Abstract
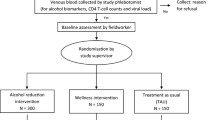
We evaluated the feasibility, acceptability, and preliminary efficacy of an economic and relationship-strengthening intervention to reduce heavy alcohol use among couples living with HIV in Malawi (Mlambe). Mlambe consisted of training on financial literacy and relationship skills, combined with 1:1 matched savings accounts to invest in an income-generating activity. In a randomized controlled trial, we compared Mlambe to enhanced usual care (EUC). We enrolled 78 married couples having a partner on antiretroviral therapy (ART) who reported heavy alcohol use based on the AUDIT-C. Using targets of 75%, primary outcomes included retention rates at 10 and 15-months, session attendance rates, and satisfaction with Mlambe. Exploratory outcomes were heavy alcohol use (AUDIT-C and/or PEth positive), number of drinking days in the past month, AUDIT-C score, optimal adherence to ART (95% or higher), and viral suppression. We exceeded our targets for feasibility and acceptability metrics. Retention rates were 96% at 15-months. Session attendance and satisfaction levels were both 100%. From baseline to 15-months, Mlambe participants reported decreases in mean number of drinking days (from 6.8 to 2.1) and AUDIT-C scores (from 7.5 to 3.1); while ART adherence rates improved across the same period (from 63.2 to 73.9%). Participants in Mlambe, as compared to those in EUC, had lower rates of heavy alcohol use (89.5% vs. 97.2%) and higher rates of viral suppression (100% vs. 91.9%) at 10-months. Differences between arms were not statistically significant in this small pilot study. Mlambe was highly feasible and acceptable, and shows promise for reducing heavy alcohol use and viral non-suppression among couples with HIV in a larger efficacy study.


Similar content being viewed by others
Data Availability
Not available due to the potential to identify participants.
Code Availability
Not applicable.
References
Schneider M, Chersich M, Temmerman M, Degomme O, Parry CD. The impact of alcohol on HIV prevention and treatment for South africans in primary healthcare. Curationis. 2014;37(1):1–8.
Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. 2010;7(4):226–33.
Williams EC, Hahn JA, Saitz R et al. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcoholism: Clinical and Experimental Research. 2016;40(10):2056-72.
Salmon-Ceron D, Lewden C, Morlat P, et al. Liver disease as a major cause of death among HIV infected patients: role of hepatitis C and B viruses and alcohol. J Hepatol. 2005;42(6):799–805.
Braithwaite RS, Bryant KJ. Influence of alcohol consumption on adherence to and toxicity of antiretroviral therapy and survival. Alcohol Res Health. 2010;33(3):280.
Velloza J, Kemp CG, Aunon FM, et al. Alcohol use and antiretroviral therapy non-adherence among adults living with HIV/AIDS in sub-saharan Africa: a systematic review and meta-analysis. AIDS Behav. 2020;24:1727–42.
World Health Organization. Global status report on alcohol and health 2018. World Health Organization; 2019.
Kalichman SC, Simbayi LC, Kagee A, et al. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Soc Sci Med. 2006;62(7):1641–9.
Dunkle KL, Jewkes RK, Brown HC, et al. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59:1581–92.
Setlalentoa B, Pisa P, Thekisho G, Ryke E, Loots Du T. The social aspects of alcohol misuse/abuse in South Africa. South Afr J Clin Nutr. 2010;23(sup2):11–5.
Rodriguez LM, Neighbors C, Knee CR. Problematic alcohol use and marital distress: an interdependence theory perspective. Addict Res Theory. 2014;22(4):294–312.
Woolf-King SE, Conroy AA, Fritz K et al. Alcohol use and relationship quality among South African couples. Subst Use Misuse. 2018:1–10.
Conroy AA, McKenna SA, Ruark A. Couple interdependence impacts alcohol use and adherence to antiretroviral therapy in Malawi. AIDS Behav. 2019;23(1):201–10.
Conroy AA, McKenna SA, Leddy A, et al. If she is Drunk, I don’t want her to take it: Partner beliefs and Influence on Use of Alcohol and antiretroviral therapy in South African couples. AIDS Behav. 2017;21(7):1885–91.
Brown JL, DeMartini KS, Sales JM, Swartzendruber AL, DiClemente RJ. Interventions to reduce alcohol use among HIV-infected individuals: a review and critique of the literature. Curr HIV/AIDS Rep. 2013;10(4):356–70.
Scott-Sheldon LA, Carey KB, Johnson BT, Carey MP, Team MR. Behavioral interventions targeting alcohol use among people living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. 2017;21(2):126–43.
Swann M. Economic strengthening for retention in HIV care and adherence to antiretroviral therapy: a review of the evidence. AIDS Care. 2018;30(sup3):85–98.
Swann M. Economic strengthening for HIV prevention and risk reduction: a review of the evidence. AIDS Care. 2018;30(sup3):37–84.
Allen H, Panetta D. Savings groups: what are they. Washington DC: SEEP Network; 2010. p. 2.
Ssewamala FM, Han C-K, Neilands TB. Asset ownership and health and mental health functioning among AIDS-orphaned adolescents: findings from a randomized clinical trial in rural Uganda. Soc Sci Med. 2009;69(2):191–8.
Bermudez LG, Ssewamala FM, Neilands TB et al. Does economic strengthening improve viral suppression among adolescents living with HIV? Results from a Cluster Randomized Trial in Uganda. AIDS Behav. 2018:1–10.
Ksoll C, Lilleør HB, Lønborg JH, Rasmussen OD. Impact of Village Savings and Loan associations: evidence from a cluster randomized trial. J Dev Econ. 2016;120:70–85.
Klostermann KC, Fals-Stewart W. Intimate partner violence and alcohol use: exploring the role of drinking in partner violence and its implications for intervention. Aggress Violent Beh. 2006;11(6):587–97.
Wechsberg WM, El-Bassel N, Carney T et al. Adapting an evidence-based HIV behavioral intervention for South African couples. Substance abuse treatment, prevention, and policy. 2015;10(1):6.
Operario D, Kuo C, Sosa-Rubí SG, Gálarraga O. Conditional economic incentives for reducing HIV risk behaviors: integration of psychology and behavioral economics. Health Psychol. 2013;32(9):932.
Darbes LA, McGrath NM, Hosegood V, et al. Results of a couples-based randomized controlled trial aimed to increase testing for HIV. JAIDS J Acquir Immune Defic Syndr. 2019;80(4):404–13.
Ssewamala FM, Bermudez LG, Neilands TB, et al. Suubi4Her: a study protocol to examine the impact and cost associated with a combination intervention to prevent HIV risk behavior and improve mental health functioning among adolescent girls in Uganda. BMC Public Health. 2018;18(1):693.
Ssewamala FM, Neilands TB, Waldfogel J, Ismayilova L. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. J Adolesc Health. 2012;50(4):346–52.
Conroy AA, Tebbetts S, Darbes LA et al. Development of an economic and relationship-strengthening intervention for Alcohol drinkers living with HIV in Malawi. AIDS Behav. 2022:1–16.
World Health Organization. Global status report on alcohol and health. Geneva, Switzerland: World Health Organization; 2014.
World Bank Group. Republic of Malawi Poverty Assessment. https://openknowledge.worldbank.org/handle/10986/26488. 2017.
UNCTAD. Access to Financial Services in Malawi: Policies and Challenges. 2014.
MDHS. Malawi demographic and health survey 2015-16. Maryland: NSO and ORC Macro; 2016.
World Health Organization. Researching violence against women: practical guidelines for researchers and activists. World Health Organization; 2005.
Juszczak E, Altman DG, Hopewell S, Schulz K. Reporting of multi-arm parallel-group randomized trials: extension of the CONSORT 2010 statement. JAMA. 2019;321(16):1610–20.
Babor TF, Higgins-Biddle JC, Organization WH. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. 2001.
Ministry of Health Malawi. 4rd Edition of the Malawi guidelines for Clinical Management of HIV in children and adults. Malawi: Lilongwe; 2018.
Silverman HJ, Miller FG. Control group selection in critical care randomized controlled trials evaluating interventional strategies: an ethical assessment. Crit Care Med. 2004;32(3):852–7.
Vickers AJ, de Craen AJ. Why use placebos in clinical trials? A narrative review of the methodological literature. J Clin Epidemiol. 2000;53(2):157–61.
Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide: version 3. 2007.
Sternberg RJ. Construct validation of a triangular love scale. Eur J Social Psychol. 1997;27(3):313–35.
Larzelere RE, Huston TL. The dyadic trust scale: toward understanding interpersonal trust in close relationships. J Marriage Fam. 1980:595–604.
Kurdek LA. The deterioration of relationship quality for gay and lesbian cohabiting couples: a five-year prospective longitudinal study. Personal Relationships. 1996;3(4):417–42.
Aron A, McLaughlin-Volpe T, Mashek D, et al. Including others in the self. Eur Rev Social Psychol. 2004;15(1):101–32.
Conroy AA, Ruark A, Neilands TB, et al. Development and validation of the couple sexual satisfaction scale for HIV and Sexual Health Research. Arch Sex Behav. 2021;50:3297–311.
Funk JL, Rogge RD. Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the couples satisfaction index. J Fam Psychol. 2007;21(4):572.
Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368(9543):1260–9.
Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. Adv Personal Relationships. 1987;1(1):37–67.
Christensen A, Shenk JL. Communication, conflict, and psychological distance in nondistressed, clinic, and divorcing couples. J Consult Clin Psychol. 1991;59(3):458.
Bradley KA, DeBenedetti AF, Volk RJ, et al. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcoholism: Clin Experimental Res. 2007;31(7):1208–17.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. Measuring alcohol consumption: Psychosocial and biochemical methods. 1992:41–72.
Conroy AA, McKenna S, Ruark A, et al. Relationship dynamics are Associated with Self-reported adherence but not an Objective Adherence measure in Malawi. AIDS Behav. 2022;26(11):3551–62.
Conroy AA, Leddy AM, Darbes LA, et al. Bidirectional violence is associated with poor engagement in HIV care and treatment in Malawian couples. J Interpers Violence. 2022;37(7–8):NP4258–77.
Gutin S, Jere J, Mulauzi N et al. Perceived impacts of Mlambe intervention on alcohol use, relationship dynamics, household economics, and HIV treatment adherence in Malawian couples. Presented at the AIDS Impact Conference, Stockholm, Sweden. June 12–14, 2023. 2023.
Jones J, Jones M, Plate C, Lewis D. The detection of 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphoethanol in human dried blood spots. Anal Methods. 2011;3(5):1101–6.
Hahn JA, Dobkin LM, Mayanja B, et al. Phosphatidylethanol (PEth) as a biomarker of alcohol consumption in HIV-positive patients in sub‐Saharan Africa. Alcoholism: Clin Experimental Res. 2012;36(5):854–62.
Ulwelling W, Smith K. The PEth blood test in the security environment: what it is; why it is important; and interpretative guidelines. J Forensic Sci. 2018;63(6):1634–40.
Helander A, Hansson T. National harmonization of the alcohol biomarker PEth. Lakartidningen. 2013;110(39–40):1747–8.
Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–9.
NIH/NCCIH. Pilot Studies: Common Uses and Misuses. Website: https://nccih.nih.gov/grants/whatnccihfunds/pilot_studies. 2017.
Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–9.
Moore CG, Carter RE, Nietert PJ, Stewart PW. Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci. 2011;4(5):332–7.
Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1.
Teresi JA, Yu X, Stewart AL, Hays RD. Guidelines for designing and evaluating feasibility pilot studies. Med Care. 2022;60(1):95–103.
Horton NJ, Kim E, Saitz R. A cautionary note regarding count models of alcohol consumption in randomized controlled trials. BMC Med Res Methodol. 2007;7(1):1–9.
Schramm B, Temfack E, Descamps D, et al. Viral suppression and HIV-1 drug resistance 1 year after pragmatic transitioning to dolutegravir first-line therapy in Malawi: a prospective cohort study. Lancet HIV. 2022;9(8):e544–53.
Hahn JA, Fatch R, Emenyonu NI, et al. Effect of two counseling interventions on self-reported alcohol consumption, alcohol biomarker phosphatidylethanol (PEth), and viral suppression among persons living with HIV (PWH) with unhealthy alcohol use in Uganda: a randomized controlled trial. Drug Alcohol Depend. 2023;244:109783.
Asiimwe C, Fatch R, Cheng DM, et al. Bar Attendance and Alcohol Use before and after COVID-19 related restrictions among HIV-infected adults in South-Western Uganda. AIDS Behav. 2023;27(6):2005–14.
UNAIDS. Understanding Fast-Track: accelerating action to end the AIDS epidemic by 2030. unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf. 2015.
Ruark AT, Darbes S, Neilands L, Hahn T, Mulauzi J, Mkandawire N, Ssewamala J, Conroy F. A. Mlambe economic and relationship-strengthening intervention increases relationship quality and decreases intimate partner violence among couples in Malawi. AIDS Impact Conference; Stockholm, Sweden. June 12-14.2023.
Swann M. Economic strengthening for retention in HIV care and adherence to antiretroviral therapy: a review of the evidence. AIDS Care. 2018;30(sup3):99–125.
Ssewamala FM, Sauceda JA, Brathwaite R, et al. Suubi + Adherence4Youth: a study protocol to optimize the Suubi intervention for adherence to HIV treatment for youth living with HIV in Uganda. BMC Public Health. 2023;23(1):717.
Funding
This study was funded by the National Institutes of Health under grants R34-AA027983 and K24-AA22586.
Author information
Authors and Affiliations
Contributions
AC led the conceptualization and design of this study, led the analysis, and drafted this manuscript. LD, JH, TN, JM, and FS conceptualized the study and edited the manuscript. ST, NM, and JM assisted with data collection and edited the manuscript. All authors contributed to the interpretation of findings and approved this manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the UCSF Human Research Protection Program (HRPP) and the National Health Sciences Research Committee (NHSRC) in Malawi.
Consent for Publication
All authors approve the publication of this manuscript.
Informed Consent
Informed consent was obtained from all participants included in the study.
Competing Interests
There are no conflicts of interest for any of the study authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Conroy, A.A., Hahn, J.A., Neilands, T.B. et al. Pilot Trial Results of Mlambe: An Economic and Relationship-Strengthening Intervention to Address Heavy Drinking and Adherence to Antiretroviral Therapy in Malawi. AIDS Behav (2024). https://doi.org/10.1007/s10461-024-04326-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s10461-024-04326-x