Abstract
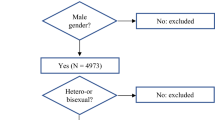
Among persons who inject drugs, women have a higher HIV prevalence (than men) in many settings. Understanding how gender affects risk for infection among HIV-negative, and transmission among HIV-positive people who currently or previously injected drugs is key to designing effective prevention and treatment programs. We analyzed data from 291 persons living with HIV who had ever injected drugs. Participants were drawn from the Russia Alcohol Research Collaboration on HIV/AIDS cohort (2012–2015) to examine associations between female gender and HIV transmission risk. Primary outcomes were sharing drug injecting equipment (e.g., needle/syringes) and condomless sex. Secondary outcomes were alcohol use before sharing drug injecting equipment; before condomless sex; and both sharing drug injecting equipment and condomless sex. Logistic regression models assessed associations between gender and outcomes, controlling for demographics, partner HIV status and use of antiretroviral treatment. Female gender was not significantly associated with sharing drug injecting equipment [aOR = 1.45, 95% confidence interval (CI) 0.85–2.46, p value = 0.18] but was associated with condomless sex (aOR = 1.91, 95% CI 1.12–3.23, p = 0.02) in adjusted models. Female gender was not significantly associated with any secondary outcomes. Better understanding of risky sex and drug use behaviors among people who currently or previously injected drugs can support the design of effective gender-tailored HIV prevention interventions.
Similar content being viewed by others
References
Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1564–74.
Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet (Lond Engl). 2008;372(9651):1733–45.
Kozlov AP, Shaboltas AV, Toussova OV, Verevochkin SV, Masse BR, Perdue T, et al. HIV incidence and factors associated with HIV acquisition among injection drug users in St. Petersburg, Russia. AIDS (Lond Engl). 2006;20(6):901–6.
United Nations Office on Drugs and Crime. World drug report 2015. New York: United Nations; 2015.
Gökengin D, Oprea C, Uysal S, Begovac J. The growing HIV epidemic in Central Europe: a neglected issue? J Virus Erad. 2016;2(3):156–61.
Degenhardt L, Peacock A, Colledge S, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–207. https://doi.org/10.1016/s2214-109x(17)30375-3.
Ministry of Healthcare. Approving the state strategy to combat the spread of HIV in Russia through 2020 and beyond. Ministry of Healthcare, Russia; 2016.
Treatment Preparedness Coalition, ARV procurement in 2014: history of decentralization. Results of monitoring of ARV procurement and provision in the Russian Federation. St. Petersburg; 2015.
UNAIDS. The gap report. 2014.
Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Hagan H. Are females who inject drugs at higher risk for HIV infection than males who inject drugs: an international systematic review of high seroprevalence areas. Drug Alcohol Depend. 2012;124(1–2):95–107.
Griesbeck M, Scully E, Altfeld M. Sex and gender differences in HIV-1 infection. Clin Sci (Lond Engl 1979). 2016;130(16):1435–51.
El-Bassel N, Strathdee SA. Women who use or inject drugs: an action agenda for women-specific, multilevel, and combination HIV prevention and research. J Acquir Immune Defic Syndr. 2015;1(69 Suppl 2):S182–90. https://doi.org/10.1097/qai.0000000000000628.
Beyrer C, Wirtz AL, O’Hara G, Léon N, Kazatchkine M. The expanding epidemic of HIV-1 in the Russian Federation. PLoS Med. 2017;14(11):e1002462. https://doi.org/10.1371/journal.pmed.1002462.
Girchenko P, King EJ. Correlates of double risk of HIV acquisition and transmission among women who inject drugs in St. Petersburg, Russia. AIDS Behav. 2017;21(4):1054–8.
Calabrese SK, Burke SE, Dovidio JF, Levina OS, Uuskula A, Niccolai LM, et al. Internalized HIV and drug stigmas: interacting forces threatening health status and health service utilization among people with HIV who inject drugs in St. Petersburg, Russia. AIDS Behav. 2016;20(1):85–97.
McLellan A, Lewis D, O’Brien C, Kleber H. Drug dependence, a chronic medical illness: implications for treatment, insurance and outcomes evaluation. JAMA. 2000;284:1689–95.
O’Brien CP. Addiction and dependence in DSM-V. Addiction. 2011;106:866–7.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: systematic review and meta-analysis of experimental studies. Addiction. 2012;107(1):51–9.
Shuper PA, Joharchi N, Irving H, Rehm J. Alcohol as a correlate of unprotected sexual behavior among people living with HIV/AIDS: review and meta-analysis. AIDS Behav. 2009;13(6):1021–36.
Saitz R, Freedner N, Palfai TP, Horton NJ, Samet JH. The severity of unhealthy alcohol use in hospitalized medical patients. The spectrum is narrow. J Gen Intern Med. 2006;21(4):381–5.
McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, et al. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis. 1985;173(7):412–23.
Wechsberg W. Revised risk behavior assessment, part I and part II. Research Triangle Park: Research Triangle Institute; 1998.
Navaline HA, Snider EC, Petro CJ, Tobin D, Metzger D, Alterman AI, et al. Preparations for AIDS vaccine trials. An automated version of the Risk Assessment Battery (RAB): enhancing the assessment of risk behaviors. AIDS Res Hum Retrovir. 1994;10(Suppl 2):S281–3.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59 Suppl 20:22–33; quiz 4–57.
National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol use disorders identification test (AUDIT).
Weatherby NL, Needle R, Cesari H, Booth R, McCoy CB, Watters JK, et al. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plan. 1994;17(4):347–55.
Needle R, Fisher DG, Weatherby NL, Chitwood D, Brown B, Cesari H, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychol Addict Behav. 1995;9(4):242–50.
Kazis LE, Miller DR, Clark JA, Skinner KM, Lee A, Ren XS, et al. Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the Veterans Health Study. J Ambul Care Manag. 2004;27(3):263–80.
Azim T, Bontell I, Strathdee SA. Women, drugs and HIV. Int J Drug Policy. 2015;26(Suppl 1):S16–21.
Gyarmathy VA, Li N, Tobin KE, Hoffman IF, Sokolov N, Levchenko J, et al. Unprotected sex in heterosexual partnerships of injecting drug users in St. Petersburg, Russia. AIDS Behav. 2011;15(1):58–64.
Davidson AS, Zaller N, Dukhovlinova E, Toussova O, Feller E, Heimer R, et al. Speaking the truth: an analysis of gender differences in serostatus disclosure practices among HIV-infected patients in St. Petersburg, Russia. Int J STD AIDS. 2012;23(10):685–8.
Belyakov N, Konovalova NV, Ogurtsova SV, Svetlichnaya YS, Bobreshova AS, Gezey MA, et al. Is a new wave of HIV spread in the northwest of the Russian Federation a threat or the fact? HIV Infect Immunosuppr Disord. 2016;8(1):73–82.
Montaner JS, Lima VD, Harrigan PR, Lourenco L, Yip B, Nosyk B, et al. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the “HIV Treatment as Prevention” experience in a Canadian setting. PLoS ONE. 2014;9(2):e87872.
Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet (Lond Engl). 2013;381(9883):2083–90.
Kalichman SC, et al. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2007;44:594–600.
Scheibe A, Makapela D, Brown B, dos Santos M, Hariga F, Virk H, et al. HIV prevalence and risk among people who inject drugs in five South African cities. Int J Drug Policy. 2016;30:107–15.
Centers for Disease Control and Prevention. HIV infection and risk, prevention, and testing behaviors among injecting drug users—national HIV behavioral surveillance system, 20 U.S. cities, 2009. 4 July 2014, Report No. 2014.
Gore-Felton C, Somlai AM, Benotsch EG, Kelly JA, Ostrovski D, Kozlov A. The influence of gender on factors associated with HIV transmission risk among young Russian injection drug users. Am J Drug Alcohol Abuse. 2003;29(4):881–94.
Page K, Tsui J, Maher L, Choopanya K, Vanichseni S, Mock PA, et al. Biomedical HIV prevention including pre-exposure prophylaxis and opiate agonist therapy for women who inject drugs: state of research and future directions. J Acquir Immune Defic Syndr. 1999;2015(69 Suppl 2):S169–75.
Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Control Saf Promot. 2008;15(4):221–31.
Devries KM, Child JC, Bacchus LJ, Mak J, Falder G, Graham K, Watts C, Heise L. Intimate partner violence victimization and alcohol consumption in women: a systematic review and meta-analysis. Addiction. 2014;109(3):379–91. https://doi.org/10.1111/add.12393 Epub 13 Dec 2013 .
Acknowledgements
The study and its data analysis was supported by the following NIH Grant Funding: U01AA020780, U01AA021989, U01AA021989-05S1, U24AA020778, U24AA020779, and K01AA024068.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional and/or National Research Committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Wagman, J.A., Samet, J.H., Cheng, D.M. et al. Female Gender and HIV Transmission Risk Behaviors Among People Living with HIV Who Have Ever Used Injection Drugs in St. Petersburg, Russia. AIDS Behav 22, 2830–2839 (2018). https://doi.org/10.1007/s10461-018-2149-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2149-7