Abstract
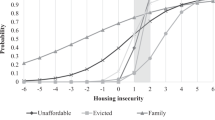
Despite greater mental health co-morbidities and heavier alcohol use among PLWH, few studies have examined the role of the neighborhood alcohol environment on either alcohol consumption or mental health. Utilizing cross-sectional data from a cohort study in a southern U.S. metropolitan area, we examine the association between neighborhood alcohol environments on hazardous drinking and mental health among 358 in-care PLWH (84% African American, 31% female). Multilevel models were utilized to quantify associations between neighborhood alcohol exposure on hazardous drinking and effect modification by sex. Neighborhood alcohol density was associated with hazardous drinking among men but not women. Women living in alcohol dense neighborhoods were nearly two-fold likely to report depression compared to those in less dense neighborhoods, with no association between neighborhood alcohol density and depression among men. Neighborhood alcohol environments may be an important contextual factor to consider in reducing heavy alcohol consumption and improving mental health among PLWH.
Resumen
Aunque el uso de alcohol y los trastornos mentales son muy comunes en las personas que viven con VIH, muy pocos estudios han investigado el contexto social, específicamente las características del expendio de alcohol, en relación con su consumo y la salud mental de la población. Utilizando datos transversales de un estudio de cohorte de personas viviendo con VIH en un área metropolitana del Sur de Los Estados Unidos, nosotros examinamos la asociación entre las características del expendio de alcohol al nivel vecinal y el consumo de alcohol y la salud mental en 358 personas que viven con VIH (84% afroamericanos, 31% mujeres). Utilizamos modelos jerárquicos para examinar y cuantificar asociaciones entre el expendio de alcohol al nivel vecinal y el alto consumo de alcohol y un posible efecto de modificación por sexo. Encontramos que la densidad de establecimientos que expenden alcohol en el vecindario se asocia con un alto consumo de alcohol en los hombres, pero no así en las mujeres. Mujeres que viven en vecindarios caracterizados por una alta densidad de expendio de alcohol son dos veces más propensas a reportar depresión que aquellas que no viven en vecindarios con densidad alta. No hubo una asociación entre la densidad de expendio de alcohol a nivel vecinal y depresión en los hombres. Las características del expendio de alcohol en un vecindario puede ser un factor importante para reducir el alto consumo de alcohol y mejorar la salud mental en las personas que viven con VIH.
Similar content being viewed by others
References
El-Sadr WM, Mayer KH, Hodder SL. AIDS in America—forgotten but not gone. N Engl J Med. 2010;362(11):967.
Gant Z, Lomotey M, Hall H, Hu X, Guo X, Song R. A county-level examination of the relationship between HIV and social determinants of health: 40 states, 2006-2008. Open AIDS J. 2012;6:1.
Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the US HIV epidemic. Am Psychol. 2013;68(4):197.
Auerbach JD, Parkhurst JO, Cáceres CF. Addressing social drivers of HIV/AIDS for the long-term response: conceptual and methodological considerations. Glob Public Health. 2011;6(sup3):S293–309.
Eberhart MG, Yehia BR, Hillier A, Voytek CD, Blank M, Frank I, et al. Behind the cascade: analyzing spatial patterns along the HIV care continuum. J Acquir Immune Defic Syndr (1999). 2013;64(0 1):S42.
Ironson G, Stuetzle R, Fletcher M. An increase in religiousness/spirituality occurs after HIV diagnosis and predicts slower disease progression over 4 years in people with HIV. J Gen Intern Med. 2006;21(Supplement 5):S62–8.
Leserman J. HIV disease progression: depression, stress, and possible mechanisms. Biol Psychiatry. 2003;54(3):295–306.
Leserman J, Petitto JM, Golden RN, Gaynes BN, Gu H, Perkins DO, et al. Impact of stressful life events, depression, social support, coping, and cortisol on progression to AIDS. Am J Psychiatry. 2000;157(8):1221–8.
Wong MD, Sarkisian CA, Davis C, Kinsler J, Cunningham WE. The association between life chaos, health care use, and health status among HIV-infected persons. J Gen Intern Med. 2007;22(9):1286–91.
Siemieniuk RA, Krentz HB, Miller P, Woodman K, Ko K, Gill MJ. The clinical implications of high rates of intimate partner violence against HIV-positive women. JAIDS J Acquir Immune Defic Syndr. 2013;64(1):32–8.
Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72(8):810.
Gorman DM, Speer PW. The concentration of liquor outlets in an economically disadvantaged city in the northeastern United States. Subst Use Misuse. 1997;32(14):2033–46.
Latkin C, Glass GE, Duncan T. Using geographic information systems to assess spatial patterns of drug use, selection bias and attrition among a sample of injection drug users. Drug Alcohol Depend. 1998;50(2):167–75.
Scribner R, Theall KP, Simonsen N, Robinson W. HIV risk and the alcohol environment: advancing an ecological epidemiology for HIV/AIDS. Alcohol Res Health. 2010;33(3):179.
Theall KP, Scribner R, Cohen D, Bluthenthal RN, Schonlau M, Farley TA. Social capital and the neighborhood alcohol environment. Health & Place. 2009;15(1):323–32.
Popova S, Giesbrecht N, Bekmuradov D, Patra J. Hours and days of sale and density of alcohol outlets: impacts on alcohol consumption and damage: a systematic review. Alcohol Alcohol. 2009;44(5):500–16.
Pereira G, Wood L, Foster S, Haggar F. Access to alcohol outlets, alcohol consumption and mental health. PLoS ONE. 2013;8(1):e53461.
Arnold M, Hsu L, Pipkin S, McFarland W, Rutherford GW. Race, place and AIDS: the role of socioeconomic context on racial disparities in treatment and survival in San Francisco. Soc Sci Med. 2009;69(1):121–8.
Joy R, Druyts EF, Brandson EK, Lima VD, Rustad CA, Zhang W, et al. Impact of neighborhood-level socioeconomic status on HIV disease progression in a universal health care setting. JAIDS J Acquir Immune Defic Syndr. 2008;47(4):500–5.
Kelly JA, Murphy DA, Bahr GR, Koob JJ, Morgan MG, Kalichman SC, et al. Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychol. 1993;12(3):215.
Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: a social ecological approach to prevention and care. Am Psychol. 2013;68(4):210.
Pence BW, Mugavero MJ, Carter TJ, Leserman J, Thielman NM, Raper JL, et al. Childhood trauma and health outcomes in HIV-infected patients: an exploration of causal pathways. JAIDS J Acquir Immune Defic Syndr. 2012;59(4):409–16. https://doi.org/10.1097/QAI.0b013e31824150bb.
Reif S, Mugavero M, Raper J, Thielman N, Leserman J, Whetten K, et al. Highly stressed: stressful and traumatic experiences among individuals with HIV/AIDS in the Deep South. AIDS Care. 2011;23(2):152–62.
Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8.
Pence BW, Miller WC, Whetten K, Eron JJ, Gaynes BN. Prevalence of DSM-IV-defined mood, anxiety, and substance use disorders in an HIV clinic in the Southeastern United States. JAIDS J Acquir Immune Defic Syndr. 2006;42(3):298–306.
Applebaum AJ, Bedoya CA, Hendriksen ES, Wilkinson JL, Safren SA, O’Cleirigh C. Future directions for interventions targeting PTSD in HIV-infected adults. J Assoc Nurses AIDS Care. 2015;26(2):127–38.
Haubrich RH, Little SJ, Currier JS, Forthal DN, Kemper CA, Beall GN, et al. The value of patient-reported adherence to antiretroviral therapy in predicting virologic and immunologic response. AIDS. 1999;13(9):1099–107.
Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133(1):21–30.
Gordillo V, del Amo J, Soriano V, González-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13(13):1763–9.
Applebaum A, Richardson M, Brady S, Brief D, Keane T. Gender and other psychosocial factors as predictors of adherence to highly active antiretroviral therapy (HAART) in adults with comorbid HIV/AIDS, psychiatric and substance-related disorder. AIDS Behav. 2015;13(1):1–6.
O’Cleirigh C, Valentine S, Pinkston M, Herman D, Bedoya C, Gordon J, et al. The unique challenges facing HIV-positive patients who smoke cigarettes: HIV viremia, art adherence, engagement in HIV care, and concurrent substance use. AIDS Behav. 2015;19(1):178–85.
Galvan FH, Bing EG, Fleishman JA, London AS, Caetano R, Burnam MA, et al. The prevalence of alcohol consumption and heavy drinking among people with HIV in the United States: results from the HIV Cost and Services Utilization Study. J Stud Alcohol. 2002;63(2):179–86.
Bensley KM, McGinnis KA, Fortney J, Chan KCG, Dombrowski JC, Ornelas I, et al. Patterns of alcohol use among patients living with HIV in urban, large rural, and small rural areas. J Rural Health. 2018;35(3):330–40.
Bilal U, McCaul ME, Crane HM, Mathews WC, Mayer KH, Geng E, et al. Predictors of longitudinal trajectories of alcohol consumption in people with HIV. Alcohol Clin Exp Res. 2018;42(3):561–70.
Crane HM, McCaul ME, Chander G, Hutton H, Nance RM, Delaney JAC, et al. Prevalence and factors associated with hazardous alcohol use among persons living with HIV across the US in the current era of antiretroviral treatment. AIDS Behav. 2017;21(7):1914–25.
Machtinger E, Wilson T, Haberer J, Weiss D. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav. 2012;16(8):2091–100.
Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, et al. Prevalence and treatment of mental disorders, 1990 to 2003. N Engl J Med. 2005;352(24):2515–23.
Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighbourhood environment. Soc Sci Med. 2005;60(8):1681–92.
Derose KP, Han B, Williamson S, Cohen DA. Gender disparities in park use and physical activity among residents of high-poverty neighborhoods in Los Angeles. Women’s Health Issues. 2018;28(1):6–13.
Theall KP, Lancaster BP, Lynch S, Haines RT, Scribner S, Scribner R, et al. The neighborhood alcohol environment and at-risk drinking among African-Americans. Alcohol Clin Exp Res. 2011;35(5):996–1003.
Welsh D, Ferguson T, Theall K, Simon L, Amedee A, Siggins R, et al. The New Orleans Alcohol Use in HIV [NOAH] Study: A translational investigation of alcohol use, biological and socioenvironmental mechanisms, and geriatric multi-morbidity in people living with HIV. (under review).
Saunders JB, Aasland OG, Babor TF, Delafuente JR, Grant M. Development of the alcohol-use disorders identification test (Audit)—who collaborative project on early detection of persons with harmful alcohol-consumption. 2. Addiction. 1993;88(6):791–804.
Bohn MJ, Babor TF, Kranzler HR. The alcohol-use disorders identification test (Audit)—validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56(4):423–32.
Valladolid GR, Vicedo JB, Sanchez-Serrano MCC, Carrasco JSD. Validation of the alcohol use disorders identification test (AUDIT) in primary care. Rev Clin Esp. 1998;198(1):11–4.
Tang YL, Jovanovic T, Wingo A, Michopoulos V, Schwartz A, Ressler KJ. Validation of the alcohol use disorders identification test (AUDIT) in an inner city primary care sample. Biol Psychiatry. 2015;77(9):374S-374S.
Lundin A, Hallgren M, Balliu N, Forsell Y. The use of alcohol use disorders identification test (AUDIT) in detecting alcohol use disorder and risk drinking in the general population: validation of AUDIT using schedules for clinical assessment in neuropsychiatry. Alcohol Clin Exp Res. 2015;39(1):158–65.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Snaith RP. The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes. 2003;1:29.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77.
Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162(3):199–200.
Kalichman SC, Kalichman MO, Cherry C. Forget about forgetting: structural barriers and severe non-adherence to antiretroviral therapy. AIDS Care. 2017;29(4):418–22.
Vagenas P, Azar MM, Copenhaver MM, Springer SA, Molina PE, Altice FL. The impact of alcohol use and related disorders on the HIV continuum of care: a systematic review. Curr HIV/AIDS Rep. 2015;12(4):421–36.
Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–71.
Theall K, Scribner R, Ghosh-Dastidar B, Cohen D, Mason K, Simonsen N. Neighbourhood alcohol availability and gonorrhea rates: impact of social capital. Geospatial Health. 2009;3(2):241–55.
Theall K, Scribner R, Cohen D, Blumenthal R, Schonlau M, Farley T. Social capital and the neighborhood alcohol environment. Health Place. 2009;15:323–32.
Theall KP, Scribner R, Cohen D, Bluthenthal RN, Schonlau M, Lynch S, et al. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol Alcohol. 2009;44(5):491–9.
Eberhart MG, Yehia BR, Hillier A, Voytek CD, Fiore DJ, Blank M, et al. Individual and community factors associated with geographic clusters of poor HIV care retention and poor viral suppression. JAIDS J Acquir Immune Defic Syndr. 2015;69:S37–43.
Shacham E, Lian M, Önen N, Donovan M, Overton E. Are neighborhood conditions associated with HIV management? HIV Med. 2013;14(10):624–32.
Kalichman SC, Pellowski J, Kalichman MO, Cherry C, Detorio M, Caliendo AM, et al. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prev Sci. 2011;12(3):324.
Gorman DM, Speer PW, Gruenewald PJ, Labouvie EW. Spatial dynamics of alcohol availability, neighborhood structure and violent crime. J Stud Alcohol. 2001;62(5):628–36.
Scribner RA, Cohen DA, Kaplan S. Alcohol availability and homicide in New Orleans: conceptual considerations for small area analysis of the effect of alcohol outlet density. J Stud Alcohol. 1999;60:310–6.
Livingston M. Alcohol outlet density and harm: comparing the impacts on violence and chronic harms. Drug Alcohol Rev. 2011;30(5):515–23.
Theall K, Scribner R, Cohen D, Blumenthal R, Farley T. The neighborhood alcohol environment and alcohol-related morbidity. Alcohol Alcohol. 2009;44(5):491–9.
Dohrenwend BS, Dohrenwend BP. Some issues in research on stressful life events. Handbook of clinical health psychology. New York: Springer; 1982. p. 91–102.
Dohrenwend BP. Mental illness in the United States: epidemiological estimates. New York: Praeger Publishers; 1980.
LaVeist TA. Racial segregation and longevity among African Americans: an individual-level analysis. Health Serv Res. 2003;38(6p2):1719–34.
Acknowledgements
We thank the research subjects for their willingness to participate. We acknowledge the hard work and time devoted by study staff, and referring clinicians. They are key to the success of the study. The authors recognize the contributions of study personnel Mary Meyaski-Schluter, RN, and Virginia Garrison, RN. The study was supported by grants from the National Institutes of Health (NIH, P60AA009803). This study was approved by the Tulane University and Louisiana State University Health Sciences Center Institutional Review Boards. The data were collected in compliance with ethical standards regarding treatment of human participants. All authors have contributed significantly to the manuscript, approved the submission of this version, and consent to having their names on the manuscript. No form of payment was given to anyone to produce the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Theall, K.P., Wallace, M., Felker-Kantor, E. et al. Neighborhood Alcohol Environment: Differential Effects on Hazardous Drinking and Mental Health by Sex in Persons Living with HIV (PLWH). AIDS Behav 23, 3237–3246 (2019). https://doi.org/10.1007/s10461-019-02632-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-019-02632-3