Abstract
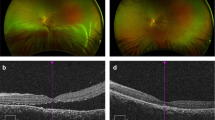
Retinal detachment is a serious vision threatening disease. Current consensus for the treatment of retinal detachment is to reattach the retina onto the choroid layer by drainage of accumulated subretinal fluid. Although several surgical methods have been developed, no satisfactory visual outcome has been obtained without surgical complications such as unintended puncture and hemorrhage of the retina and choroid tissue. In this study, we developed a novel Curved-Micro-Drainer (CMD) for the innocuous drainage of subretinal fluid. It is a curved structure with a 15° beveled tip that is 5 mm in length, with an 80 μm inner diameter and a 100 μm outer diameter. This high inner-to-outer diameter ratio of CMD with a 100 μm outer diameter allows efficient drainage of highly viscous subretinal fluid in a minimally invasive manner. In addition, the curved structure precisely matches the spherical ocular structure, which facilitates the CMD insertion into the subretinal space without choroid tissue damage. We demonstrate that the optimized CMD allows for the innocuous drainage of the viscous subretinal fluid from the porcine eye, whereas the traditional hypodermic needle (31-gauge) induces severe retinal and choroid damage. CMD can overcome a critical safety issue and is a potential alternative to conventional surgical interventions for the innocuous drainage of subretinal fluid.





Similar content being viewed by others
References
M. Angi, H. Kalirai, S. E. Coupland, B. E. Damato, F. Semeraro, M. R. Romano, Proteomic analyses of the vitreous humour. Mediat. Inflamm. (2012). doi:10.1155/2012/148039
A. Bonfiglio, R. Repetto, J.H. Siggers, A. (2013) Stocchino, investigation of the motion of a viscous fluid in the vitreous cavity induced by eye rotations and implications for drug delivery. Phys. Med. Biol. 58, 1969–1982 doi:10.1088/0031-9155/58/6/1969
R. Duval, K. A. Rezaei, Vitrectomy surgery for primary retinal detachment. Dev. Ophthalmol. 54, 174–181 (2014). doi:10.1159/000360464
L. R. Ferguson, S. Grover, J. M. Dominguez, S. Balaiya, K. V. Chalam, Retinal thickness measurement obtained with spectral domain optical coherence tomography assisted optical biopsy accurately correlates with ex vivo histology. PLoS One (2014). doi:10.1371/journal.pone.0111203
K. Kadonosono, S. Yamane, A. Arakawa, M. Inoue, T. Yamakawa, E. Uchio, et al. Endovascular cannulation with a microneedle for central retinal vein occlusion. JAMA. Ophthalmol. 6, 783–786 (2013). doi:10.1001/jamaophthalmol.2013.2585
C. Y. Lee, K. Lee, Y. S. You, S. H. Lee, H. Jung, Tower microneedle via reverse drawing lithography for innocuous intravitreal drug delivery. Adv. Healthc. Mater. (2012). doi:10.1002/adhm.201200239
C. Y. Lee, Y. S. You, S. H. Lee, H. Jung, Tower microneedle minimizes vitreal reflux in intravitreal injection. Biomed. Microdevices 15, 841–848 (2013). doi:10.1007/s10544-013-9771
C. G. Li, C. Y. Lee, K. Lee, H. Jung, An optimized hollow microneedle for minimally invasive blood extraction. Biomed. Microdevices 15, 17–25 (2013). doi:10.1007/s10544-012-9683-2
R. P. Lira, I. Takasaka, C. E. Arieta, M. A. Nascimento, R. Caldato, H. Panetta, Cryotherapy vs laser photocoagulation in scleral buckle surgery: a randomized clinical trial. Arch. Ophthalmol. 128, 1519–1522 (2013). doi:10.1001/archophthalmol.2010.271
A. Loewenstein, R.S. Rader, T.H. Shelley, E. de Juan. Jr, (1997) A flexible infusion micro-cannula for subretinal surgery. Ophthalmic Surg. Lasers Imaging 28, 774–775
Z. Lv, Y. Li, Y. Wu, Y. Qu, Surgical complications of primary rhegmatogenous retinal detachment: a meta-analysis. PLoS One (2015). doi:10.1371/journal.pone.0116493
H. Nakajima, A. Mizota, M. Tanaka, Technical note: method for estimating volume of subretinal fluid in cases of localized retinal detachment by OCT ophthalmoscopy. Ophthalmic. Physiol. Opt. 27, 512–517 (2007). doi:10.1111/j.1475-1313.2007.00507.x
V. J. Setlur, N. Rayess, S. J. Garg, J. Hsu, C. K. Luo, C. D. Regillo, M. S. Fineman, A. Sivalingam, Combined 23-gauge PPV and scleral buckle versus 23-gauge PPV alone for primary repair of Pseudophakic rhegmatogenous retinal detachment. Ophthalmic Surg. Lasers Imaging 46, 702–707 (2015). doi:10.3928/23258160-20150730-03
B. V. Stanzel, Z. Liu, R. Brinken, N. Braun, F. G. Holz, N. Eter, Subretinal delivery of ultrathin rigid-elastic cell carriers using a metallic shooter instrument and biodegradable hydrogel encapsulation. Invest. Ophthalmol. Vis. Sci. 53, 490–500 (2012). doi:10.1167/iovs.11-8260
K. Tsuchiya, N. Nakanishi, Y. Uetsuji, E. Nakamachi, Development of blood extraction system for health monitoring system. Biomed. Microdevices 7, 347–353 (2005). doi:10.1007/s10544-005-6077-8
Y. S. You, C. Y. Lee, C. Li, S. H. Lee, K. Kim, H. Jung, An arched micro-injector (ARCMI) for innocuous subretinal injection. PLoS One (2014). doi:10.1371/journal.pone.0104145
R. Zhou, H. C. Chang, Capillary penetration failure of blood suspensions. J. Colloid Interface Sci. 287, 647–656 (2005). doi:10.1016/j.jcis.2005.02.023
Acknowledgments
This work was supported by the R&D program of MSIP/COMPA (2015 K000201, Development of minimal pain multi-micro lancets for one-touch-smart diagnostic sensor) and also by grants from the Korean Health Technology R&D Project, Ministry for Health and Welfare, Republic of Korea (HI10 C1959) and the Public Welfare & Safety Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2010-0020772).
Author information
Authors and Affiliations
Corresponding author
Additional information
Yonghao Ma1 and ChangYeol Lee contributed equally to this work.
Electronic supplementary material
Figs. 1
Time of draining different volume of distilled water by 15°, 30°, 45°, and 90° bevel angle of CMD. Data are shown as mean ± SEM from three independent experiments. P < 0.05 (*) indicates significant differences compared with the control group (GIF 17 kb)
Figs. 2
The penetration force of porcine retina tissue with blunt and 15° BA of 20 μm wall thickness of CMD. Data are shown as mean ± SEM from three independent experiments. P < 0.05 (*) indicates significant differences compared with the control group (GIF 15 kb)
Rights and permissions
About this article
Cite this article
Ma, Y., Lee, C., Li, C.G. et al. Minimally invasive curved-micro-drainer (CMD) capable of innocuous drainage of subretinal fluid for the treatment of retinal detachment. Biomed Microdevices 18, 65 (2016). https://doi.org/10.1007/s10544-016-0088-5
Published:
DOI: https://doi.org/10.1007/s10544-016-0088-5