Abstract
Hip fracture is a common physical trauma in older adults that is also associated with a high incidence of new onset depression. The immune system declines with age and is also compromised by physical and psychological stress. This study examined whether hip fracture and depressive symptoms had additive effects upon the aged immune system that might contribute to poor health outcomes after hip fracture. We assessed the frequency of regulatory T cells, Tregs (CD4+ CD25+ Foxp3+) and IL10 production by CD4 T cells, and the frequency and IL10 production by regulatory B cells, Bregs (CD19+ CD24hi CD38hi) in 101 hip fracture patients (81 female) 6 weeks after injury and 43 healthy age-matched controls (28 female). 38 hip fracture patients (37 %) developed depressive symptoms. Hip fracture did not have an effect on circulating Tregs frequency but a significant reduction in the frequency of Bregs was observed in patients who developed depression compared with non-depressed patients (p = 0.001) or healthy controls (p < 0.001). Bregs also showed a significant decline in IL10 production in depressed hip fracture patients compared with controls (p = 0.04) and non-depressed patients (p = 0.01). In contrast, there was an increase in IL10 production by CD4 T cells in hip fracture patients with new onset depression compared to hip fracture patients without depression (p = .04) and healthy controls (p = .02). We conclude that the reduced immunity associated with new onset depression post hip fracture could include a contribution by heightened Tregs function.
Similar content being viewed by others
Introduction
Hip fracture is a common and devastating injury and a major health issue in old age (Abrahamsen et al. 2009). 1 in 3 adults aged 65 years and over fall each year and in the UK alone this results in approximately 75,000 hip fractures each year. Hip fracture is a frequent cause of institutionalisation and has a 1 year mortality of approximately 25 % (Panula et al. 2011) with infections a major cause of morbidity and mortality in this patient group (Edwards et al. 2008). The reasons for such poor outcomes in this trauma population are multifactorial but include co-morbidities (Edwards et al. 2008; Panula et al. 2011), reduced immunity (Butcher et al. 2005) and the consequences of depression (Phillips et al. 2013). Healthy older individuals have been reported to experience greater levels of stress, anxiousness and depression than young adults (Luz et al. 2003). Stressful life events such as bereavement or a disabling medical event are amongst the most potent factors that can trigger depressive symptoms (Cole and Dendukuri 2003). Therefore, it is perhaps not surprising that a high rate of depression (9–47 %) has been reported in studies of older adults with hip fracture (Holmes and House 2000). Importantly, depression in hip fracture patients has been associated with increased risk of infections and poor survival (Nightingale et al. 2001), impaired recovery and a retarded ability to regain pre-fracture levels of physical functioning (Mossey et al. 1990).
It is well documented that ageing is accompanied by immune decline, termed immunesenescence, which contributes to increased susceptibility to infections in older adults (Dorshkind et al. 2009; Panda et al. 2009). However the immune system does not act in isolation and is profoundly affected by both physical and psychological stress (Butcher and Lord 2004; Segerstrom and Miller 2004). Importantly, there is accumulating evidence suggesting that the effects of stress and age are interactive, with chronic stress exacerbating the effects of ageing in older adults (Kiecolt-Glaser and Glaser 1999). In this study we set out to test the hypothesis that psychological stress, specifically depressive symptoms, would act additively with the physical stress of hip fracture to amplify the effect of ageing upon immunity. We have reported previously that after hip fracture the function of innate immune cells (neutrophils, NK cells and monocytes) was significantly suppressed but only in the patients who developed depression (Duggal et al. 2013a, 2014, 2015). Here we extend the investigation to consider the regulatory cells of the immune system that are central to immune homeostasis, in order to determine if over activity in this arm of the immune response to injury could account for reduced immunity and increased susceptibility to infections after hip fracture.
Once activated it is essential to modulate the immune response to prevent unintended harmful effects arising from the defensive actions of immune cells. Regulatory CD4+CD25+Foxp3+ T cells play a pivotal role in maintaining immune homeostasis by suppressing immune responses (Wing and Sakaguchi 2010). Tregs suppressive function is mediated via production of immunosuppressive cytokines, such as IL10 (Hara et al. 2001), TGFβ (Oida et al. 2003) and via cell–cell contact (Stephens et al. 2001). An age associated increase in the frequency of Tregs has been reported in mice (Kozlowska et al. 2007; Zhao et al. 2007) and humans (Gregg et al. 2005). However, concomitant impairment in the immunosuppressive function of CD4+ Tregs has been shown in aged mice (Zhao et al. 2007) and humans (Tsaknaridis et al. 2003), though the literature is inconsistent with other studies reporting intact Tregs suppressive function with age (Gregg et al. 2005; Lages et al. 2008). More recently, a subset of B cells has been shown to be able to suppress inflammation (Wolf et al. 1996). In humans, CD19+ CD24hi CD38hi immature transitional B cells exhibit immunosuppressive properties, mainly via IL10 production on stimulation via CD40 or the TLR pathway (Blair et al. 2010; Duggal et al. 2013b). These IL10 producing B cells restrain inflammatory Th1 and Th17 cells and maintain Treg numbers (Carter et al. 2012; 2011). Tedder and co-workers have also reported the existence of a CD19+ CD5+ CD1dhi B cell subset, designated as B10 cells that can exert immunosuppressive effects in a IL10 dependent manner (Yanaba et al. 2008). Recently on investigating regulatory function in healthy older adults we reported both numerical and functional impairments (reduced IL10 production) in CD19+ CD24hi CD38hi Bregs with advancing age (Duggal et al. 2013b) .
Here we investigated the impact of hip fracture and new onset depressive symptoms on the frequency and function of Tregs and CD19+ CD24hi CD38hi B cells.
Materials and methods
Study participants
101 older hip fracture patients were recruited from five hospitals in Birmingham, UK between 2010 and 2012. Inclusion criteria were that participants had to be aged 60 years and over with a hip fracture sustained 4–6 weeks previously but with no chronic immune-related disorders or taking any regular medications that might modify immunity. Additionally patients must not have had any diagnosis of depression by a physician prior to age 50 years or be taking or have previously taken anti-depressant medication. 43 healthy older adults were also recruited from the community as controls. These controls also had to meet the inclusion criteria above but not have had a hip fracture. The study was approved by South Birmingham Local Research Ethics Committee and all participants provided written informed consent (study ref: 09/H1203/80).
Study design and procedure
The study was a prospective case–control design with three groups of older adults: hip fracture patients with or without depressive symptoms and healthy older adults. Consent was gained whilst patients were still in hospital. All patients provided a blood sample and completed questionnaires and structured interviews 4-6 weeks after hip fracture. Control participants attended the University, for one-off blood sampling and completed questionnaires. None of the participants had an acute infection at the time of blood sampling.
Assessment for depressive symptoms
Standard socio-demographic and health behaviour information were taken and all comorbidities and medications, prescription and over-the-counter, were recorded by the interviewer. The psychological status of the participant was assessed by a Geriatric Depression Scale (GDS) (Yesavage et al. 1982). Depression was defined as a GDS score greater than or equal to six. The Hospital Anxiety and Depression Scale (HADS) was also used to measure depression and anxiety (Zigmond and Snaith 1983). Healthy control participants completed the HADS depression sub-scale in order to check that they did not have significant depressive symptoms.
Foxp3 staining for identification of Tregs
Peripheral blood mononuclear cells (PBMCs) were isolated by density centrifugation using Ficoll-Paque™ PLUS (GE Healthcare, Sweden). Isolated PBMCs were resuspended in phosphate buffered saline (PBS) at a concentration of 1 × 106/ml and were stained with anti-human CD3-PEcy7 (eBiosciences, UK; clone: UCHT1), anti-human CD4 Alexa fluor 450 (eBiosciences, UK; clone: RPA-T4) and anti-human CD25 APC (Biolegend, UK; clone: BC96) antibodies for 20 min in the dark at 4 °C. Post incubation, cells were washed with PBS and re-suspended in Foxp3 Fix Perm Working solution (eBiosciences, UK) and incubated for 30 min in the dark at room temperature. Post incubation, cells were washed and resuspended in Foxp3 Permeabilization buffer (eBiosciences, UK) and stained with anti-human Foxp3 PE antibody (eBiosciences, UK) for 30 min in the dark at room temperature. Finally, the cells were washed and resuspended in PBS for flow cytometric analysis using a Cyan ™ ADP (Dako Ltd, UK). The percentage of CD3+ CD4+ CD25+ Foxp3+ T cells were recorded.
Stimulation of PBMCs to induce IL10 production by CD4 T cells
Cell cultures were performed in RPMI 1640 (Sigma Aldrich, UK) containing 10 % FCS (Biosera, UK) supplemented with glutamine/penicillin/streptomycin (Life Technologies, UK). PBMCs (1 × 106/ml) were stimulated for 4 h with PMA (50 ng/ml; Sigma Aldrich, UK) and Ionomycin (500 ng/ml; Sigma Aldrich, UK) in the presence of Brefeldin A (10 μg/ml; Sigma Aldrich, UK). Post stimulation, cells were washed twice with PBS and stained using anti-human CD3 PEcy7 (eBiosciences, UK; clone: UCHT1) and anti-human CD4 Alexa fluor 450 (eBiosciences, UK; clone: RPA-T4) for 20 min in the dark at 4 °C. Cells were washed and fixed with Reagent A (Fix and Perm kit, Invitrogen, UK) for 30 min in the dark at room temperature. Post incubation, cells were washed and re-suspended in Reagent B (Fix and Perm kit, Invitrogen, UK) and anti-human Alexa fluor 647 IL10 antibody (clone: JES3-9D7) was added to cells that were incubated in the dark at room temperature for 30 min. After washing the cells were resuspended in PBS and analysed on a Cyan ™ ADP (Dako Ltd, UK) and the percentage of CD3+ CD4+ IL10+ T cells and IL10 expression levels (MFI value) by CD4 T cells was recorded.
Identification of immunosuppressive CD19+CD24hiCD38hi B cells
Isolated PBMCs (1 × 106/ml) were stained with a combination of fluorochrome conjugated antibodies including; CD19-PE (eBiosciences, clone: HIB19), CD24-FITC (eBiosciences, clone: eBioSN3), CD38-PEcy7 (eBiosciences, clone: HIT2), antibodies for 20 min in dark at 4 °C. Post incubation, the cells were washed and resuspended in PBS for flow cytometric analysis using Cyan ™ ADP (Dako Ltd, UK). The percentage of CD24hi CD38hi CD19+ B cells was recorded.
CD3 stimulation of PBMCs to induce IL10 production by CD19+CD24hiCD38hi B cells
96 well microtitre plates with round bottom wells (Sarstedt Ltd, Leicester, UK) were coated with anti-CD3 mAb (BD Biosciences) at a concentration of 0.5 μg/ml for 1 h at 37 °C. Isolated PBMCs were plated at 25 × 104 cells/well for 72 h at 37 °C in a humidified atmosphere of 5 % CO2 and Brefeldin A (10 μg/ml; Sigma-Aldrich) was added during the last 6 h of the incubation. After culturing cells with stimulus they were washed and stained for a combination of extracellular surface markers to identify IL10 producing CD24hi CD38hi CD19+ B cells. Post immunostaining, cells were fixed, permeabilised and stained with anti-human Alexa fluor 647 IL10 antibody (described in “Stimulation of PBMCs to induce IL10 production by CD4 T cells” section). Post immunostaining, cells were washed and resuspended in PBS and analysed on a Cyan ™ ADP (Dako Ltd, UK). The percentage of IL10+ CD24hi CD38hi CD19+ B cells and IL10 expression levels (MFI value) by CD24hi CD38hi CD19+ B cells was recorded.
T cell independent (LPS) stimulation of PBMCs to induce IL10 production by CD19+CD24hiCD38hi B cells
Isolated PBMCs were plated at 25 × 104 cells/well in a 96 well microtitre plates with round bottom wells (Sarstedt Ltd, UK) in the presence of LPS isolated from Escherichia coli serotype 0111:B4 (1 µg/ml; Peprotech, UK) for 72 h at 37 °C in a humidified atmosphere of 5 % CO2. Brefeldin A (10 μg/ml; Sigma-Aldrich, UK) was added during the last 6 h of the incubation. After culturing cells with stimulus they were washed and stained for a combination of extracellular surface markers to identify IL10 producing CD24hi CD38hi CD19+ B cells. Post immunostaining, cells were fixed, permeabilised and stained with anti-human Alexa fluor 647 IL10 antibody (described in “Stimulation of PBMCs to induce IL10 production by CD4 T cells” section). Post immunostaining, cells were washed and resuspended in PBS and analysed on a Cyan ™ ADP (Dako Ltd, UK). The percentage of IL10+ CD24hi CD38hi CD19+ B cells and IL10 expression levels (MFI value) by CD24hi CD38hi CD19+ B cells was recorded.
Serum cortisol assay
Serum cortisol levels were measured by ELISA using a commercial kit (IBL international, Hamburg, Germany) according to manufacturer’s instructions. Intra assay coefficients of variation (CV %) were 6.7.
Statistical analysis
Univariate ANOVA with least significant difference post hoc tests were used to assess differences between the three groups (hip fracture with depressive symptoms, hip fracture without depressive symptoms and healthy controls). Where demographic variables differed significantly between the three groups analyses were rerun adjusting for these variables using ANCOVA. Pearson’s correlations were used to examine associations between depression score, serum cortisol levels and T and B cell phenotype and IL10 production.
Results
The demographic details of the study participants have been reported in full previously (Phillips et al. 2013).
Regulatory T cells in hip fracture patients
Tregs have been defined by the expression of CD4, CD25 and the transcription factor foxp3 (Buckner 2010; O’Garra and Vieira 2004). On examining the circulating frequency of CD4+ CD25+ Foxp3+ T cells no significant differences were observed between hip fracture patients with and without depressive symptoms and healthy older adults, F(2, 57) = 1.24, p = .29, η2 = .04 (Fig. 1a). Similarly, no significant differences were found between absolute numbers of regulatory T cells, F (2, 31) = .98, p = .38, η2 = 06 (Fig. 1b) between our three subject groups.
CD4+ CD25+ Foxp3+ regulatory T lymphocytes in hip fracture patients. a Percentage of CD4+ CD25+ Foxp3+ T cells in healthy controls (n = 20), hip fracture patients without depressive symptoms (HF; n = 20) and hip fracture patients with depressive symptoms (HF + D; n = 20). The solid bar represents the mean value. b Absolute number of CD4+ CD25+ Foxp3+ regulatory T cells in healthy controls (n = 12), hip fracture patients without depressive symptoms (HF; n = 13) and hip fracture patients with depressive symptoms (HF + D; n = 10). Data are mean ± SEM
IL10 production by CD4 T cells in hip fracture patients
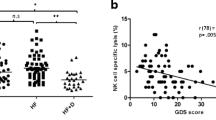
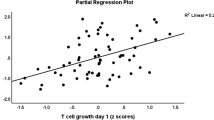
IL10 secretion is one of the main mechanisms of immunosuppression used by Tregs (Roncarolo et al. 2006). In this study, IL10 production by CD4 T cells upon stimulation with PMA and Ionomycin was measured. Significant differences were seen in the percentage of IL10 producing CD4 T cells between our three groups, F (2, 50) = 4.93, p = .01, η2 = .16 (Fig. 2a), driven by a significant increase in the percentage of IL10+ CD4 T cells in hip fracture patients with depressive symptoms compared with hip fracture patients without depressive symptoms, p = .04 and healthy controls, p = .02. No significant differences were observed in the amount of IL10 expressed (MFI value) by CD4 T cells between our groups, F(2, 42) = .46, p = .63, η2 = .02 (Fig. 2b). Interestingly, there was a significant association between GDS scores and the frequency of peripheral IL10+ CD4 T cells in hip fracture patients, β = .34, p = .04, ΔR2 = .11, such that hip fracture patients with greater depressive symptoms (GDS score) had a higher frequency of IL10+ CD4 T cells (Fig. 2c).
IL10 production by CD4 T lymphocytes in hip fracture patients. a Percentage IL10+ CD4 T cells and b mean IL10 production (MFI value) by CD4 T cells in healthy controls (n = 17), hip fracture patients without depressive symptoms (HF; n = 16) or hip fracture patients with depressive symptoms (HF+D; n = 21). The solid bar represents the mean value in (a) and data are mean ± SEM in (b). c Correlation between GDS depression scores and IL10 production by CD4 T cells in hip fracture patients (n = 36). *p < 0.05
Frequency of CD19+ CD24hi CD38hi B cells in hip fracture patients
Three major populations of circulating B cells have been reported in peripheral blood: transitional, circulating mature naïve and memory B cells discriminated on the basis of relative distribution of developmentally regulated markers CD24 and CD38 (Sims et al. 2005). The gating strategy used to identify CD19+ CD24hi CD38hi B cells has been reported previously (Duggal et al. 2013b). On assessing the peripheral frequency and absolute numbers of B cells no differences were observed between hip fracture patients with and without depression and healthy controls (data not shown), which is in agreement with other reports of unaltered circulating B cell numbers in depressed individuals (Basterzi et al. 2010). However the frequency of CD19+CD24hiCD38hi B cells in the B cell pool differed between our three groups, F(2, 61) = 11.16, p < .001, η2 = .26 (Fig. 3a), due to a decline in this subset in hip fracture patients with depressive symptoms compared with healthy controls, p < .001 as well as hip fracture patients without depressive symptoms, p = .001. When all of the above analyses were repeated with adjustment for age, sex and BMI, the results still remained significant (data not shown).
Frequency of CD19+CD24hiCD38hi B cells in hip fracture patients. a Percentage and b absolute numbers of CD19+CD24hiCD38hi cells in healthy controls (n = 21), hip fracture patients without depressive symptoms (HF; n = 15) and hip fracture patients with depressive symptoms (HF + D; n = 22). The solid bar represents the mean value in (a) and the data are mean ± SEM in (b). c Correlation between percentage of CD19+CD24hiCD38hi and GDS scores in hip fracture patients (n = 36). *p < 0.05, **p < 0.005 and ***p < 0.001
Similarly, significant differences were seen in absolute numbers of CD19+CD24hiCD38hi B cells, F (2, 38) = 4.85, p = .01, η2 = .20 (Fig. 3b) between our three groups, driven by a significant decline in absolute numbers in hip fracture patients with depressive symptoms compared with healthy controls, p = .04 as well as hip fracture patients without depressive symptoms, p = .02. A significant association was observed between GDS scores and frequency of peripheral CD19+CD24hiCD38hi B cells in hip fracture patients, β = −0.38, p = 0.01, ΔR2 = 0.15, such that hip fracture patients with greater depressive symptoms (GDS score) had lower frequency of CD19+CD24hiCD38hi B cells (Fig. 3c).
IL10 production by CD19+ CD24hi CD38hi B cells in hip fracture patients
The hallmark of CD19+ CD24hi CD38hi B cell suppressive function is their ability to produce IL10 (Vitale et al. 2010). CD40 is a co-stimulatory molecule known to be involved in T cell mediated B cell activation (Castigli et al. 1994) known to upregulate IL10 production (Mauri et al. 2003). We have previously reported that CD19+ CD24hi CD38hi B cells are the main IL10 producing B cell subset post CD40 stimulation (Duggal et al. 2013b). Thus, the frequency of IL10 producing CD19+CD24hiCD38hi B cells post CD3 stimulation (72 h) was determined. The data revealed significant differences between our groups, F (2, 55) = 4.88, p = .01, η2 = .15, but the reduction in IL10 induction was restricted to hip fracture patients with depressive symptoms compared with healthy controls, p = .04 and hip fracture patients without depression, p = .01 (Fig. 4a). When all of the above analyses were repeated with adjustment for age, sex and BMI, the results still remained significant (data not shown). However, the mean IL10 production by CD19+CD24hiCD38hi B cells post stimulation did not differ between the subject groups, F(2, 55) = 0.85, p = 0.43, η2 = 0.03 (Fig. 4b).
IL10 production by CD19+CD24hiCD38hi B cells in hip fracture patients. a Frequency of IL10+CD19+CD24hiCD38hi cells in healthy controls (n = 18), hip fracture patients without depressive symptoms (HF; n = 21) or hip fracture patients with depressive symptoms (HF+D; n = 19). The solid bar represents the mean value. b IL10 production by CD19+CD24hiCD38hi cells in healthy controls (n = 18), hip fracture patients without depressive symptoms (HF; n = 21) or hip fracture patients with depressive symptoms (HF+D; n = 19) post CD3 stimulation for 72 h. Data are mean ± SEM. c Correlation between percentage of IL10+CD19+CD24hiCD38hi B cells post CD3 stimulation (72 h) and GDS scores in hip fracture patients (n = 40). d IL10 production by CD19+CD24hiCD38hi cells in healthy controls (n = 24), hip fracture patients without depressive symptoms (HF; n = 26) or hip fracture patients with depressive symptoms (HF+D; n = 22) post LPS stimulation for 72 h. *p < 0.05
There was a significant association between GDS scores and the frequency of IL10 producing CD19+CD24hiCD38hi B cells post stimulation in hip fracture patients, β = −0.34, p = .03, ΔR2 = 0.34, such that hip fracture patients with greater depressive symptoms (GDS score) had a lower frequency of CD19+CD24hiCD38hi B cells (Fig. 4c).
In addition to T cell-dependent stimulation, B cells can also be activated by microbial products via Toll-like receptor (TLR) signalling (Yanaba et al. 2009). In a previous study we showed that CD19+ CD24hi CD38hi B cells are the main IL10 producing B cell subset post TLR4 ligand (LPS) stimulation (Duggal et al 2013b). On examining IL10 production by CD19+ CD24hi CD38hi B cells on stimulation by LPS no significant differences were observed between our groups, F(2, 41) = 2.03, p = .14, η2 = .43 (Fig. 4d), although a trend towards a decline in IL10 production by Bregs was observed in hip fracture patients with depressive symptoms.
Serum cortisol and regulatory immune cell parameters
We have previously reported elevated serum cortisol levels in the hip fracture patients with depressive symptoms compared with patients with hip fracture alone and healthy controls []. However, there was no significant association between serum cortisol levels and IL10 producing CD4 T cells in hip fracture patients, β = −0.10, p = 0.49, ΔR2 = 0.02 (Fig. 5a). Further, there was no significant association between serum cortisol levels and IL10 producing CD19+CD24hiCD38hi B cells in hip fracture patients, β = −0.15, p = 0.28, ΔR2 = 0.02 (Fig. 5b). When all of the above analyses were repeated with adjustment for age and BMI, the results remained the same.
Discussion
A high incidence of depression has been observed after hip fracture by many studies and was seen in approximately one-third of our hip fracture patients at 6 weeks post-surgery, which is consistent with previous studies (Holmes and House 2000; Lenze et al. 2007). Although mood disorders, especially depression, have been well studied in older patients with fractured neck of femur (Holmes and House 2000; Lenze et al. 2007), the effects of depressive symptoms on immune functioning are less well studied or appreciated in the clinical context. We have recently published that neutrophil bactericidal properties (Duggal et al. 2013a), monocyte (Duggal et al. 2014) and NK cell functioning (Duggal et al. 2015) are impaired only in those hip fracture patients that developed depressive symptoms. We have also shown that new onset of depressive symptoms is associated with poor physical recovery after hip fracture (Phillips et al. 2013). Here we have now shown the effects of chronic stress (hip fracture and depression) on two regulatory immune cell subsets; CD4+CD25+Foxp3+ (Tregs) and CD19+CD24hiCD38hi (Bregs) and again find that depressive symptoms are the factor determining the immune alterations.
Firstly, on examining the effect of hip fracture and depressive symptoms on Tregs, no significant differences were observed in the frequency of circulating CD4+CD25+Foxp3+ Tregs, which contradicts the findings of two previous studies showing a decline in Tregs in mice with depression-like behaviour (Kim et al. 2012) and in humans with major depression (Li et al. 2010). Furthermore, another study has shown that anti-depressant therapy increased Treg numbers and this was associated with a reduction in depression and reduced serum pro-inflammatory cytokines which have a role in the pathophysiology of depression (Himmerich et al. 2010). One possible explanation of this contradiction might be heterogeneity in Treg characterisation, the three previous studies classified CD4+ CD25+ T cells as Tregs, rather than the more accurate CD4+ CD25+ Foxp3+ phenotype and many of these cells would have been CD25 expressing activated T cells rather than Foxp3 expressing immunosuppressive Tregs. The regulatory function of Tregs is known to be mediated via immunosuppressive cytokines such as IL10 (Vignali et al. 2008). IL10 is an immunoregulatory cytokine that plays a central role in controlling inflammation by suppressing T cell proliferation and cytokine production, antigen presentation and proinflammatory cytokine production by monocytes (Moore et al. 2001). We have previously reported higher circulating levels of IL10 in hip fracture patients with new onset of depression (22.41 ± 6.46 pg/ml) compared with hip fracture patients without depression (10.37 ± 2.25 pg/ml) or healthy controls (5.27 ± 1.11 pg/ml) (Duggal et al. 2013a) and here we show a marked increase in IL10 production by CD4 T cells of hip fracture patients with depressive symptoms compared to healthy controls. These data suggest that this is likely to account for the raised IL10 seen in these patients and may contribute to the reduced function of a variety of immune cells seen after hip fracture. Interestingly, a significant positive association was also found between GDS scores and IL10 production by CD4 T cells. Although this is the first study to examine the effect of hip fracture and depression on IL10 production by CD4+ T cells, a few studies examining the effect of chronic stress such as caregiving (Damjanovic et al. 2007; Glaser et al. 2001) and academic stress (Koh et al. 2008) have reported increased IL10 production and secretion. Whether the raised IL10 production is a response to the inflammation associated with depression in our cohort, we found raised IL6 and TNFα only in the hip fracture patients who developed depressive symptoms (Duggal et al. 2013a), remains to be shown but is one possibility. HPA axis hyperactivity is one of the most recognised findings in depressed patients (Gold et al. 1988). In-vitro studies have shown that glucocorticoids enhance IL10 production by CD4 T cells (Franchimont 2004; Richards et al. 2000). We have previously reported elevated serum cortisol levels in hip fracture patients with depressive symptoms (Duggal et al. 2013a). However, we failed to find any association between frequency of IL10+ CD4 T cells and serum cortisol levels in hip fracture patients.
Recently Bregs have attracted increasing attention for the important role of these cells in maintaining immune homeostasis. Studies on Bregs in humans are still limited and our study is the first to examine the effects of ageing and chronic stress on these immunosuppressive cells. We have previously reported a numerical deficit in CD19+CD24hiCD38hi B cells with advancing age. In this study on examining the additive effect of chronic stress on this age associated numerical deficit we report a further reduction in the frequency of Bregs (CD19+CD24hiCD38hi) in hip fracture patients with depressive symptoms. In addition we also found impairments in immunosuppressive properties of these cells with age (Duggal et al. 2013b) and here we show an additional decline in IL10 production upon CD3 stimulation in hip fracture patients with depressive symptoms. Again to the best of our knowledge this is the first study to examine the effect of psychological stress on IL10 production by B cells. However, these data are surprising when considered together with the increased IL10 production by CD4 T cells shown here and the overall raised serum IL10 reported in these patients previously (Duggal et al. 2013a). Although the effect of glucocorticoids on Bregs remains unexplored, we failed to find any association between frequencies of IL10+ Bregs and serum cortisol levels in hip fracture patients.
From these data we have to conclude that the increased frequency and function of the Treg population dominates in these patients and contributes to the reduced function seen in a variety of immune cells in these patients (Duggal et al. 2013a, 2015).
Conclusion
In conclusion, the present study reports for the first time that development of new onset depressive symptoms in older hip fracture patients results in numerical and functional deficits in Bregs but an increase in IL10 production by CD4 T cells. These findings suggest that impairments in T regulatory immune cells might be a contributing factor towards immune suppression in hip fracture patients with depressive symptoms and our data support the need for early prevention and treatment of depression in older hip fracture patients.
References
Abrahamsen B et al (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650. doi:10.1007/s00198-009-0920-3
Basterzi AD et al (2010) Effects of venlafaxine and fluoxetine on lymphocyte subsets in patients with major depressive disorder: a flow cytometric analysis. Prog Neuropsychopharmacol Biol Psychiatry 34:70–75. doi:10.1016/j.pnpbp.2009.09.025
Blair PA et al (2010) CD19(+)CD24(hi)CD38(hi) B cells exhibit regulatory capacity in healthy individuals but are functionally impaired in systemic lupus erythematosus patients. Immunity 32:129–140. doi:10.1016/j.immuni.2009.11.009
Buckner JH (2010) Mechanisms of impaired regulation by CD4(+)CD25(+)FOXP3(+) regulatory T cells in human autoimmune diseases. Nat Rev Immunol 10:849–859. doi:10.1038/nri2889
Butcher SK, Lord JM (2004) Stress responses and innate immunity: aging as a contributory factor. Aging Cell 3:151–160
Butcher SK et al (2005) Raised cortisol:dHEAS ratios in the elderly after injury: potential impact upon neutrophil function and immunity. Aging Cell 4:319–324
Carter NA et al (2011) Mice lacking endogenous IL-10-producing regulatory B cells develop exacerbated disease and present with an increased frequency of Th1/Th17 but a decrease in regulatory T cells. J Immunol 186:5569–5579. doi:10.4049/jimmunol.1100284
Carter NA, Rosser EC, Mauri C (2012) Interleukin-10 produced by B cells is crucial for the suppression of Th17/Th1 responses, induction of T regulatory type 1 cells and reduction of collagen-induced arthritis. Arthritis Res Ther 14:R32. doi:10.1186/ar3736
Castigli E et al (1994) CD40-deficient mice generated by recombination-activating gene-2-deficient blastocyst complementation. Proc Natl Acad Sci USA 91:12135–12139
Cole MG, Dendukuri N (2003) Risk factors for depression among elderly community subjects: a systematic review and meta-analysis. Am J Psychiatry 160:1147–1156
Damjanovic AK et al (2007) Accelerated telomere erosion is associated with a declining immune function of caregivers of Alzheimer’s disease patients. J Immunol 179:4249–4254
Dorshkind K, Montecino-Rodriguez E, Signer RA (2009) The ageing immune system: is it ever too old to become young again? Nat Rev Immunol 9:57–62. doi:10.1038/nri2471
Duggal NA et al (2013a) Depressive symptoms are associated with reduced neutrophil function in hip fracture patients. Brain Behav Immun 33:173–182. doi:10.1016/j.bbi.2013.07.004
Duggal NA et al (2013b) An age-related numerical and functional deficit in CD19 CD24 CD38 B cells is associated with an increase in systemic autoimmunity. Aging Cell 12(5):873–881. doi:10.1111/acel.12114
Duggal NA et al (2014) Depressive symptoms in hip fracture patients are associated with reduced monocyte superoxide production. Exp Gerontol 54:27–34. doi:10.1016/j.exger.2014.01.028
Duggal NA et al (2015) NK cell immunesenescence is increased by psychological but not physical stress in older adults associated with raised cortisol and reduced perforin expression. Age (Dordr) 37:9748. doi:10.1007/s11357-015-9748-2
Edwards C, Counsell A, Boulton C, Moran CG (2008) Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg Br 90:770–777. doi:10.1302/0301-620X.90B6.20194
Richards DF, Fernandez M, Caulfield J, Hawrylowicz CM (2000) Glucocorticoids drive human CD8(+) T cell differentiation towards a phenotype with high IL-10 and reduced IL-4, IL-5 and IL-13 production. Eur J Immunol 30:2344–2354
Franchimont D (2004) Overview of the actions of glucocorticoids on the immune response: a good model to characterize new pathways of immunosuppression for new treatment strategies. Ann N Y Acad Sci 1024:124–137
Glaser R et al (2001) Evidence for a shift in the Th-1 to Th-2 cytokine response associated with chronic stress and aging. J Gerontol A Biol Sci Med Sci 56:M477–M482
Gold PW, Goodwin FK, Chrousos GP (1988) Clinical and biochemical manifestations of depression. Relation to the neurobiology of stress (1). N Engl J Med 319:348–353
Gregg R et al (2005) The number of human peripheral blood CD4+CD25high regulatory T cells increases with age. Clin Exp Immunol 140:540–546
Hara M et al (2001) IL-10 is required for regulatory T cells to mediate tolerance to alloantigens in vivo. J Immunol 166:3789–3796
Himmerich H, Milenovic S, Fulda S, Plumakers B, Sheldrick AJ, Michel TM, Kircher T, Rink L (2010) Regulatory T cells increased while Il-1 beta decreased during antidepressant therapy. J Psyhciatr Res 44:1052–1057
Holmes JD, House AO (2000) Psychiatric illness in hip fracture. Age Ageing 29:537–546
Kiecolt-Glaser JK, Glaser R (1999) Chronic stress and mortality among older adults. JAMA 282:2259–2260
Kim SJ et al (2012) CD4+CD25 + regulatory T cell depletion modulates anxiety and depression-like behaviors in mice. PLoS One 7:e42054. doi:10.1371/journal.pone.0042054
Koh KB et al (2008) Counter-stress effects of relaxation on proinflammatory and anti-inflammatory cytokines. Brain Behav Immun 2:1130–1137. doi:10.1016/j.bbi.2008.06.009
Kozlowska E, Biernacka M, Ciechomska M, Drela N (2007) Age-related changes in the occurrence and characteristics of thymic CD4(+) CD25(+) T cells in mice. Immunology 122:445–453
Lages CS et al (2008) Functional regulatory T cells accumulate in aged hosts and promote chronic infectious disease reactivation. J Immunol 181:1835–1848
Lenze EJ et al (2007) Onset of depression in elderly persons after hip fracture: implications for prevention and early intervention of late-life depression. J Am Geriatr Soc 55:81–86
Li Y et al (2010) Altered expression of CD4(+)CD25(+) regulatory T cells and its 5-HT(1a) receptor in patients with major depression disorder. J Affect Disord 124:68–75. doi:10.1016/j.jad.2009.10.018
Luz C et al (2003) Impact of psychological and endocrine factors on cytokine production of healthy elderly people. Mech Ageing Dev 124:887–895
Mauri C, Gray D, Mushtaq N, Londei M (2003) Prevention of arthritis by interleukin 10-producing B cells. J Exp Med 197:489–501
Moore KW, de Waal Malefyt R, Coffman RL, O’Garra A (2001) Interleukin-10 and the interleukin-10 receptor. Annu Rev Immunol 19:683–765
Mossey JM, Knott K, Craik R (1990) The effects of persistent depressive symptoms on hip fracture recovery. J Gerontol 45:M163–M168
Stephens LA, Mottet C, Mason D, Powrie F (2001) Human CD4(+)CD25(+) thymocytes and peripheral T cells have immune suppressive activity in vitro. Eur J Immunol 31:1247–1254
Nightingale S, Holmes J, Mason J, House A (2001) Psychiatric illness and mortality after hip fracture. Lancet 357:1264–1265
O’Garra A, Vieira P (2004) Regulatory T cells and mechanisms of immune system control. Nat Med 10:801–805
Oida T et al (2003) CD4+CD25- T cells that express latency-associated peptide on the surface suppress CD4+CD45RBhigh-induced colitis by a TGF-beta-dependent mechanism. J Immunol 170:2516–2522
Panda A et al (2009) Human innate immunosenescence: causes and consequences for immunity in old age. Trends Immunol 30:325–333. doi:10.1016/j.it.2009.05.004
Panula J et al (2011) Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord 12:105. doi:10.1186/1471-2474-12-105
Phillips AC et al (2013) Depression following hip fracture is associated with increased physical frailty in older adults: the role of the cortisol: dehydroepiandrosterone sulphate ratio. BMC Geriatr 13:60. doi:10.1186/1471-2318-13-60
Roncarolo MG et al (2006) Interleukin-10-secreting type 1 regulatory T cells in rodents and humans. Immunol Rev 212:28–50
Segerstrom SC, Miller GE (2004) Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull 130:601–630
Sims GP et al (2005) Identification and characterization of circulating human transitional B cells. Blood 105:4390–4398
Tsaknaridis L et al (2003) Functional assay for human CD4+CD25+ Treg cells reveals an age-dependent loss of suppressive activity. J Neurosci Res 74:296–308
Vignali DA, Collison LW, Workman CJ (2008) How regulatory T cells work. Nat Rev Immunol 8:523–532. doi:10.1038/nri2343
Vitale G, Mion F, Pucillo C (2010) Regulatory B cells: evidence, developmental origin and population diversity. Mol Immunol 48:1–8. doi:10.1016/j.molimm.2010.09.010
Wing K, Sakaguchi S (2010) Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol 11:7–13. doi:10.1038/ni.1818
Wolf SD, Dittel BN, Hardardottir F, Janeway CA (1996) Experimental autoimmune encephalomyelitis induction in genetically B cell-deficient mice. J Exp Med 184:2271–2278
Yanaba K et al (2008) A regulatory B cell subset with a unique CD1dhiCD5 + phenotype controls T cell-dependent inflammatory responses. Immunity 28:639–650. doi:10.1016/j.immuni.2008.03.017
Yanaba K et al (2009) The development and function of regulatory B cells expressing IL-10 (B10 cells) requires antigen receptor diversity and TLR signals. J Immunol 182:7459–7472. doi:10.4049/jimmunol.0900270
Yesavage JA et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Zhao L et al (2007) Changes of CD4+CD25+Foxp3+ regulatory T cells in aged Balb/c mice. J Leukoc Biol 81:1386–1394
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370
Acknowledgments
This research was supported by funding from the Research Councils UK New Dynamics of Ageing initiative administered through the Economic and Social Research Council (project RES-356-25-0011). We are grateful to the following hospital consultants for their assistance: Professor Sir Keith Porter (Queen Elizabeth Hospital Birmingham), Mr Martin Goodman (Queen Elizabeth Hospital Birmingham), Mr Edward Davis (Russell’s Hall Hospital Dudley) and Mr Sanjay Mistry (Heartlands Hospital Birmingham). We also acknowledge the support of the NIHR Wellcome Trust Clinical Research Facility at University Hospital Birmingham.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Duggal, N.A., Upton, J., Phillips, A.C. et al. Development of depressive symptoms post hip fracture is associated with altered immunosuppressive phenotype in regulatory T and B lymphocytes. Biogerontology 17, 229–239 (2016). https://doi.org/10.1007/s10522-015-9587-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10522-015-9587-7