Abstract
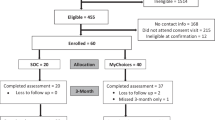
A qualitative systematic review was conducted to evaluate pre-exposure prophylaxis (PrEP) interventions, describe characteristics of best practices for increasing PrEP use and persistence, and explore research gaps based on current PrEP interventions. We searched CDC’s Prevention Research Synthesis (PRS) Project’s cumulative HIV database (includes CINAHL, EMBASE, Global Health, MEDLINE, PsycInfo, and Sociological Abstracts) to identify PrEP intervention studies conducted in the U.S., published between 2000 and 2022 (last searched January 2023). Eligibility criteria include studies that evaluated PrEP interventions for persons testing negative for HIV infection, or for healthcare providers who prescribed PrEP; included comparisons between groups or pre/post; and reported at least one relevant PrEP outcome. Each eligible intervention was evaluated on the quality of study design, implementation, analysis, and strength of evidence (PROSPERO registration number: CRD42021256460). Of the 26 eligible interventions, the majority were focused on men who have sex with men (n = 18) and reported PrEP adherence outcomes (n = 12). Nine interventions met the criteria for Best Practices (i.e., evidence-based interventions, evidence-informed interventions). Five were digital health interventions while two implemented individual counseling, one offered motivational interviewing, and one provided integrated medical care with a PrEP peer navigator. Longer intervention periods may provide more time for intervention exposure to facilitate behavioral change, and engaging the community when developing, designing and implementing interventions may be key for effectiveness. For digital health interventions, two-way messaging may help participants feel supported. Research gaps included a lack of Best Practices for several populations (e.g., Black persons, Hispanic/Latino persons, persons who inject drugs, and women of color) and evidence for various intervention strategies (e.g., interventions for promoting provider’s PrEP prescription behavior, peer support). These findings call for more collaborative work with communities to develop interventions that work and implement and disseminate Best Practices for increasing PrEP use and persistence in communities.

Similar content being viewed by others
References
U.S. Centers for Disease Control and Prevention: PrEP Effectiveness. 2021. https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html. Accessed 27 Aug 2021.
HIV.gov. What is Ending the HIV Epidemic in the U.S.? 2019. https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed 3 Feb 2022.
U.S. Department of Health and Human Services: HIV National Strategic Plan for the United States: A Roadmap to End the Epidemic 2021–2021. 2021. https://files.hiv.gov/s3fs-public/HIV-National-Strategic-Plan-2021-2025.pdf#:~:text=HIV%20National%20Strategic%20Plan%3A%202021%E2%80%932025%20i%20VISION%20The,all%20people%2C%20regardless%20of%20age%2C%20sex%2C%20gender%20identity%2C.
U.S. Food and Drug Administration. Truvada for PrEP Fact Sheet: Ensuring Safe and Proper Use. 2012. https://www.fda.gov/media/83586/download.
Centers for Disease Control and Prevention. HIV Surveillance Report, 2021. 2023. 34. https://www.cdc.gov/hiv/library/reports/hiv-surveillance/vol-34/index.html. Accessed 24 May 2023.
Centers for Disease Control and Prevention. Expanding PrEP Coverage in the United States to Achieve EHE Goals. 2023. https://www.cdc.gov/nchhstp/dear_colleague/2023/dcl-101723-prep-coverage.html. Accessed 2 Feb 2024.
Centers for Disease Control and Prevention. PrEP for HIV Prevention in the U.S. 2023. https://www.cdc.gov/nchhstp/newsroom/fact-sheets/hiv/prep-for-hiv-prevention-in-the-us-factsheet.html. Accessed 6 March 2024.
Lyles CM, Crepaz N, Herbst JH, Kay LS. Evidence-based HIV behavioral prevention from the perspective of the CDC’s HIV/AIDS Prevention Research Synthesis Team. AIDS Educ Prev. 2006;18(4 Suppl A):21–31.
U.S. Centers for Disease Control and Prevention. Pre-Exposure Prophylaxis (PrEP) Chapter. 2022. https://www.cdc.gov/hiv/research/interventionresearch/compendium/prep/index.html. Accessed 30th Aug 2022.
Kamitani E, Higa D, Crepaz N, Wichser M, Mullins M, (PRS); TCsPRSP. Evidence-Based and Evidence-Informed Interventions for HIV Pre-exposure Prophylaxis (PrEP) Use and Persistence: a Systematic Review. 2021. CRD42021256460:https://www.crd.york.ac.uk/PROSPERO/display_record.php?RecordID=256460. Accessed 24th Mar 2022.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;2021:372:n71.
Kamitani E, Johnson AH, Wichser M, Mizuno Y, DeLuca JB, Higa DH. Mapping the study topics and characteristics of HIV pre-exposure prophylaxis research literature: a protocol for a scoping review. BMJ Open. 2019;9(5):e024212.
DeLuca JB, Mullins MM, Lyles CM, Crepaz N, Kay L, Thadiparthi S. Developing a comprehensive search strategy for evidence based systematic reviews. Evid Based Lib Inf Pract. 2008;3(1):3–32.
U.S. Centers for Disease Control and Prevention. PrEP Best Practices Criteria. Compedium of Evidence-Based Interventions and Best Practices for HIV Prevention 2021. https://www.cdc.gov/hiv/research/interventionresearch/compendium/prep/prep-best-practices.html. Accessed 21 Mar 2022.
Flores SA, Crepaz N. Quality of study methods in individual- and group-level HIV intervention research: critical reporting elements. AIDS Educ Prev. 2004;16(4):341–52.
Blumenthal J, Jain S, Mulvihill E, et al. Perceived versus calculated HIV risk: Implications for pre-exposure prophylaxis uptake in a randomized trial of men who have sex with men. JAIDS J Acquir Immun Defic Syndr. 2019;80(2):e23–9.
Colson PW, Franks J, Wu Y, et al. Adherence to pre-exposure prophylaxis in Black men who have sex with men and transgender women in a community setting in Harlem. NY AIDS Behav. 2020;24:3436–55.
Harawa NT, Schrode KM, McWells C, Weiss RE, Hilliard CL, Bluthenthal RN. Small randomized controlled trial of the new passport to wellness HIV prevention intervention for black men who have sex with men (BMSM). AIDS Educ Prev. 2020;32(4):311–24.
Mitchell JT, LeGrand S, Hightow-Weidman LB, et al. Smartphone-based contingency management intervention to improve pre-exposure prophylaxis adherence: Pilot trial. JMIR Mhealth Uhealth. 2018;6(9): e10456.
Molina JM, Capitant C, Spire B, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015;373(23):2237–46.
Raifman J, Nunn A, Oldenburg CE, et al. An evaluation of a clinical pre-exposure prophylaxis education intervention among men who have sex with men. Health Serv Res. 2018;53(4):2249–67.
Songtaweesin WN, Kawichai S, Phanuphak N, et al. Youth-friendly services and a mobile phone application to promote adherence to pre-exposure prophylaxis among adolescent men who have sex with men and transgender women at-risk for HIV in Thailand: a randomized control trial. J Int AIDS Soc. 2020;23(Suppl 5):e25564.
Arnold EA, Saberi P, Wong JO, et al. We are family: a feasibility and acceptability study of an HIV prevention intervention with the house ball and gay family communities. J Acquir Immun Def Syndr. 2021;88(1):S6–11.
Young LE, Schneider JA. The co-evolution of network structure and PrEP adoption among a large cohort of PrEP peer leaders: implications for intervention evaluation and community capacity-building. Int J Environ Res Public Health. 2021. https://doi.org/10.3390/ijerph18116051.
Wray TB, Luo X, Ke J, Pérez AE, Carr DJ, Monti PM. Using smartphone survey data and machine learning to identify situational and contextual risk factors for HIV risk behavior among men who have sex with men who are not on PrEP. Prev Sci. 2019;20(6):904–13.
Moore DJ, Jain S, Dubé MP, et al. Randomized controlled trial of daily text messages to support adherence to preexposure prophylaxis in individuals at risk for human immunodeficiency virus: the TAPIR study. Clin Infect Dis. 2018;66(10):1566–72.
Mayer KH, Safren SA, Elsesser SA, et al. Optimizing pre-exposure antiretroviral prophylaxis adherence in men who have sex with men: results of a pilot randomized controlled trial of “life-steps for PrEP.” AIDS Behav. 2017;21(5):1350–60.
Liu AY, Vittinghoff E, von Felten P, et al. Randomized controlled trial of a mobile health intervention to promote retention and adherence to preexposure prophylaxis among young people at risk for human immunodeficiency virus: the EPIC study. Clin Infect Dis. 2019;68(12):2010–7.
Fuchs JD, Stojanovski K, Vittinghoff E, et al. A mobile health strategy to support adherence to antiretroviral preexposure prophylaxis. AIDS Patient Care STDS. 2018;32(3):104–11.
Desrosiers A, Levy M, Dright A, et al. A randomized controlled pilot study of a culturally-tailored counseling intervention to increase uptake of HIV pre-exposure prophylaxis among young black men who have sex with men in washington, DC. AIDS Behav. 2019;23(1):105–15.
Chan PA, Nunn A, van den Berg JJ, et al. A randomized trial of a brief behavioral intervention for PrEP uptake among men who have sex with men at increased risk for HIV infection. J Acquir Immune Defic Syndr. 2021;87(3):937–43.
Sullivan PS, Stephenson R, Hirshfield S, et al. Behavioral efficacy of a sexual health mobile app for men who have sex with men: randomized controlled trial of mobile messaging for men. J Med Internet Res. 2022;24(2):e34574.
Weitzman PF, Zhou Y, Kogelman L, Rodarte S, Vicente SR, Levkoff SE. mHealth for pre-exposure prophylaxis adherence by young adult men who have sex with men. Mhealth. 2021;7:44.
Stephenson R, Todd K, Kahle E, et al. Project Moxie: Results of a feasibility study of a telehealth intervention to increase HIV testing among binary and nonbinary transgender youth. AIDS Behav. 2020;24(5):1517–30.
Dale SK. Using motivational interviewing to increase PrEP uptake among Black women at risk for HIV: an open pilot trial of MI-PrEP. J Racial Ethn Health Disparities. 2020;7(5):913–27.
Phillips A, Harmon JL, Bera J, Ogle M, Thompson J. Integrating preexposure prophylaxis (PrEP) into a network of community health centers. J Nurse Practitioners. 2020;16(3):232–5.
Furukawa NW, Weimer M, Willenburg KS, et al. Expansion of preexposure prophylaxis capacity in response to an HIV outbreak among people who inject drugs-Cabell County, West Virginia, 2019. Public Health Rep Jan-Feb. 2022;137(1):25–31.
Storholm ED, Siconolfi D, Huang W, et al. Project SLIP: implementation of a PrEP screening and linkage intervention in primary care. AIDS Behav. 2021;25(8):2348–57.
Coleman M, Hodges A, Henn S, Lambert CC. Integrated pharmacy and PrEP navigation services to support PrEP uptake: a quality improvement project. J Assoc Nurses AIDS Care Nov-Dec. 2020;31(6):685–92.
Arnold T. An Acceptance Based PrEP Intervention to Engage Young Black MSM in the South. 2021. https://reporter.nih.gov/search/Ytsm7QuhhEKDb9QuOexPiA/project-details/10253247. Accessed 16 Jan 2024.
Wray TB, Kahler CW, Simpanen EM, Operario D. A preliminary randomized controlled trial of Game Plan, a web application to help men who have sex with men reduce their HIV risk and alcohol use. AIDS Behav. 2019;23(6):1668–79.
The Community Guide. HIV Prevention: Digital Health Interventions to Improve Adherence to HIV Pre-Exposure Prophylaxis. 2021; https://thecommunityguide.org/findings/hiv-prevention-digital-health-interventions-improve-adherence-hiv-pre-exposure-prophylaxis.html. Accessed 23 Jan 2023.
Buchbinder S. PrEP-3D: An Integrated Pharmacy Digital Diary and Delivery Strategy to Increase PrEP Use Among MSM. 4/8/2019–3/31/2024. https://reporter.nih.gov/search/eaLbb0atxE-Py1yPCP8P_w/project-details/9910448.
Centers for Disease Control and Prevention. US Public Health Service: Preexposure prophylaxis for the Prevention of HIV infection in the United States - 2021 Update: a clinicl practice guideline. 2021. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf. Accessed 23 Nov 2022.
Masa RD. Intersectional Stigma and Resilience among Young Latinx Gay, Bisexual and Other Men who have Sex with Men to Improve HIV Testing and PrEP Uptake: National Institute on Minority Health and Health Disparities; 2021.
Shrestha R, Altice FL, Karki P, Copenhaver MM. Integrated bio-behavioral approach to improve adherence to pre-exposure prophylaxis and reduce HIV risk in people who use drugs: a pilot feasibility study. AIDS Behav. 2018;22(8):2640–9.
Sieving RE, McRee AL, Secor-Turner M, et al. Prime Time: long-term sexual health outcomes of a clinic-linked intervention. Perspect Sex Reprod Health. 2014;46(2):91–100.
Davey-Rothwell MA, Tobin K, Yang C, Sun CJ, Latkin CA. Results of a randomized controlled trial of a peer mentor HIV/STI prevention intervention for women over an 18 month follow-up. AIDS Behav. 2011;15(8):1654–63.
Ortblad K, Kibuuka Musoke D, Ngabirano T, et al. Direct provision versus facility collection of HIV self-tests among female sex workers in Uganda: a cluster-randomized controlled health systems trial. PLoS Med. 2017;14(11): e1002458.
Cunningham WE, Weiss RE, Nakazono T, et al. Effectiveness of a peer navigation intervention to sustain viral suppression among HIV-positive men and transgender women released from jail: The LINK LA randomized clinical trial. JAMA Intern Med. 2018;178(4):542–53.
Ruria EC, Masaba R, Kose J, et al. Optimizing linkage to care and initiation and retention on treatment of adolescents with newly diagnosed HIV infection. AIDS. 2017;31(Suppl 3):S253-s260.
Messeri P, Yomogida M, Ferat RM, Garr L, Wirth D. An HIV health plan patient navigation program: Engaging HIV positive individuals in primary medical care. J of HIV/AIDS Soc Serv. 2020;19(1):55–73.
Bouris A, Jaffe K, Eavou R, et al. Project nGage: results of a randomized controlled trial of a dyadic network support intervention to retain young black men who have sex with men in HIV Care. AIDS Behav. 2017;21(12):3618–29.
Denison JA, Burke VM, Miti S, et al. Project YES! youth engaging for success: a randomized controlled trial assessing the impact of a clinic-based peer mentoring program on viral suppression, adherence and internalized stigma among HIV-positive youth (15–24 years) in Ndola, Zambia. PLoS ONE. 2020;15(4): e0230703.
Kerrigan D, Mbwambo J, Likindikoki S, et al. Project Shikamana: community empowerment-based combination HIV prevention significantly impacts HIV incidence and care continuum outcomes among female sex workers in Iringa, Tanzania. J acquir Immun Def Syndr. 2019;82(2):141–8.
Clement, ME: mHealth Peer Support to Reduce Rates of STIs in Black MSM PrEP Users. 9/3/2018–8/31/2023. https://reporter.nih.gov/search/-8bQvi425EuN6uDdoWJADA/project-details/10003946.
Horvath, KJ: PrEP iT! A Pilot Test of a Mobile Peer Support Intervention to Optimize PrEP Adherence and Retention in PrEP Care: NATIONAL INSTITUTE OF MENTAL HEALTH.
Funding
None.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Centers for Disease Control and Prevention.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kamitani, E., Higa, D.H., Crepaz, N. et al. Identifying Best Practices for Increasing HIV Pre-exposure Prophylaxis (PrEP) Use and Persistence in the United States: A Systematic Review. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04332-z
Accepted:
Published:
DOI: https://doi.org/10.1007/s10461-024-04332-z