Abstract
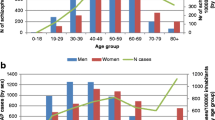
The co-occurrence of schizophrenia and substance use disorder (SUD) is clinically challenging and increasingly prevalent. This study compares trends in hospitalization characteristics of chronic psychotic patients with and without SUD in Israel, before and after introduction of the Community Rehabilitation of Persons with Mental Disability Law in 2000. The National Psychiatric Case Registry provided data on 18,684 adults with schizophrenia/schizoaffective disorders, hospitalized in 1991–2016 (at least once in 2010–2015). Repeated-measures ANOVA was used to measure the effect (and interactions) of group (patients with and without co-occurring disorders (COD)), time-period (Period1: 1991–2000, Period2: 2001–2009, Period3: 2010–2016) and age, on hospitalization measures—average length of stay (LOS), annual number of hospitalizations and hospitalization days. Among non-COD patients hospitalized in all three periods, LOS declined by half from 133.3 days in Period1 to 63.2 in Period3, and the annual number of hospitalizations increased slightly from 0.45 to 0.56. Among COD patients, LOS declined moderately from 82.7 days to 58.3 days, while annual hospitalizations increased dramatically from 0.56 to 0.82. The annual average number of hospitalization days/capita declined from 49.7 in Period1 to 26.3 in Period3 among non-COD patients, yet remained virtually unchanged among COD patients—39.6 and 37.4 in the two periods, respectively. Since introduction of the law, a significant improvement in hospitalization characteristics of chronic psychotic non-COD patients has been noted, whereas the situation worsened somewhat for COD patients. Community rehabilitation services for COD patients in Israel have yet to develop as a suitable alternative to hospitalization, and additional rehabilitation services are urgently needed.

Similar content being viewed by others
References
Adan, A., Arredondo, A. Y., Capella, M. D., Prat, G., Forero, D. A., & Navarro, J. F. (2017). Neurobiological underpinnings and modulating factors in schizophrenia spectrum disorders with a comorbid substance use disorder: A systematic review. Neuroscience and Biobehavioral Reviews, 75, 361–377. https://doi.org/10.1016/j.neubiorev.2017.01.038.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Aviram, U., & Azary-Viesel, S. (2018). Mental health reform in Israel: Challenge and opportunity. Part I: Fundamentals of the reform and the mental health service system on the eve of the reform. Israel Journal of Psychiatry & Related Science, 55(3), 45–54.
Aviram, U., Ginath, Y., & Roe, D. (2012). Mental health reforms in Europe: Israel's rehabilitation in the community of persons with mental disabilities law: Challenges and opportunities. Psychiatric Services, 63(2), 110–112. https://doi.org/10.1176/appi.ps.201100009.
Bahorik, A. L., Newhill, C. E., Queen, C. C., & Eack, S. M. (2014). Under-reporting of drug use among individuals with schizophrenia: Prevalence and predictors. Psychological Medicine, 44(1), 61–69. https://doi.org/10.1017/S0033291713000548.
Bar-Hamburger, R. (2006). Psychoactive substance use among Israeli resident from 1990 until 2005. Israel Anti-Drug Authority [Hebrew].
Bar-Hamburger, R., Ezrachi, Y., Roziner, I., Nirel, R. (2009). Psychoactive substance use among Israeli resident. Israel Anti-Drug Authority [Hebrew].
Bock, P. R., Friedel, W. E., Hanisch, J., Karasmann, M., & Schneider, B. (2004). Retrolective, comparative, epidemiological cohort study with parallel groups design for evaluation of efficacy and safety of drugs with "well-established use". Forsch Komplementarmed Klass Naturheilkd, Suppl 1, 23–29. https://doi.org/10.1159/000080572.
Bonny-Noach, H. (2019). Harm reduction drug policy in Israel: What has been accomplished and what still needs to be done? Israel Journal of Health Policy Research, 8(1), 75. https://doi.org/10.1186/s13584-019-0343-3.
Buckley, P. F. (2006). Prevalence and consequences of the dual diagnosis of substance abuse and severe mental illness. Journal of Clinical Psychiatry, 67(Suppl 7), 5–9.
Dixon, L. (1999). Dual diagnosis of substance abuse in schizophrenia: Prevalence and impact on outcomes. Schizophrenia Research, 35, S93–100.
Drake, R. E., Luciano, A. E., Mueser, K. T., Covell, N. H., Essock, S. M., Xie, H., et al. (2016). Longitudinal course of clients with co-occurring schizophrenia-spectrum and substance use disorders in urban mental health centers: A 7-Year prospective study. Schizophrenia Bulletin, 42(1), 202–211. https://doi.org/10.1093/schbul/sbv110.
D'Souza, D. C., Radhakrishnan, R., Sherif, M., Cortes-Briones, J., Cahill, J., Gupta, S., et al. (2016). Cannabinoids and psychosis. Current Pharmaceutical Design, 22(42), 6380–6391. https://doi.org/10.2174/1381612822666160826105628.
Eaton, W. W., Bilker, W., Haro, J. M., Herrman, H., Mortensen, P. B., Freeman, H., et al. (1992). Long-term course of hospitalization for schizophrenia: Part II. Change with passage of time. Schizophrenia Bulletin, 18(2), 229–241. https://doi.org/10.1093/schbul/18.2.229.
European Monitoring Centre for Drugs and Drug Addiction. (2013). Co-morbid substance use and mental disorders in Europe: A review of the data, EMCDDA Papers, Publications Office of the European Union, Luxembourg. Retrieved August 9, 2019, from https://www.emcdda.europa.eu/attachements.cfm/att_220660_EN_TDAU13002ENN.pdf.
Every-Palmer, S. (2011). Synthetic cannabinoid JWH-018 and psychosis: An explorative study. Drug and Alcohol Dependence, 117(2–3), 152–157. https://doi.org/10.1016/j.drugalcdep.2011.01.012.
Florentin, S., & Raskin, S. (2017). Co-occurring schizophrenia and substance use disorder: Etiological theories and challenges in Israel. Harefuah, 156(11), 715–719.
Florentin, S., Rosca, P., Raskin, S., Bdolah-Abram, T., & Neumark, Y. (2019). Psychiatric hospitalizations of chronic psychotic disorder patients with and without dual diagnosis, Israel, 1963–2016. Journal of Dual Diagnosis, 15(3), 130–139. https://doi.org/10.1080/15504263.2019.1609149.
Gastal, F. L., Andreoli, S. B., Quintana, M. I., Almeida Gameiro, M., Leite, S. O., & McGrath, J. (2000). Predicting the revolving door phenomenon among patients with schizophrenic, affective disorders and non-organic psychoses. Revista de Saude Publica, 34(3), 280–285. https://doi.org/10.1590/s0034-89102000000300011.
Green, A. I., Drake, R. E., Brunette, M. F., & Noordsy, D. L. (2007). Schizophrenia and co-occurring substance use disorder. American Journal of Psychiatry, 164(3), 402–408. https://doi.org/10.1176/ajp.2007.164.3.402.
Grinshpoon, A., Abramowitz, M. Z., Lerner, Y., & Zilber, N. (2007). Re-hospitalization of first-in-life admitted schizophrenic patients before and after rehabilitation legislation: A comparison of two national cohorts. Social Psychiatry and Psychiatric Epidemiology, 42(5), 355–359. https://doi.org/10.1007/s00127-007-0167-2.
Gur, R. E., Petty, R. G., Turetsky, B. I., & Gur, R. C. (1996). Schizophrenia throughout life: Sex differences in severity and profile of symptoms. Schizophrenia Research, 21, 1–12.
Harel-Fisch, Y., & Ezrachi, Y. (2017). Psychoactive drug use among the adult population in Israel—National epidemiological survey 2016. Israel Anti-Drug Authority
Hartz, S. M., Pato, C. N., Medeiros, H., Cavazos-Rehg, P., Sobell, J. L., Knowles, J. A., et al. (2014). Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry, 71(3), 248–254. https://doi.org/10.1001/jamapsychiatry.2013.3726.
Henwood, B. F., Padgett, D. K., & Tiderington, E. (2014). Provider views of harm reduction versus abstinence policies within homeless services for dually diagnosed adults. The Journal of Behavioral Health Services & Research, 41(1), 80–89. https://doi.org/10.1007/s11414-013-9318-2.
Hornik-Lurie, T., Zilber, N., & Lerner, Y. (2012). Trends in the use of rehabilitation services in the community by people with mental disabilities in Israel; the factors involved. Israel Journal of Health Policy Research, 1(1), 24. https://doi.org/10.1186/2045-4015-1-24.
Janssen, B., Gaebel, W., Haerter, M., Komaharadi, F., Lindel, B., & Weinmann, S. (2006). Evaluation of factors influencing medication compliance in inpatient treatment of psychotic disorders. Psychopharmacology (Berl), 187(2), 229–236. https://doi.org/10.1007/s00213-006-0413-4.
Jiménez-Castro, L., Hare, E., Medina, R., Raventos, H., Nicolini, H., Mendoza, R., et al. (2010). Substance use disorder comorbidity with schizophrenia in families of Mexican and Central American ancestry. Schizophrenia Research, 120(1–3), 87–94. https://doi.org/10.1016/j.schres.2010.02.1053.
Lichtenberg, P., Kaplan, Z., Grinshpoon, A., Feldman, D., & Nahon, D. (1999). The goals and limitations of Israel’s psychiatric case register. Psychiatric Services, 50, 1043–1048.
Lybrand, J., & Caroff, S. N. (2009). Management of schizophrenia with substance use disorders. Psychiatric Clinics of North America, 32, 821–833. https://doi.org/10.1016/j.psc.2009.09.002.
Magura, S. (2008). Effectiveness of dual focus mutual aid for co-occurring substance use and mental health disorders: A review and ynthesis of the “Double Trouble” in recovery evaluation. Substance Use and Misuse, 43, 1904–1926. https://doi.org/10.1080/10826080802297005.
Mancevski, B., Keilp, J., Kurzon, M., Berman, R. M., Ortakov, V., Harkavy-Friedman, J., et al. (2007). Lifelong course of positive and negative symptoms in chronically institutionalized patients with schizophrenia. Psychopathology, 40, 83–92. https://doi.org/10.1159/000098488.
Manuel, J. I., Gandy, M. E., & Rieker, D. (2015). Trends in hospital discharges and dispositions for episodes of co-occurring severe mental illness and substance use disorders. Administration and Policy in Mental Health and Mental Health Services Research, 42(2), 168–175. https://doi.org/10.1007/s10488-014-0540-x.
Marquez-Arrico, J. E., López-Vera, S., Prat, G., & Adan, A. (2016). Temperament and character dimensions in male patients with substance use disorders: Differences relating to psychiatric comorbidity. Psychiatry Research, 237, 1–8. https://doi.org/10.1016/j.psychres.2016.01.061.
Ministry of Health. (2015). Information Division, Division of Technologies, Medical Information and Research. Mental Health in Israel. Statistical Abstract (English and Hebrew).
Ministry of Justice. (2001). Rehabilitation of the Mentally Disabled in the Community Law of 2001 (RMD) Israeli Law Code (2001), 1746 Jerusalem: Ministry of Justice [Hebrew].
Mortensen, P. B., & Eaton, W. W. (1994). Predictors for readmission risk in schizophrenia. Psychological Medicine, 24(1), 223–232.
Mueser, K. T., Drake, R. E., & Wallach, M. A. (1998). Dual diagnosis: A review of etiological theories. Addictive Behaviors, 23, 717–734.
Natan, G. (2010). Treatment of drug dependent persons with co-morbid mental illness. Report to the Israeli Parliament (Knesset), Jerusalem, Israel [Hebrew]. Retrieved August 9, 2019, fromhttps://www.knesset.gov.il/mmm/data/pdf/m02377.pdf
Nesvåg, R., Knudsen, G. P., Bakken, I. J., Høye, A., Ystrom, E., Surén, P., et al. (2015). Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: A registry-based study. Social Psychiatry and Psychiatric Epidemiology, 50, 1267–1276. https://doi.org/10.1007/s00127-015-1025-2.
Radhakrishnan, R., Wilkinson, S. T., & D'Souza, D. C. (2014). Gone to Pot—A review of the association between cannabis and psychosis. Frontiers Psychiatry, 5, 54. https://doi.org/10.3389/fpsyt.2014.00054.
Regier, D. A., Farmer, M. E., Rae, D. S., Locke, B. Z., Keith, S. J., Judd, L. L., et al. (1990). Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA Psychiatry, 264, 2511–2518.
Río-Martínez, L., Marquez-Arrico, J. E., Prat, G., & Adan, A. (2020). Temperament and character profile and its clinical correlates in male patients with dual schizophrenia. J. Clin. Med., 9, 1876. https://doi.org/10.3390/jcm9061876.
Roe, D., Hasson-Ohayon, I., Lachman, M., & Kravetz, S. (2007). Selecting and implementing evidence-based practices in psychiatric rehabilitation services in Israel: A worthy and feasible challenge. Israel Journal of Psychiatry and Related Science, 44(1), 47–53.
Roe, D., Lachman, M., & Mueser, K. T. (2010). Editorial: A decade of the Israeli psychiatric rehabilitation law. Israel Journal of Psychiatry and Related Science, 47(3), 164–165.
Samaha, A. N. (2014). Can antipsychotic treatment contribute to drug addiction in schizophrenia? Progress in Neuro-psychopharmacology and Biological Psychiatry, 52, 9–16.
Schmidt, L. M., Hesse, M., & Lykke, J. (2011). The impact of substance use disorders on the course of schizophrenia—A 15-year follow-up study: Dual diagnosis over 15 years. Schizophrenia Research, 130(1–3), 228–233. https://doi.org/10.1016/j.schres.2011.04.011.
Shalit, N., Barzilay, R., Shoval, G., Shlosberg, D., Mor, N., Zweigenhaft, N., et al. (2016). Characteristics of synthetic cannabinoid and cannabis users admitted to a psychiatric hospital: A Comparative sstudy. Journal of Clinical Psychiatry, 77(8), e989–e995. https://doi.org/10.4088/JCP.15m09938.
Soyka, M., Albus, M., Kathmann, N., Finelli, A., Hofstetter, S., Holzbach, R., et al. (1993). Prevalence of alcohol and drug abuse in schizophrenic inpatients. European Archives of Psychiatry and Clinical Neuroscience, 242(6), 362–372. https://doi.org/10.1007/BF02190250.
Swartz, M. S., Wagner, H. R., Swanson, J. W., Stroup, T. S., McEvoy, J. P., Canive, J. M., et al. (2006). Substance use in persons with schizophrenia: Baseline prevalence and correlates from the NIMH CATIE study. The Journal of Nervous Mental Disease, 194, 164–172. https://doi.org/10.1097/01.nmd.0000202575.79453.6e.
Sytema, S., Burgess, P., & Tansella, M. (2002). Does community care decrease length of stay and risk of rehospitalization in new patients with schizophrenia disorders? A comparative case register study in Groningen, The Netherlands; Victoria, Australia; and South-Verona, Italy. Schizophrenia Bulletin, 28(2), 273–281. https://doi.org/10.1093/oxfordjournals.schbul.a006937.
Talamo, A., Centorrino, F., Tondo, L., Dimitri, A., Hennen, J., & Baldessarini, R. J. (2006). Comorbid substance-use in schizophrenia: Relation to positive and negative symptoms. Schizophrenia Research, 86, 251–255. https://doi.org/10.1016/j.schres.2006.04.004.
Toftdahl, N. G., Nordentoft, M., & Hjorthøj, C. (2016). Prevalence of substance use disorders in psychiatric patients: A nationwide Danish population-based study. Social Psychiatry and Psychiatric Epidemiology, 51(1), 129–140. https://doi.org/10.1007/s00127-015-1104-4.
Winklbaur, B. (2006). Substance abuse in patients with schizophrenia. Dialogues in Clinical Neuroscience, 8(1), 37–43.
Funding
No external funds were used to support this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest. This research was conducted within the framework of SF's thesis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Florentin, S., Neumark, Y., Raskin, S. et al. Differential Effect of Community Rehabilitation Reform on Hospitalizations of Patients with Chronic Psychotic Disorders With and Without Substance Use Disorder, Israel, 1991–2016. Adm Policy Ment Health 48, 354–362 (2021). https://doi.org/10.1007/s10488-020-01077-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10488-020-01077-4