Abstract
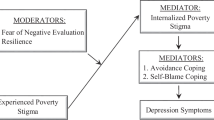
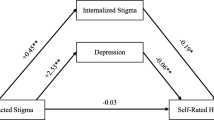
Pain is common in women with HIV, though little research has focused on psychosocial experiences contributing to pain in this population. In the present study we examined whether internalized HIV stigma predicts pain, and whether depressive symptoms mediate this relationship among women with HIV. Data were drawn from the Women’s Interagency HIV Study (WIHS), for 1,364 women with HIV who completed three study visits between 2015 and 2016. We used a sequential longitudinal design to assess the relationship between internalized HIV stigma at time 1 on pain at time 3 through depressive symptoms at time 2. Analyses revealed internalized HIV stigma was prospectively associated with greater pain, B = 5.30, 95% CI [2.84, 7.60]. The indirect effect through depressive symptoms supported mediation, B = 3.68, 95% CI [2.69, 4.79]. Depression is a modifiable risk factor that can be addressed to improve pain prevention and intervention for women with HIV.

Similar content being viewed by others
References
Hasse B, Ledergerber B, Furrer H, et al. Morbidity and aging in HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis. 2011;53(11):1130–9. https://doi.org/10.1093/cid/cir626.
Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. The Lancet. 2013;382(9903):1525–33. https://doi.org/10.1016/S0140-6736(13)61809-7.
Balderson BH, Grothaus L, Harrison RG, McCoy K, Mahoney C, Catz S. Chronic illness burden and quality of life in an aging HIV population. AIDS Care. 2013;25(4):451–8. https://doi.org/10.1080/09540121.2012.712669.
Merlin J. Chronic pain in patients with HIV infection: what clinicians need to know. Top Antivir Med. 2015;23(3):120–4.
Goodin BR, Owens MA, White DM, et al. Intersectional health-related stigma in persons living with HIV and chronic pain: implications for depressive symptoms. AIDS Care. 2018;30(sup2):66–73. https://doi.org/10.1080/09540121.2018.1468012.
Merlin JS, Westfall AO, Raper JL, et al. Pain, Mood, and Substance Abuse in HIV. JAIDS. 2012;61(2):164–70. https://doi.org/10.1097/QAI.0b013e3182662215.
Miaskowski C, Penko JM, Guzman D, Mattson JE, Bangsberg DR, Kushel MB. Occurrence and characteristics of chronic pain in a community-based cohort of indigent adults living with HIV infection. J Pain. 2011;12(9):1004–166. https://doi.org/10.1016/j.jpain.2011.04.002.
Richardson JL, Heikes B, Karim R, Weber K, Anastos K, Young M. Experience of pain among women with advanced HIV disease. AIDS Patient Care STDS. 2009;23(7):503–11. https://doi.org/10.1089/apc.2008.0128.
Jiao JM, So E, Jebakumar J, George MC, Simpson DM, Robinson-Papp J. Chronic pain disorders in HIV primary care: clinical characteristics and association with healthcare utilization. Pain. 2016;157(4):931–7. https://doi.org/10.1097/j.pain.0000000000000462.
Sharma A, Hoover DR, Shi Q, et al. Frequent occurrence of pain and prescription opioid use for treatment of pain among women with and at risk for HIV infection. AIDS Behav. 2018;22(6):2008–177. https://doi.org/10.1007/s10461-017-1828-0.
Goodin BR, Owens MA, Yessick LR, et al. Detectable Viral Load May Be Associated with Increased Pain Sensitivity in Persons Living with HIV: Preliminary Findings. Pain Med. 2017;18(12):2289–95. https://doi.org/10.1093/pm/pnx057.
Merlin JS, Zinski A, Norton WE, et al. A conceptual framework for understanding chronic pain in patients with HIV. Pain Pract. 2014;14(3):207–16. https://doi.org/10.1111/papr.12052.
Merlin JS, Westfall AO, Chamot E, et al. Pain is independently associated with impaired physical function in HIV-infected patients. Pain Med. 2013;14(12):1985–93. https://doi.org/10.1111/pme.12255.
Merlin JS, Westfall AO, Raper JL, et al. Pain, mood, and substance abuse in HIV: implications for clinic visit utilization, ART adherence, and virologic failure. JAIDS. 2012;61(2):164–70. https://doi.org/10.1097/QAI.0b013e3182662215.
Surratt HL, Kurtz SP, Levi-Minzi MA, Cicero TJ, Tsuyuki K, O'grady CL. Pain treatment and antiretroviral medication adherence among vulnerable HIV-positive patients. AIDS Patient Care STDs. 2015; 29(4): 186–192.
Aouizerat BE, Miaskowski CA, Gay C, et al. Risk factors and symptoms associated with pain in HIV-infected adults. J Assoc Nurses AIDS Care. 2010;21(2):125–33. https://doi.org/10.1016/j.jana.2009.10.003.
Parker R, Stein DJ, Jelsma J. Pain in people living with HIV/AIDS: a systematic review. J Int AIDS Soc. 2014;17(1):18719. https://doi.org/10.7448/IAS.17.1.18719.
Scott W, Arkuter C, Kioskli K, et al. Psychosocial factors associated with persistent pain in people with HIV: a systematic review with meta-analysis. Pain. 2018;159(12):2461–76. https://doi.org/10.1097/j.pain.0000000000001369.
DeWall CN, MacDonald G, Webster GD, et al. Acetaminophen reduces social pain: behavioral and neural evidence. Psychol Sci. 2010;21(7):931–7. https://doi.org/10.1177/0956797610374741.
MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychol Bull. 2005;131(2):202–23. https://doi.org/10.1037/0033-2909.131.2.202.
Kross E, Berman MG, Mischel W, Smith EE, Wager TD. Social rejection shares somatosensory representations with physical pain. Proc Natl Acad Sci USA. 2011;108(15):6270–5. https://doi.org/10.1073/pnas.1102693108.
Woo C-W, Koban L, Kross E, et al. Separate neural representations for physical pain and social rejection. Nat Commun. 2014;5:5380. https://doi.org/10.1038/ncomms6380.
Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27(1):363–85.
Mahajan AP, Sayles JN, Patel VA, et al. Stigma in the HIV/AIDS epidemic: a review of the literature and recommendations for the way forward. AIDS. 2008;22(Suppl 2):S67–S79. https://doi.org/10.1097/01.aids.0000327438.13291.62.
Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. 2013;103(5):813–21. https://doi.org/10.2105/AJPH.2012.301069.
Wadley AL, Pincus T, Evangeli M. A preliminary analysis of the association between perceived stigma and HIV-related pain. Afr J Prim Health Care Fam Med. 2019;11(1):e1–e5. https://doi.org/10.4102/phcfm.v11i1.1647.
Turan B, Crockett KB, Buyukcan-Tetik A, et al. Buffering internalization of HIV stigma: implications for treatment adherence and depression. JAIDS. 2019;80(3):284–91. https://doi.org/10.1097/QAI.0000000000001915.
Turan B, Hatcher AM, Weiser SD, Johnson MO, Rice WS, Turan JM. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health. 2017;107(6):863–9. https://doi.org/10.2105/AJPH.2017.303744.
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160.
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–95. https://doi.org/10.1007/s10461-013-0437-9.
Boone MR, Cook SH, Wilson PA. Sexual identity and HIV status influence the relationship between internalized stigma and psychological distress in black gay and bisexual men. AIDS Care. 2016;28(6):764–70. https://doi.org/10.1080/09540121.2016.1164801.
Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town. South Africa Soc Sci Med. 2007;64(9):1823–31. https://doi.org/10.1016/j.socscimed.2007.01.006.
Mak WW, Poon CY, Pun LY, Cheung SF. Meta-analysis of stigma and mental health. Soc Sci Med. 2007;65(2):245–61. https://doi.org/10.1016/j.socscimed.2007.03.015.
Turan B, Rice WS, Crockett KB, et al. Longitudinal association between internalized HIV stigma and antiretroviral therapy adherence for women living with HIV: the mediating role of depression. AIDS. 2019;33(3):571–6. https://doi.org/10.1097/QAD.0000000000002071.
Crockett KB, Kalichman SC, Kalichman MO, Cruess DG, Katner HP. Experiences of HIV-related discrimination and consequences for internalised stigma, depression and alcohol use. Psychol Health. 2019;34(7):796–810. https://doi.org/10.1080/08870446.2019.1572143.
Turan B, Smith W, Cohen MH, et al. Mechanisms for the negative effects of internalized HIV-related stigma on antiretroviral therapy adherence in women: the mediating roles of social isolation and depression. JAIDS. 2016;72(2):198–205. https://doi.org/10.1097/QAI.0000000000000948.
Chang MH, Hsu JW, Huang KL, et al. Bidirectional association between depression and fibromyalgia syndrome: a nationwide longitudinal study. J Pain. 2015;16(9):895–902. https://doi.org/10.1016/j.jpain.2015.06.004.
Elliot TE, Renier CM, Palcher JA. Chronic pain, depression, and quality of life: correlations and predictive value of the SF-36. Pain Med. 2003;4(4):331–9. https://doi.org/10.1111/j.1526-4637.2003.03040.x.
Arnow BA, Hunkeler EM, Blasey CM, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68(2):262–8. https://doi.org/10.1097/01.psy.0000204851.15499.fc.
Carr EC, Nicky Thomas V, Wilson-Barnet J. Patient experiences of anxiety, depression and acute pain after surgery: a longitudinal perspective. Int J Nurs Stud. 2005;42(5):521–30. https://doi.org/10.1016/j.ijnurstu.2004.09.014.
Moayedi M, Davis KD. Theories of pain: from specificity to gate control. J Neurophysiol. 2012;109(1):5–12. https://doi.org/10.1152/jn.00457.2012.
Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581–624. https://doi.org/10.1037/0033-2909.133.4.581.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45. https://doi.org/10.1001/archinte.163.20.2433.
Adimora AA, Ramirez C, Benning L, et al. Cohort profile: the women’s interagency HIV study (WIHS). Int J Epidemiol. 2018;47(2):393–394i. https://doi.org/10.1093/ije/dyy021.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29.
Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007;19(3):198–208. https://doi.org/10.1521/aeap.2007.19.3.198.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188(10):662–70. https://doi.org/10.1097/00005053-200010000-00004.
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;473–483.
Muthén LK, Muthén BO. Mplus. The comprehensive modelling program for applied researchers: user’s guide. Muthén & Muthén, 1998.
MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104.
Velly AM, Mohit S. Epidemiology of pain and relation to psychiatric disorders. Prog Neuropsychopharmacol Biol Psychiatry. 2018;87:159–67.
Ebirim LN, Otokwala JG. Inadequate pain relief in ambulatory patients with human immunodeficiency virus disease in Port Harcourt. HIV AIDS. 2013;5:199–203. https://doi.org/10.2147/HIV.S45150.
Smith D, Wilkie R, Uthman O, Jordan JL, McBeth J. Chronic pain and mortality: a systematic review. PLoS ONE. 2014;9(6):e99048. https://doi.org/10.1371/journal.pone.0099048.
Baugher AR, Beer L, Fagan JL, et al. Prevalence of internalized HIV-related stigma among HIV-infected adults in care, United States, 2011–2013. AIDS Behav. 2017;21(9):2600–2608.
Pantelic M, Sprague L, Stangl AL. It’s not “all in your head”: critical knowledge gaps on internalized HIV stigma and a call for integrating social and structural conceptualizations. BMC Infect Dis. 2019;19(1):210. https://doi.org/10.1186/s12879-019-3704-1.
Dworkin RH, O’connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237–251.
Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry. 2009;31(3):206–19. https://doi.org/10.1016/j.genhosppsych.2008.12.006.
Noble M, Treadwell JR, Tregear SJ, et al. Long-term opioid management for chronic noncancer pain. Cochrane Database Syst Rev. 2010;(1):CD006605.
Semenkovich K, Chockalingam R, Scherrer JF, et al. Prescription opioid analgesics increase risk of major depression: new evidence, plausible neurobiological mechanisms and management to achieve depression prophylaxis. Mo Med. 2014;111(2):148–54.
Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic non-cancer pain: the role of opioid prescription. Clin J Pain. 2014;30(7):557–64.
Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315–1321.
Ehde DM, Dillworth TM, Turner JA. Cognitive-behavioral therapy for individuals with chronic pain: efficacy, innovations, and directions for research. Am Psychol. 2014;69(2):153–66. https://doi.org/10.1037/a0035747.
Merlin JS, Westfall AO, Long D, et al. A randomized pilot trial of a novel behavioral intervention for chronic pain tailored to individuals with HIV. AIDS Behav. 2018;22(8):2733–42. https://doi.org/10.1007/s10461-018-2028-2.
Turan JM, Elafros MA, Logie CH, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019;17(1):7. https://doi.org/10.1186/s12916-018-1246-9.
Funding
Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS). WIHS (Principal Investigators): UAB-MS WIHS (Mirjam-Colette Kempf and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos and Anjali Sharma), U01-AI-035004; Brooklyn WIHS (Deborah Gustafson and Tracey Wilson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Seble Kassaye and Daniel Merenstein), U01-AI-034994; Miami WIHS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women’s HIV Study, Northern California (Bradley Aouizerat and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Joel Milam), U01-HD-032632 (WIHS I—WIHS IV). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and other Communication Disorders (NIDCD), and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA), P30-AI-050409 (Atlanta CFAR), P30-AI-050410 (UNC CFAR), and P30-AI-027767 (UAB CFAR). Additional support for software was provided by the National Institute on Minority Health and Health Disparities under Award Number U54MD000502. This research was also supported by K12HL143958, an NIH funded grant made possible through the NHLBI. The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
No conflicts of interest were reported by the authors of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Crockett, K.B., Esensoy, T.A., Johnson, M.O. et al. Internalized HIV Stigma and Pain among Women with HIV in the United States: The Mediating Role of Depressive Symptoms. AIDS Behav 24, 3482–3490 (2020). https://doi.org/10.1007/s10461-020-02919-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-020-02919-w