Abstract
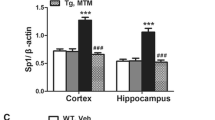
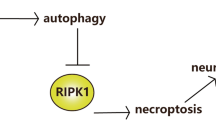
Alzheimer’s disease (AD), the most prevalent form of dementia, is characterized by progressive cognitive impairment accompanied by aberrant neuronal apoptosis. Reports suggest that the pro-apoptotic mammalian set20-like kinase 1/2 (MST1/2) instigates neuronal apoptosis via activating the Hippo signaling pathway under various stress conditions, including AD. However, whether inhibiting MST1/2 has any therapeutic benefits in AD remains unknown. Thus, we tested the therapeutic effects of intervening MST1/2 activation via the pharmacological inhibitor Xmu-mp-1 in a sporadic AD rat model. Sporadic AD was established in adult rats by intracerebroventricular streptozotocin (ICV-STZ) injection (3 mg/kg body weight). Xmu-mp-1 (0.5 mg/kg/body weight) was administered once every 48 h for two weeks, and Donepezil (5 mg/kg body weight) was used as a reference standard drug. The therapeutic effects of Xmu-mp-1 on ICV-STZ rats were determined through various behavioral, biochemical, histopathological, and molecular tests. At the behavioral level, Xmu-mp-1 improved cognitive deficits in sporadic AD rats. Further, Xmu-mp-1 treatment reduced STZ-associated tau phosphorylation, amyloid-beta deposition, oxidative stress, neurotoxicity, neuroinflammation, synaptic dysfunction, neuronal apoptosis, and neurodegeneration. Mechanistically, Xmu-mp-1 exerted these neuroprotective actions by inactivating the Hippo signaling while potentiating the Wnt/β-Catenin signaling in the AD rats. Together, the results of the present study provide compelling support that Xmu-mp-1 negated the neuronal dysregulation in the rat model of sporadic AD. Therefore, inhibiting MST/Hippo signaling and modulating its crosstalk with the Wnt/β-Catenin pathway can be a promising alternative treatment strategy against AD pathology. This is the first study providing novel mechanistic insights into the therapeutic use of Xmu-mp-1 in sporadic AD.










Similar content being viewed by others
Data availability
Data is provided in the masnucript and supplementary information file.
Abbreviations
- AChE:
-
Acetylcholinesterase
- AD:
-
Alzheimer’s disease
- APP:
-
Amyloid precursor protein
- Aβ:
-
Amyloid beta
- Bace-1:
-
Beta secretase-1
- BDNF:
-
Brain-derived neurotrophic factor
- GFAP:
-
Glial fibrillary acidic protein
- GSH:
-
Reduced glutathione
- Iba-1:
-
Ionized calcium-binding adaptor molecule 1
- ICV:
-
Intracerebroventricular
- Il-6:
-
Interleukin-6
- LATS:
-
Large tumor suppressor protein
- LPO:
-
Lipid peroxidation
- MAP-2:
-
Microtubule-associated protein – 2
- MST:
-
Mammalian Ste20-like protein
- MWM:
-
Morris water maze
- NOR:
-
Novel object recognition
- OFT:
-
Open field test
- PCO:
-
Protein carbonyl
- PMS:
-
Post-mitochondrial supernatant
- PSD-95:
-
Post synaptic scaffolding protein-95
- ROS:
-
Reactive oxygen species
- SOD:
-
Superoxide dismutase
- STZ:
-
Streptozotocin
- ThT:
-
ThioflavinT
- Tnf-α:
-
Tumour necrosis factor-α
- Xmu-mp-1:
-
4-((5,10-Dimethyl-6-oxo-6,10-dihydro-5H- pyrimido[5,4-b]thieno[3,2-e][1,4]diazepin-2-yl)amino)benzenesulfonamide
- YAP:
-
Yes-associated protein
References
Sanabria-Castro A, Alvarado-Echeverría I, Monge-Bonilla C (2017) Molecular pathogenesis of Alzheimer’s disease: an update. Ann Neurosci 24:46–54. https://doi.org/10.1159/000464422
Salkovic-Petrisic M, Osmanovic J, Grünblatt E et al (2009) Modeling sporadic Alzheimer’s disease: the insulin resistant brain state generates multiple long-term morphobiological abnormalities including hyperphosphorylated Tau protein and amyloid-β. J Alzheimer’s Dis 18:729–750. https://doi.org/10.3233/JAD-2009-1184
Pinton S, da Rocha JT, Gai BM, Nogueira CW (2011) Sporadic dementia of Alzheimer’s type induced by streptozotocin promotes anxiogenic behavior in mice. Behav Brain Res 223:1–6. https://doi.org/10.1016/j.bbr.2011.04.014
Burns A, Rossor M, Hecker J et al (1999) The effects of donepezil in Alzheimer’s disease-results from a multinational trial1. Dement Geriatr Cogn Disord 10:237–244. https://doi.org/10.1159/000017126
Reisberg B, Doody R, Stöffler A et al (2003) Memantine in moderate-to-severe Alzheimer’s disease. N Engl J Med 348:1333–1341. https://doi.org/10.1056/NEJMoa013128
Finn L (2017) Current medications for the treatment of Alzheimer’s disease: acetylcholinesterase inhibitors and NMDA receptor antagonist. In: Adejare A (ed) Drug discovery approaches for the treatment of neurodegenerative disorders: Alzheimer’s disease, 1st edn. Academic Press, Philadelphia, pp 49–58. https://doi.org/10.1016/B978-0-12-802810-0.00004-0
Shimohama S (2000) Apoptosis in Alzheimer’s disease—an update. Apoptosis 5:9–16. https://doi.org/10.1023/a:1009625323388
Sharma VK, Singh TG, Singh S et al (2021) Apoptotic pathways and Alzheimer’s disease: probing therapeutic potential. Neurochem Res 46:3103–3122. https://doi.org/10.1007/s11064-021-03418-7
Misra JR, Irvine KD (2018) The Hippo signaling network and its biological functions. Annu Rev Genet 52:65–87. https://doi.org/10.1146/annurev-genet-120417-031621
Wei X, Huang G, Liu J et al (2023) An update on the role of Hippo signaling pathway in ischemia-associated central nervous system diseases. Biomed Pharmacother 162:114619. https://doi.org/10.1016/j.biopha.2023.114619
Wang S-P, Wang L-H (2016) Disease implication of hyper-Hippo signalling. Open Biol 6. https://doi.org/10.1098/rsob.160119
Fallahi E, O’Driscoll NA, Matallanas D (2016) The MST/Hippo pathway and cell death: a non-canonical affair. Genes (Basel) 7:1–31. https://doi.org/10.3390/genes7060028
Su D, Li Y, Guan L et al (2021) Elevated MST1 leads to apoptosis via depletion of YAP1 in cardiomyocytes exposed to high glucose. Mol Med 27. https://doi.org/10.1186/s10020-021-00267-6
Lee JK, Shin JH, Hwang SG et al (2013) MST1 functions as a key modulator of neurodegeneration in a mouse model of ALS. Proc Natl Acad Sci U S A 110:12066–12071.https://doi.org/10.1073/pnas.1300894110
Zhu M, Gu H, Bai H et al (2024) Role and molecular regulatory mechanisms of Hippo signaling pathway in Caenorhabditis elegans and mammalian cell models of Alzheimer’s disease. Neurobiol Aging 134:9–20. https://doi.org/10.1016/j.neurobiolaging.2023.09.015
Sahu MR, Mondal AC (2020) The emerging role of Hippo signaling in neurodegeneration. J Neurosci Res 98:796–814. https://doi.org/10.1002/jnr.24551
Wang H, Shang Y, Wang E et al (2022) MST1 mediates neuronal loss and cognitive deficits: a novel therapeutic target for Alzheimer’s disease. Prog Neurobiol 214:102280. https://doi.org/10.1016/j.pneurobio.2022.102280
Bruno L, Karagil S, Mahmood A et al (2021) Mechanosensing and the Hippo pathway in microglia: a potential link to Alzheimer’s disease pathogenesis? Cells 10:3144. https://doi.org/10.3390/cells10113144
Fan F, He Z, Kong LL et al (2016) Pharmacological targeting of kinases MST1 and MST2 augments tissue repair and regeneration. Sci Transl Med 8. https://doi.org/10.1126/scitranslmed.aaf2304
Qu J, Zhao H, Li Q et al (2018) MST1 suppression reduces early brain injury by inhibiting the NF-κB/MMP-9 pathway after subarachnoid hemorrhage in mice. Behav Neurol 2018. https://doi.org/10.1155/2018/6470957
Zhang P, Wang T, Zhang D et al (2019) Exploration of MST1-Mediated Secondary Brain Injury Induced by Intracerebral Hemorrhage in Rats via Hippo Signaling Pathway. Transl Stroke Res 10:729–743. https://doi.org/10.1007/s12975-019-00702-1
Xu X, Shen X, Wang J et al (2021) YAP prevents premature senescence of astrocytes and cognitive decline of Alzheimer’s disease through regulating CDK6 signaling. Aging Cell 1–16. https://doi.org/10.1111/acel.13465
Giri S, Ranjan A, Kumar A et al (2021) Rapid eye movement sleep deprivation impairs neuronal plasticity and reduces hippocampal neuronal arborization in male albino rats: noradrenaline is involved in the process. J Neurosci Res 99:1815–1834. https://doi.org/10.1002/jnr.24838
Zhu L, Hou X-j, Che X, hang, et al (2021) Pseudoginsenoside-F11 attenuates cognitive dysfunction and tau phosphorylation in sporadic Alzheimer’s disease rat model. Acta Pharmacol Sin 42:1401–1408. https://doi.org/10.1038/s41401-020-00562-8
Moosavi M, Hooshmandi E, Javadpour P et al (2020) Effect of carbamylated erythropoietin Fc fusion protein (CEPO-Fc) on learning and memory impairment and hippocampal apoptosis induced by intracerebroventricular administration of streptozotocin in rats. Behav Brain Res 384:112554. https://doi.org/10.1016/j.bbr.2020.112554
Liu P, Cui L, Liu B et al (2020) Silibinin ameliorates STZ-induced impairment of memory and learning by up- regulating insulin signaling pathway and attenuating apoptosis. Physiol Behav 213:112689. https://doi.org/10.1016/j.physbeh.2019.112689
Bavarsad K, Hadjzadeh MAR, Hosseini M et al (2020) Effects of levothyroxine on learning and memory deficits in a rat model of Alzheimer’s disease: the role of BDNF and oxidative stress. Drug Chem Toxicol 43:57–63. https://doi.org/10.1080/01480545.2018.1481085
Mehla J, Pahuja M, Gupta YK (2013) Streptozotocin-induced sporadic Alzheimer’s Disease: selection of appropriate dose. J Alzheimer’s Dis 33:17–21. https://doi.org/10.3233/JAD-2012-120958
Xie C, Shen X, Xu X et al (2020) Astrocytic YAP promotes the formation of glia scars and neural regeneration after spinal cord injury. J Neurosci 40:2644–2662. https://doi.org/10.1523/JNEUROSCI.2229-19.2020
Triastuti E, Nugroho AB, Zi M et al (2019) Pharmacological inhibition of Hippo pathway, with the novel kinase inhibitor XMU-MP-1, protects the heart against adverse effects during pressure overload. Br J Pharmacol 176:3956–3971. https://doi.org/10.1111/bph.14795
Nair AB, Jacob S (2016) A simple practice guide for dose conversion between animals and human. J basic Clin Pharm 7:27–31. https://doi.org/10.4103/0976-0105.177703
Agrawal R, Tyagi E, Shukla R, Nath C (2009) A study of brain insulin receptors, AChE activity and oxidative stress in rat model of ICV STZ induced dementia. Neuropharmacology 56:779–787. https://doi.org/10.1016/j.neuropharm.2009.01.005
Siddiqui N, Ali J, Parvez S et al (2023) Neuroprotective role of DPP-4 inhibitor linagliptin against neurodegeneration, neuronal insulin resistance and neuroinflammation induced by intracerebroventricular streptozotocin in rat model of Alzheimer’s disease. Neurochem Res 48:2714–2730. https://doi.org/10.1007/s11064-023-03924-w
Lu Y, Sareddy GR, Wang J et al (2019) Neuron-derived estrogen regulates synaptic plasticity and memory. J Neurosci 39:2792–2809. https://doi.org/10.1523/JNEUROSCI.1970-18.2019
Wu C, Yang L, Li Y et al (2020) Effects of exercise training on anxious-depressive-like behavior in Alzheimer rat. Med Sci Sports Exerc 52:1456–1469. https://doi.org/10.1249/MSS.0000000000002294
Roy A, Sharma S, Nag TC et al (2022) Cognitive dysfunction and anxiety resulting from synaptic downscaling, hippocampal atrophy, and ventricular enlargement with intracerebroventricular streptozotocin injection in male wistar rats. Neurotox Res 40:2179–2202. https://doi.org/10.1007/s12640-022-00563-x
Nunez J (2008) Morris water maze experiment. J Vis Exp 12–13. https://doi.org/10.3791/897
Mishra SK, Singh S, Shukla S, Shukla R (2018) Intracerebroventricular streptozotocin impairs adult neurogenesis and cognitive functions via regulating neuroinflammation and insulin signaling in adult rats. Neurochem Int 113:56–68. https://doi.org/10.1016/j.neuint.2017.11.012
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254. https://doi.org/10.1016/0003-2697(76)90527-3
Jollow D, Mitchell JR, Zampaglione N, Gillette JR (1974) Bromobenzene-induced liver necrosis. protective role of glutathione and evidence for 3, 4-bromobenzene oxide as the hepatotoxic metabolite. Pharmacology 11:151–169. https://doi.org/10.1159/000136485
Marklund S, Marklund G (1974) Involvement of the superoxide anion radical in the autoxidation of pyrogallol and a convenient assay for superoxide dismutase. Eur J Biochem 47:469–474. https://doi.org/10.1111/j.1432-1033.1974.tb03714.x
Claiborne A (1985) Catalase activity. In: Greenwald RA (ed) Handbook of methods for oxygen radical research, 1st edn. CRC Press, Boca Raton, pp 283–284
Uchiyama M, Mihara M (1978) Determination of malonaldehyde precursor in tissues by thiobarbituric acid test. Anal Biochem 86:271–278. https://doi.org/10.1016/0003-2697(78)90342-1
Floor E, Wetzel MG (1998) Increased protein oxidation in human substantia nigra pars compacta in comparison with basal ganglia and prefrontal cortex measured with an improved dinitrophenylhydrazine assay. J Neurochem 70:268–275. https://doi.org/10.1046/j.1471-4159.1998.70010268.x
Ellman GL, Courtney KD, Andres V, Featherstone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 7:88–95. https://doi.org/10.1016/0006-2952(61)90145-9
Picken MM, Herrera GA (2012) Thiofl avin T stain: an easier and more sensitive method for amyloid detection. Amyloid Relat Disord Surg Pathol Clin Correl 187–189. https://doi.org/10.1007/978-1-60761-389-3
Neddens J, Temmel M, Flunkert S et al (2018) Phosphorylation of different tau sites during progression of Alzheimer’s disease. Acta Neuropathol Commun 6:52. https://doi.org/10.1186/s40478-018-0557-6
Tsatsanis A, Wong BX, Gunn AP et al (2020) Amyloidogenic processing of Alzheimer’s disease β-amyloid precursor protein induces cellular iron retention. Mol Psychiatry 25:1958–1966. https://doi.org/10.1038/s41380-020-0762-0
Huang WJ, Zhang X, Chen WW (2016) Role of oxidative stress in Alzheimer’s disease (review). Biomed Rep 4:519–522. https://doi.org/10.3892/br.2016.630
Jiang L, Li J, Zhang C et al (2020) YAP-mediated crosstalk between the Wnt and Hippo signaling pathways. Mol Med Rep 22:4101–4106. https://doi.org/10.3892/mmr.2020.11529
Abubakar MB, Sanusi KO, Ugusman A et al (2022) Alzheimer’s disease: an update and insights into pathophysiology. Front Aging Neurosci 14:1–16. https://doi.org/10.3389/fnagi.2022.742408
Akhtar A, Dhaliwal J, Saroj P et al (2020) Chromium picolinate attenuates cognitive deficit in ICV-STZ rat paradigm of sporadic Alzheimer’s-like dementia via targeting neuroinflammatory and IRS-1/PI3K/AKT/GSK-3β pathway. Inflammopharmacology 28:385–400. https://doi.org/10.1007/s10787-019-00681-7
Yan Y, Xu X, Chen R et al (2021) Down-regulation of MST1 in hippocampus protects against stress-induced depression-like behaviours and synaptic plasticity impairments. Brain Behav Immun 94:196–209. https://doi.org/10.1016/j.bbi.2021.02.007
Akhtar A, Bishnoi M, Sah SP (2020) Sodium orthovanadate improves learning and memory in intracerebroventricular-streptozotocin rat model of Alzheimer’s disease through modulation of brain insulin resistance induced tau pathology. Brain Res Bull 164:83–97. https://doi.org/10.1016/j.brainresbull.2020.08.001
Ding Y, Liu H, Cen M et al (2021) Rapamycin ameliorates cognitive impairments and Alzheimer’s disease-like pathology with restoring mitochondrial abnormality in the hippocampus of streptozotocin-induced diabetic mice. Neurochem Res 46:265–275. https://doi.org/10.1007/s11064-020-03160-6
Ahn Y, Seo J, Park J et al (2020) Synaptic loss and amyloid beta alterations in the rodent hippocampus induced by streptozotocin injection into the cisterna magna. Lab Anim Res 36:1–6. https://doi.org/10.1186/s42826-020-00049-x
Irwin M, Tare M, Singh A et al (2020) A positive feedback loop of Hippo-and c-Jun-amino-terminal kinase signaling pathways regulates amyloid-beta-mediated neurodegeneration. Front Cell Dev Biol 8:117. https://doi.org/10.3389/fcell.2020.00117
Qi Y, Sun D, Yang W et al (2020) Mammalian sterile 20-like kinase (MST) 1/2: crucial players in nervous and immune system and neurological disorders. J Mol Biol 432:3177–3190. https://doi.org/10.1016/j.jmb.2020.03.010
Sanphui P, Biswas SC (2013) FoxO3a is activated and executes neuron death via Bim in response to β-amyloid. Cell Death Dis 4:e625–e712. https://doi.org/10.1038/cddis.2013.148
Zhou W, Lei B, Yang C, et al (2023) Artemisia annua extract improves the cognitive deficits and reverses the pathological changes of Alzheimer’s disease via regulating YAP signaling. Int J Mol Sci 24. https://doi.org/10.3390/ijms24065259
Wei J, Yang F, Gong C et al (2019) Protective effect of daidzein against streptozotocin-induced Alzheimer’s disease via improving cognitive dysfunction and oxidative stress in rat model. J Biochem Mol Toxicol 33:e22319. https://doi.org/10.1002/jbt.22319
Akhtar A, Dhaliwal J, Sah SP (2021) 7,8-Dihydroxyflavone improves cognitive functions in ICV-STZ rat model of sporadic Alzheimer’s disease by reversing oxidative stress, mitochondrial dysfunction, and insulin resistance. Psychopharmacology 238:1991–2009. https://doi.org/10.1007/s00213-021-05826-7
Zhou X, Wang H, Li D et al (2022) MST1/2 inhibitor XMU-MP-1 alleviates the injury induced by ionizing radiation in haematopoietic and intestinal system. J Cell Mol Med 26:1621–1628. https://doi.org/10.1111/jcmm.17203
Yu L, Liu Y, Jin Y et al (2018) Lentivirus-mediated HDAC3 inhibition attenuates oxidative stress in APPswe/PS1dE9 mice. J Alzheimer’s Dis 61:1411–1424. https://doi.org/10.3233/JAD-170844
Biswas J, Goswami P, Gupta S et al (2016) Streptozotocin induced neurotoxicity involves Alzheimer’s related pathological markers: a study on N2A cells. Mol Neurobiol 53:2794–2806. https://doi.org/10.1007/s12035-015-9144-z
Tayanloo-Beik A, Kiasalari Z, Roghani M (2022) Paeonol ameliorates cognitive deficits in streptozotocin murine model of sporadic Alzheimer’s disease via attenuation of oxidative stress, inflammation, and mitochondrial dysfunction. J Mol Neurosci 72:336–348. https://doi.org/10.1007/s12031-021-01936-1
Caldeira C, Cunha C, Vaz AR et al (2017) Key aging-associated alterations in primary microglia response to beta-amyloid stimulation. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2017.00277
Karkhah A, Saadi M, Pourabdolhossein F et al (2021) Indomethacin attenuates neuroinflammation and memory impairment in an STZ-induced model of Alzheimer’s like disease. Immunopharmacol Immunotoxicol 43:758–766. https://doi.org/10.1080/08923973.2021.1981374
Rajkumar M, Kannan S, Thangaraj R (2023) Voglibose attenuates cognitive impairment, Aβ aggregation, oxidative stress, and neuroinflammation in streptozotocin-induced Alzheimer’s disease rat model. Inflammopharmacology 31:2751–2771. https://doi.org/10.1007/s10787-023-01313-x
Zhao S, Yin J, Zhou L et al (2016) Hippo/MST1 signaling mediates microglial activation following acute cerebral ischemia–reperfusion injury. Brain Behav Immun 55:236–248. https://doi.org/10.1016/j.bbi.2015.12.016
Geng C, Wei J, Wu C (2019) Mammalian STE20-like Kinase 1 knockdown attenuates TNFα-mediated neurodegenerative disease by repressing the JNK pathway and mitochondrial stress. Neurochem Res 44:1653–1664. https://doi.org/10.1007/s11064-019-02791-8
Chen B, Zhang Q, Yan Y, Zhang T (2022) MST1-knockdown protects against impairment of working memory via regulating neural activity in depression-like mice. Genes, Brain Behav 21:1–10. https://doi.org/10.1111/gbb.12782
Li X, Li K, Chen Y, Fang F (2021) The role of hippo signaling pathway in the development of the nervous system. Dev Neurosci 43:263–270. https://doi.org/10.1159/000515633
Kamat PK, Kalani A, Rai S et al (2016) Streptozotocin intracerebroventricular-induced neurotoxicity and brain insulin resistance: a therapeutic intervention for treatment of sporadic Alzheimer’s disease (sAD)-like pathology. Mol Neurobiol 53:4548–4562. https://doi.org/10.1007/s12035-015-9384-y
Graves JD, Gotoh Y, Draves KE et al (1998) Caspase-mediated activation and induction of apoptosis by the mammalian Ste20-like kinase Mst1. EMBO J 17:2224–2234. https://doi.org/10.1093/emboj/17.8.2224
Lehtinen MK, Yuan Z, Boag PR et al (2006) A conserved MST-FOXO signaling pathway mediates oxidative-stress responses and extends life span. Cell 125:987–1001. https://doi.org/10.1016/j.cell.2006.03.046
Ciltas AC, Karabulut S, Sahin B et al (2023) FGF-18 alleviates memory impairments and neuropathological changes in a rat model of Alzheimer’s disease. Neuropeptides 101:102367. https://doi.org/10.1016/j.npep.2023.102367
Sharma S, Verma S, Kapoor M et al (2016) Alzheimer’s disease like pathology induced six weeks after aggregated amyloid-beta injection in rats: increased oxidative stress and impaired long-term memory with anxiety-like behavior. Neurol Res 38:838–850. https://doi.org/10.1080/01616412.2016.1209337
Bae SJ, Luo X (2018) Activation mechanisms of the Hippo kinase signaling cascade. Biosci Rep 38:1–14. https://doi.org/10.1042/BSR20171469
Xiao L, Chen D, Hu P et al (2011) The c-Abl-MST1 signaling pathway mediates oxidative stress-induced neuronal cell death. J Neurosci 31:9611–9619. https://doi.org/10.1523/JNEUROSCI.0035-11.2011
Cheng J, Wang S, Dong Y, Yuan Z (2020) The role and regulatory mechanism of hippo signaling components in the neuronal system. Front Immunol 11:281. https://doi.org/10.3389/fimmu.2020.00281
Liu Y, Chu G, Shen W et al (2022) XMU-MP-1 protects heart from ischemia/reperfusion injury in mice through modulating Mst1/AMPK pathway. Eur J Pharmacol 174801. https://doi.org/10.1016/j.ejphar.2022.174801
Neininger AC, Dai X, Liu Q, Burnette DT (2021) The Hippo pathway regulates density-dependent proliferation of iPSC-derived cardiac myocytes. Sci Rep 11:1–20. https://doi.org/10.1038/s41598-021-97133-6
Alvarez AR, Godoy JA, Mullendorff K et al (2004) Wnt-3a overcomes β-amyloid toxicity in rat hippocampal neurons. Exp Cell Res 297:186–196. https://doi.org/10.1016/j.yexcr.2004.02.028
Palomer E, Buechler J, Salinas PC (2019) Wnt signaling deregulation in the aging and Alzheimer’s brain. Front Cell Neurosci 13:227. https://doi.org/10.3389/fncel.2019.00227
Xu F, Wang Y-L, Chang J-J et al (2014) Mammalian sterile 20-like kinase 1/2 inhibits the Wnt/β-catenin signalling pathway by directly binding casein kinase 1ε. Biochem J 458:159–169. https://doi.org/10.1042/BJ20130986
Ward D, Montes Olivas S, Fletcher A et al (2020) Cross-talk between Hippo and Wnt signalling pathways in intestinal crypts: Insights from an agent-based model. Comput Struct Biotechnol J 18:230–240. https://doi.org/10.1016/j.csbj.2019.12.015
Sileo P, Simonin C, Melnyk P et al (2022) Crosstalk between the Hippo Pathway and the Wnt Pathway in Huntington’s Disease and Other Neurodegenerative Disorders. Cells 11. https://doi.org/10.3390/cells11223631
Imajo M, Miyatake K, Iimura A et al (2012) A molecular mechanism that links Hippo signalling to the inhibition of Wnt/β-catenin signalling. EMBO J 31:1109–1122. https://doi.org/10.1038/emboj.2011.487
Azzolin L, Panciera T, Soligo S et al (2014) YAP/TAZ incorporation in the β-catenin destruction complex orchestrates the Wnt response. Cell 158:157–170. https://doi.org/10.1016/j.cell.2014.06.013
Lu L, Li Y, Kim SM et al (2010) Hippo signaling is a potent in vivo growth and tumor suppressor pathway in the mammalian liver. Proc Natl Acad Sci U S A 107:1437–1442.https://doi.org/10.1073/pnas.0911427107
Camargo FD, Gokhale S, Johnnidis JB et al (2007) YAP1 increases organ size and expands undifferentiated progenitor cells. Curr Biol 17:2054–2060. https://doi.org/10.1016/j.cub.2007.10.039
Acknowledgements
We acknowledge the central laboratory animal resources (CLAR) facility of Jawaharlal Nehru University for facilitating the animal experiments. We are thankful to Prof. Birendra Nath Mallick, School of Life Sciences (SLS), Jawaharlal Nehru University (JNU) for facilitating the stereotaxic surgery apparatus and ANY-Maze integrated behavioral setup.
Funding
This study was supported by the Department of Biotechnology (DBT), Govt. of India (BT/PR32907/MED/122/227/2019), (BT/PR38493/TRM/120/465/2020), and (BT/PR47726/CMD/150/26/2023), DBT- BUILDER-Level-III (BT/INF/22/SP45382/2022), and Department of Science & Technology, Govt. of India (DST-FIST-II) to the School of Life Sciences, JNU, India. Manas Ranjan Sahu acknowledges financial support from DST INSPIRE (DST/INSPIRE Fellowship/2018/IF180507).
Author information
Authors and Affiliations
Contributions
The study was conceptualized, designed, and supervised by Amal Chandra Mondal. Manas Ranjan Sahu carried out the experiments, analyzed the data, and wrote the manuscript. Mir Hilal Ahmad contributed to the experiments and manuscript editing. All authors reviewed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sahu, M.R., Ahmad, M.H. & Mondal, A.C. MST1 selective inhibitor Xmu-mp-1 ameliorates neuropathological changes in a rat model of sporadic Alzheimer’s Disease by modulating Hippo-Wnt signaling crosstalk. Apoptosis (2024). https://doi.org/10.1007/s10495-024-01975-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s10495-024-01975-0