Abstract
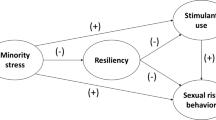
Gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria bear a disproportionately higher burden of HIV. Meyer’s minority stress theory posits that social stress due to the discrimination, violence, and stigma experienced by lesbian, gay, and bisexual men and women (LGBs)—due to their sexual orientation—may contribute to psychological problems, including mental health problems, substance use, and HIV sexual risk-taking. Between March and June 2019, we recruited 406 GBMSM from four states in Nigeria (Abuja, Delta, Lagos, and Plateau) to complete a cross-sectional survey at local community-based organizations. We utilized structural equation modeling to test whether psychological problems and substance use mediated the relationship between minority stress and HIV sexual risk-taking (condomless anal sex and number of sexual partners) among GBMSM in Nigeria. Minority stress (β = 0.60, 95% CI: 0.44–0.72, p ≤ .001), substance use (β = 0.43, 95% CI: 0.27–0.59, p = .004), and psychological problems (β = 0.35, 95% CI: 0.28–0.45 p = .012) had moderate associations with HIV sexual risk-taking. We found that psychological problems mediated the relationship between minority stress and HIV sexual risk-taking. Interventions focused on addressing psychological problems may help mitigate the effects of minority stress on HIV sexual risk-taking among GBMSM in Nigeria.


Similar content being viewed by others
References
Batchelder, A. W., Choi, K., Dale, S. K., Pierre-Louis, C., Sweek, E. W., Ironson, G., et al. (2019). Effects of syndemic psychiatric diagnoses on health indicators in men who have sex with men. Health Psychology, 38(6), 509–517.
Brown, T. A. (2014). Confirmatory factor analysis for applied research. New York: Guilford Publications.
Bruce, D., Harper, G. W., & Bauermeister, J. A. (2015). Minority stress, positive identity development, and depressive symptoms: Implications for resilience among sexual minority male youth. Psychology of Sexual Orientation and Gender Diversity, 2(3), 287–296.
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine, 158(16), 1789–1795.
Celentano, D. D., Valleroy, L. A., Sifakis, F., MacKellar, D. A., Hylton, J., Thiede, H., et al. (2006). Associations between substance use and sexual risk among very young men who have sex with men. Sexually Transmitted Diseases, 33(4), 265–271.
Choi, K.-H., Paul, J., Ayala, G., Boylan, R., & Gregorich, S. E. (2013). Experiences of discrimination and their impact on the mental health among African American, Asian and Pacific Islander, and Latino men who have sex with men. American Journal of Public Health, 103(5), 868–874.
Eaton, W. W., Smith, C., Ybarra, M., Muntaner, C., & Tien, A. (2004). Center for Epidemiologic Studies Depression Scale: Review and revision (CESD and CESD-R). In M. E. Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults (Vol. 1, pp. 363–377). Lawrence Erlbaum Associates Publishers.
Eluwa, G. I., Adebajo, S. B., Eluwa, T., Ogbanufe, O., Ilesanmi, O., & Nzelu, C. (2019). Rising HIV prevalence among men who have sex with men in Nigeria: A trend analysis. BMC Public Health, 19(1), 1201. https://doi.org/10.1186/s12889-019-7540-4.
English, D., Rendina, H. J., & Parsons, J. T. (2018). The effects of intersecting stigma: A longitudinal examination of minority stress, mental health, and substance use among Black, Latino, and multiracial gay and bisexual men. Psychology of Violence, 8(6), 669–679.
Fingerhut, A. W., Peplau, L. A., & Gable, S. L. (2010). Identity, minority stress and psychological well-being among gay men and lesbians. Psychology and Sexuality, 1(2), 101–114.
Frost, D. M., Lehavot, K., & Meyer, I. H. (2015). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 38(1), 1–8.
Green, K. E., & Feinstein, B. A. (2012). Substance use in lesbian, gay, and bisexual populations: An update on empirical research and implications for treatment. Psychology of Addictive Behaviors, 26(2), 265–278.
Gureje, O., Abdulmalik, J., Kola, L., Musa, E., Yasamy, M. T., & Adebayo, K. (2015). Integrating mental health into primary care in Nigeria: Report of a demonstration project using the mental health gap action programme intervention guide. BMC Health Services Research, 15(1), 1–8. https://doi.org/10.1186/s12913-015-0911-3.
Hatzenbuehler, M. L., Nolen-Hoeksema, S., & Erickson, S. J. (2008). Minority stress predictors of HIV risk behavior, substance use, and depressive symptoms: Results from a prospective study of bereaved gay men. Health Psychology, 27(4), 455–462.
Icard, L. D., Zhang, J., Jemmott, J. B., Sandfort, T. G., Rutledge, S. E., Van Greunen, D., & Martinez, O. (2020). The effects of three types of sexual orientation victimization on HIV sexual risk behavior among black south African men who have sex with men (MSM). Journal of Homosexuality, 67, 513–527.
Jeffries, W. L., Marks, G., Lauby, J., Murrill, C. S., & Millett, G. A. (2013). Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS and Behavior, 17(4), 1442–1453.
Korhonen, C., Kimani, M., Wahome, E., Otieno, F., Okall, D., Bailey, R. C., et al. (2018). Depressive symptoms and problematic alcohol and other substance use in 1476 gay, bisexual, and other MSM at three research sites in Kenya. AIDS, 32(11), 1507–1515.
Lewis, R. J., Derlega, V. J., Griffin, J. L., & Krowinski, A. C. (2003). Stressors for gay men and lesbians: Life stress, gay-related stress, stigma consciousness, and depressive symptoms. Journal of Social and Clinical Psychology, 22(6), 716–729.
Marsh, H. W., Hau, K.-T., & Wen, Z. (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling, 11(3), 320–341.
McAdams-Mahmoud, A., Stephenson, R., Rentsch, C., Cooper, H., Arriola, K. J., Jobson, G., et al. (2014). Minority stress in the lives of men who have sex with men in Cape Town, South Africa. Journal of Homosexuality, 61(6), 847–867.
McCarty-Caplan, D., Jantz, I., & Swartz, J. (2014). MSM and drug use: A latent class analysis of drug use and related sexual risk behaviors. AIDS and Behavior, 18(7), 1339–1351.
Meyer, I. H. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38–56.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697.
Muthén, B. (2011). Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. Los Angeles: Citeseer.
Newcomb, M. E., & Mustanski, B. (2011). Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: A meta-analysis. Archives of Sexual Behavior, 40(1), 189–199.
Oginni, O. A., Mapayi, B. M., Afolabi, O. T., Ebuenyi, I. D., Akinsulore, A., & Mosaku, K. S. (2019). Association between risky sexual behavior and a psychosocial syndemic among Nigerian men who have sex with men. Journal of Gay and Lesbian Mental Health, 23(2), 168–185.
Oginni, O. A., Mapayi, B. M., Afolabi, O. T., Obiajunwa, C., & Oloniniyi, I. O. (2020). Internalized homophobia, coping, and quality of life among Nigerian gay and bisexual men. Journal of Homosexuality, 67, 1447–1470.
Oginni, O. A., Mosaku, K. S., Mapayi, B. M., Akinsulore, A., & Afolabi, T. O. (2018). Depression and associated factors among gay and heterosexual male university students in Nigeria. Archives of Sexual Behavior, 47(4), 1119–1132.
Ogunbajo, A., Anyamele, C., Restar, A. J., Dolezal, C., & Sandfort, T. G. (2019a). Substance use and depression among recently migrated African gay and bisexual men living in the United States. Journal of Immigrant and Minority Health, 21(6), 1224–1232.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K. B., Kahler, C. W., Sandfort, T., & Mimiaga, M. J. (2020a). Validation of depressive symptoms, social support, and minority stress scales among gay, bisexual, and other men who have with men (GBMSM) in Nigeria, Africa: A mixed methods approach. BMC Public Health, 20, 1–12. https://doi.org/10.1186/s12889-020-09127-0.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K. B., Kahler, C. W., Sandfort, T. G., & Mimiaga, M. J. (2020b). Experiences of minority stress among gay, bisexual, and other men who have sex with men (GBMSM) in Nigeria, Africa: The intersection of mental health, substance use, and HIV sexual risk behavior. Global Public Health, 20. https://doi.org/10.1080/17441692.2020.1834598.
Ogunbajo, A., Iwuagwu, S., Williams, R., Biello, K., & Mimiaga, M. J. (2019b). Awareness, willingness to use, and history of HIV PrEP use among gay, bisexual, and other men who have sex with men in Nigeria. PLoS ONE, 14(12), e0226384.
Ogunbajo, A., Kang, A., Shangani, S., Wade, R. M., Onyango, D. P., Odero, W. W., & Harper, G. W. (2019c). Awareness and acceptability of pre-exposure prophylaxis (PrEP) among gay, bisexual and other men who have sex with men (GBMSM) in Kenya. AIDS Care, 31, 1185–1192.
Ogunbajo, A., Leblanc, N. M., Kushwaha, S., Boakye, F., Hanson, S., Smith, M. D., & Nelson, L. E. (2020c). Knowledge and acceptability of HIV pre-exposure prophylaxis (PrEP) among men who have sex with men (MSM) in Ghana. AIDS Care, 32, 330–336.
Ogunbajo, A., Oke, T., Jin, H., Rashidi, W., Iwuagwu, S., Harper, G. W., et al. (2020d). A syndemic of psychosocial health problems is associated with increased HIV sexual risk among Nigerian gay, bisexual, and other men who have sex with men (GBMSM). AIDS Care, 32, 337–343.
Okanlawon, K. (2018). Cultures of public intervention regarding LGBTQ issues after Nigeria’s same-sex marriage prohibition act (SSMPA). College Literature, 45(4), 641–651.
Pachankis, J. E., Hatzenbuehler, M. L., Hickson, F., Weatherburn, P., Berg, R. C., Marcus, U., & Schmidt, A. J. (2015). Hidden from health: Structural stigma, sexual orientation concealment, and HIV across 38 countries in the European MSM internet survey. AIDS, 29(10), 1239–1246.
Ramirez-Valles, J., Garcia, D., Campbell, R. T., Diaz, R. M., & Heckathorn, D. D. (2008). HIV infection, sexual risk behavior, and substance use among Latino gay and bisexual men and transgender persons. American Journal of Public Health, 98(6), 1036–1042.
Reisner, S. L., Mimiaga, M. J., Skeer, M., Bright, D., Cranston, K., Isenberg, D., et al. (2009). Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in Massachusetts. AIDS and Behavior, 13(4), 798–810.
Rendina, H. J., Gamarel, K. E., Pachankis, J. E., Ventuneac, A., Grov, C., & Parsons, J. T. (2017). Extending the minority stress model to incorporate HIV-positive gay and bisexual men’s experiences: A longitudinal examination of mental health and sexual risk behavior. Annals of Behavioral Medicine, 51(2), 147–158.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
Storholm, E. D., Huang, W., Siconolfi, D. E., Pollack, L. M., Carrico, A. W., Vincent, W., et al. (2019). Sources of resilience as mediators of the effect of minority stress on stimulant use and sexual risk behavior among young black men who have sex with men. AIDS and Behavior, 23(12), 3384–3395.
TIERS. (2019). Report on human rights violations based on real or perceived sexual orientation and gender identity in Nigeria (Vol. 4, pp. 1–37). The Initiative for Equal Rights Publications.
Tucker-Seeley, R. D., Mitchell, J. A., Shires, D. A., & Modlin, C. S. (2015). Financial hardship, unmet medical need, and health self-efficacy among African American men. Health Education and Behavior, 42(3), 285–292.
UNAIDS. (2017). UNAIDS Data 2017 (Vol. 1, No. 1, pp. 1–323). UNAIDS Publications.
Vosburgh, H. W., Mansergh, G., Sullivan, P. S., & Purcell, D. W. (2012). A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior, 16(6), 1394–1410.
Vu, L., Adebajo, S., Tun, W., Sheehy, M., Karlyn, A., Njab, J., et al. (2013). High HIV prevalence among men who have sex with men in Nigeria: Implications for combination prevention. JAIDS Journal of Acquired Immune Deficiency Syndromes, 63(2), 221–227.
Wong, C. F., Schrager, S. M., Holloway, I. W., Meyer, I. H., & Kipke, M. D. (2014). Minority stress experiences and psychological well-being: The impact of support from and connection to social networks within the Los Angeles house and ball communities. Prevention Science, 15(1), 44–55.
Wong, C. F., Weiss, G., Ayala, G., & Kipke, M. D. (2010). Harassment, discrimination, violence, and illicit drug use among young men who have sex with men. AIDS Education and Prevention, 22(4), 286–298.
Acknowledgements
We will like to thank all the participants of the study for their time and efforts. We would also like to thank the staff at Centre for Right to Health (Abuja) Equality Triangle Initiative (Delta), Improved Sexual Health and Rights Advocacy Initiative (ISHRAI, Lagos) and Hope Alive Health Awareness Initiative (Plateau). We also extend our gratitude to Olubiyi Oludipe (ISHRAI), Bala Mohammed Salisu (Hope Alive Health Awareness Initiative), Chucks Onuoha, Prince Bethel, Eke Chukwudi, Tochukwu Okereke, Josiah Djagvidi, Victor Brownson, and Odi Iorfa Agev, for providing logistical support to the Project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was supported by a R36 dissertation grant from the National Institute on Drug Abuse [DA047216] (principal investigator [PI]: Adedotun Ogunbajo) and by the Robert Wood Johnson Foundation Health Policy Research Scholars Program, for which the first author is a scholar but the foundation did not provide direct Project support.
Ethical Approval
The study protocols were approved by the institutional review boards at Brown University and the Nigerian Institute of Medical Research.
Informed Consent
Each participant provided verbal informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogunbajo, A., Iwuagwu, S., Williams, R. et al. Psychological Problems Mediate the Relationship Between Minority Stress and HIV Sexual Risk Among Nigerian Men Who Have Sex with Men: Testing the Minority Stress Model. Arch Sex Behav 50, 3163–3174 (2021). https://doi.org/10.1007/s10508-021-01943-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-021-01943-8