Abstract
Disclosure of HIV serostatus is beneficial for women, their partners, and their infants as it enables women to actively participate in preventative care (Hodgson et al. in PLoS ONE 9(11):e111421, 2014; Odiachi et al. in Reprod Health 15(1):36, 2018). Therefore, it is important that interventions addressing HIV prevention include elements that foster disclosure of HIV to partners. This study conducted in South Africa utilizes the “Protect Your Family” (PYF) behavioral intervention and compares Prevention of Mother to Child Transmission (PMTCT) among women participating in the program versus those in a control program. Within both groups, male partners were either present or not present for the intervention. The purpose of this study was to examine differential disclosure over time for individuals in the different conditions and partner involvement. A firth logistic regression revealed an interaction in the experimental condition with male partners participating (b = − 2.84, SE = 1.56, p = .012), in which female participants were less likely to disclose their HIV status over time. Findings from this study illustrate that additional efforts are needed to empower women to disclose their HIV status.
Resumen
Revelar su estado serológico del VIH a sus parejas es beneficioso para las mujeres, sus parejas y sus bebés, ya que les permite a las mujeres participar activamente en atención preventiva (Hodgson et al. in PLoS ONE 9(11):e111421, 2014; Odiachi et al. in Reprod Health 15(1):36, 2018). Por lo tanto, es importante que las intervenciones que aborden la prevención del VIH incluyan elementos que fomenten la revelación del estado serológico del VIH de las mujeres a sus parejas. Este estudio realizado en Sudáfrica utiliza la intervención conductual “Protege a tu familia” (PYF por sus siglas en Ingles) y compara la prevención de la transmisión de madre a hijo (PMTCT por sus siglas en Ingles) entre mujeres que participaron en el programa y las que participaron en un programa de control. Dentro de ambos grupos, los compañeros masculinos estuvieron presentes o no presentes para la intervención. El propósito de este estudio fue examinar la revelación diferente a lo largo del tiempo para individuos en diferentes condiciones y participación de pareja. Una regresión logística reveló de Firth una interacción en la condición experimental con la participación de parejas masculinas (b = − 2.84, SE = 1.56, p = .012), en las cuales las participantes femeninas tenían menos probabilidades de revelar su estado de VIH a lo largo del tiempo. Los resultados de este estudio ilustran que se necesitan esfuerzos adicionales para motivar a las mujeres a revelar su estado de VIH.


Similar content being viewed by others
References
UNAIDS; 2020. https://www.unaids.org/en/regionscountries/countries/southafrica.
Theuring S, Mbezi P, Luvanda H, Jordan-Harder B, Kunz A, Harms G. Male involvement in PMTCT services in Mbeya region, Tanzania. AIDS Behav. 2009;13(S1):92–102.
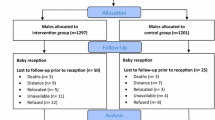
Jones D, Peltzer K, Weiss SM, et al. Implementing comprehensive prevention of mother-to-child transmission and HIV prevention for South African couples: study protocol for a randomized controlled trial (Medical condition overview). Trials. 2014;15(1):417.
Clouse K, Pettifor A, Shearer K, et al. Loss to follow-up before and after delivery among women testing HIV positive during pregnancy in Johannesburg, South Africa. Trop Med Int Health. 2013;18(4):451–60.
Ejigu Y, Tadesse B. HIV testing during pregnancy for prevention of mother-to-child transmission of HIV in Ethiopia. PLoS ONE. 2018;13(8):e0201886.
Bancheno WM, Mwanyumba F, Mareverwa J. Outcomes and challenges of scaling up comprehensive PMTCT services in rural Swaziland, Southern Africa. AIDS Care. 2010;22(9):1130–5.
Jones SA, Sherman Gg Fau-Varga CA, Varga CA. Exploring socio-economic conditions and poor follow-up rates of HIV-exposed infants in Johannesburg, South Africa. 2005(0954-0121 (Print)).
Mepham S, Zondi Z, Mbuyazi A, Mkhwanazi N, Newell ML. Challenges in PMTCT antiretroviral adherence in northern KwaZulu-Natal, South Africa. AIDS Care. 2011;23(6):741–7.
Tabana H, Doherty T, Swanevelder S, et al. Knowledge of HIV status prior to a community HIV counseling and testing intervention in a rural district of south Africa: results of a community based survey. BMC Infect Dis. 2012;12:73.
Ghoma-Linguissi L, Sidibe A, Thomas S, Poulain P, Ntoumi F. Factors influencing acceptability of voluntary HIV testing among pregnant women in Gamboma, Republic of Congo. BMC Res Notes. 2015;8:652.
Gourlay A, Birdthistle I, Mburu G, Iorpenda K, Wringe A. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother-to-child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16:18588.
Rice WS, Logie CH, Napoles TM, et al. Perceptions of intersectional stigma among diverse women living with HIV in the United States. Soc Sci Med. 2018;208:9–17.
Conkling M, Shutes EL, Karita E, et al. Couples’ voluntary counselling and testing and nevirapine use in antenatal clinics in two African capitals: a prospective cohort study. J Int AIDS Soc. 2010;13(1):10.
Brusamento S, Ghanotakis E, Tudor Car L, van-Velthoven MH, Majeed A, Car J. Male involvement for increasing the effectiveness of prevention of mother-to-child HIV transmission (PMTCT) programmes. Cochrane Database Syst Rev. 2012. https://doi.org/10.1002/14651858.CD009468.pub2/abstract.
Auvinen J, Suominen T, Välimäki M. Male participation and prevention of human immunodeficiency virus (HIV) mother-to-child transmission in Africa. Psychol Health Med. 2010;15(3):288–313.
Matseke MG, Ruiter RAC, Rodriguez VJ, Peltzer K, Setswe G, Sifunda S. Factors associated with male partner involvement in programs for the prevention of mother-to-child transmission of HIV in rural South Africa. Int J Environ Res Public Health. 2017;14(11):1333.
Ditekemena J, Koole O, Engmann C, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. 2012;9(1):1–8.
Amano A, Musa A. Male involvement in PMTCT and associated factors among men whom their wives had anc visit 12 months prior to the study in gondar town, North West Ethiopia, December, 2014. Pan Afr Med J. 2016;24.
Mucheto P, Chadambuka A, Shambira G, Tshimanga M, Notion G, Nyamayaro W. Determinants of nondisclosure of HIV status among women attending the prevention of mother to child transmission programme, Makonde district, Zimbabwe, 2009. Pan Afr Med J. 2011. https://doi.org/10.4314/pamj.v8i1.71169.
Orne-Gliemann J, Tchendjou PT, Miric M, et al. Couple-oriented prenatal HIV counseling for HIV primary prevention: an acceptability study. BMC Public Health. 2010;10:197.
Falnes EF, Moland KM, Tylleskär T, Paoli MM, Msuya SE, Engebretsen IM. “It is her responsibility”: partner involvement in prevention of mother to child transmission of HIV programmes, northern Tanzania. J Int AIDS Soc. 2011;14(1):21.
Hodgson I, Plummer ML, Konopka SN, et al. A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS ONE. 2014;9(11):e111421.
Odiachi A, Erekaha S, Cornelius LJ, et al. HIV status disclosure to male partners among rural Nigerian women along the prevention of mother-to-child transmission of HIV cascade: a mixed methods study. Reprod Health. 2018;15(1):36.
Stringer EM, Chi BH, Chintu N, et al. Monitoring effectiveness of programmes to prevent mother-to-child HIV transmission in lower-income countries. Bull World Health Org. 2008;86(1):57.
Spangler AS, Onono AM, Bukusi RE, Cohen MC, Turan MJ. HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. JAIDS J Acquir Immune Defic Syndr. 2014;67 Suppl 4(Suppl 4):S235–42.
Skinner D, Mfecane S. Stigma, discrimination and the implications for people living with HIV/AIDS in South Africa. Sahara J. 2004;1(3):157–64.
Simbayi LC, Kalichman SC, Strebel A, Cloete A, Henda N, Mqeketo A. Disclosure of HIV status to sex partners and sexual risk behaviours among HIV-positive men and women, Cape Town, South Africa. Sex Transm Infect. 2007;83(1):29.
Visser MJ, Neufeld S, de Villiers A, Makin JD, Forsyth BWC. To tell or not to tell: South African women’s disclosure of HIV status during pregnancy. AIDS Care. 2008;20(9):1138–45.
Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Org. 2004;82(4):299–307.
Abler L, Sikkema KJ, Watt MH, Hansen NB, Wilson PA, Kochman A. Depression and HIV serostatus disclosure to sexual partners among newly HIV-diagnosed men who have sex with men. AIDS Patient Care STDs. 2015;29(10):550–8.
Nacius LA, Levison J, Minard CG, Fasser C, Davila JA. Serodiscordance and disclosure among HIV-positive pregnant women in the Southwestern United States. AIDS Patient Care STDs. 2013;27(4):242–7.
Farquhar AC, Mbori-Ngacha KD, Bosire WR, Nduati KR, Kreiss CJ, John CG. Partner notification by HIV-1 seropositive pregnant women: association with infant feeding decisions. AIDS. 2001;15(6):815–7.
Kalichman S, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med. 2003;26(4):315–32.
National Department of Health—Republic of South Africa. National Consolidated Guidelines for the prevention of mother-to-child transmission of HIV (PMTCT) and the management of HIV in children, adolescents, and adults; 2015.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–6.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29.
Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–77.
Heinze G, Schemper M. A solution to the problem of separation in logistic regression. Stat Med. 2002;21(16):2409–19.
Puhr R, Heinze G, Nold M, Lusa L, Geroldinger A. Firth’s logistic regression with rare events: accurate effect estimates and predictions? Stat Med. 2017;36(14):2302–17.
Ramlagan S. Understanding ART adherence: exploring the structural and psychosocial determinants of antiretroviral therapy adherence among pregnant women in Mpumalanga Province, South Africa. Maastricht: ProefschriftMaken; 2019.
Tam M, Amzel A, Phelps BR. Disclosure of HIV serostatus among pregnant and postpartum women in sub-Saharan Africa: a systematic review. AIDS Care. 2015;27(4):436–50.
Moses S, Tomlinson M. The fluidity of disclosure: a longitudinal exploration of women’s experience and understanding of HIV disclosure in the context of pregnancy and early motherhood. AIDS Care. 2013;25(6):667–75.
Funding
This study was funded by a Grant from NIH, R01HD078187, and with the support of the University of Miami Miller School of Medicine Center for AIDS Research, funded by an NIH Grant, P30AI073961.
Author information
Authors and Affiliations
Contributions
JA and Dr. TKL performed the data analysis, and worked on the methods and results section. MP wrote the introduction. Dr. SR wrote the discussion. Dr. SS reviewed the manuscript and provided editing. Dr. SMW, Dr. KP, and Dr. DLJ were involved in study design.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Prior to study onset, ethical approval was obtained from the Mpumalanga Department of Health, the Human Sciences Research Council (HSRC) and the University of Miami (UM) Institutional Review Board. Ethical approval for the study was procured from the Human Sciences Research Council (HSRC) Research Ethics Committee (REC) (Number: REC4/21/08/13), the Department of Health and Welfare, Mpumalanga Provincial Government, and the University of Miami Miller School of Medicine Institutional Review Board (IRBID: 20130238). The study was registered as a clinical trial on clinicaltrials.gov, Number NCT02085356.
Research Involved in Human and Animal Rights
Human Participants All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abbamonte, J.M., Parrish, M.S., Lee, T.K. et al. Influence of Male Partners on HIV Disclosure Among South African Women in a Cluster Randomized PMTCT Intervention. AIDS Behav 25, 604–614 (2021). https://doi.org/10.1007/s10461-020-03021-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-03021-x