer diagnosis. J Gen Intern Med 25(10):1045–1050
Azuero A et al (2014) Co-morbidity and predictors of health status in older rural breast cancer survivors. Springerplus 3:102
Pisu M et al (2017) Out-of-pocket costs and burden among rural breast cancer survivors. Cancer Med 6(3):572–581
Acknowledgements
This work was also supported by the Centers for Medicare & Medicaid Services (CMS) (1C1CMS331023). CMS had no role in any aspect of the study or manuscript preparation and submission.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rocque, G.B., Williams, C.P., Jones, M.I. et al. Healthcare utilization, Medicare spending, and sources of patient distress identified during implementation of a lay navigation program for older patients with breast cancer. Breast Cancer Res Treat 167, 215–223 (2018). https://doi.org/10.1007/s10549-017-4498-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4498-8