Abstract
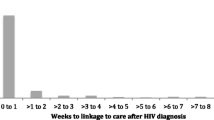
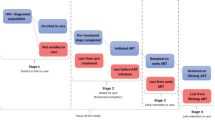
Quantifying HIV service provision along the HIV care continuum is increasingly important for monitoring and evaluating HIV interventions. We examined factors associated with linkage and retention in care longitudinally among MSM (n = 1974, 4933 person-years) diagnosed and living in Guangzhou, China, in 2008–2014. We measured longitudinal change of retention in care (≥2 CD4 tests per year) from linkage and antiretroviral therapy initiation (ART). We examined factors associated with linkage using logistic regression and with retention using generalized estimating equations. The rate of linkage to care was 89% in 2014. ART retention rate dropped from 71% (year 1) to 46% (year 2), suggesting that first-year retention measures likely overestimate retention over longer periods. Lower CD4 levels and older age predicted retention in ART care. These data can inform interventions to improve retention about some subgroups.


Similar content being viewed by others
References
Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800.
Tang W, Han L, Best J, et al. Crowdsourcing HIV test promotion videos: a noninferiority randomized controlled trial in China. Clin Infect Dis. 2016;62(11):1436–42.
Cheng W, Cai Y, Tang W, et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016;94(3):222–7.
Marks G, Crepaz N, Senterfitt JW, Janssen RS. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J Acquir Immune Def Synd. 2005;39:446–53.
Maulsby C, Jain KM, Weir BW, et al. The cost and threshold analysis of retention in care (RiC): a Multi-Site National HIV Care Program. AIDS Behav. 2017;21(3):643–9.
Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–96.
Koenig SP, Bernard D, Devieux JG, et al. Trends in CD4 count testing, retention in pre-ART care, and ART initiation rates over the first decade of expansion of HIV services in Haiti. PLoS ONE. 2016;11(2):e0146903.
Cornell M, Grimsrud A, Fairall L, et al. Temporal changes in programme outcomes among adult patients initiating antiretroviral therapy across South Africa, 2002–2007. AIDS. 2010;24(14):2263–70.
Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27(16):2559–66.
Zhu H, Napravnik S, Eron J, et al. Attrition among human immunodeficiency virus (HIV)- infected patients initiating antiretroviral therapy in China, 2003–2010. PLoS ONE. 2012;7(6):e39414.
McNairy ML, Lamb MR, Abrams EJ, et al. Use of a Comprehensive HIV care cascade for evaluating HIV Program Performance: findings from 4 Sub-Saharan African countries. J Acquir Immune Defic Syndr. 2015;70(2):e44–51.
Clouse K, Pettifor AE, Maskew M, et al. Patient retention from HIV diagnosis through one year on antiretroviral therapy at a primary health care clinic in Johannesburg, South Africa. J Acquir Immune Defic Syndr. 2013;62(2):e39–46.
Haas AD, Tenthani L, Msukwa MT, et al. Retention in care during the first 3 years of antiretroviral therapy for women in Malawi’s option B+ programme: an observational cohort study. Lancet HIV. 2016;3(4):e175–82.
McFall AM, Mehta SH, Srikrishnan AK, et al. Getting to 90: linkage to HIV care among men who have sex with men and people who inject drugs in India. AIDS Care. 2016;28(10):1230–9.
Parchure R, Kulkarni V, Kulkarni S, Gangakhedkar R. Pattern of linkage and retention in HIV care continuum among patients attending referral HIV care clinic in private sector in India. AIDS Care. 2015;27(6):716–22.
National Health and Family Planning Commission of the People’s Republic of China. 2015 China AIDS Response Progress Report. Beijing, China May 2015 2015.
Wu Z, Sullivan SG, Wang Y, Rotheram-Borus MJ, Detels R. Evolution of China’s response to HIV/AIDS. Lancet. 2007;369(9562):679–90.
Zhang F, Dou Z, Ma Y, et al. Five-year outcomes of the China National Free Antiretroviral Treatment Program. Ann Intern Med. 2009;151(4):241–51.
National Center for AIDS/STD Control and Prevention China CDC (2016) [National Health and Family Planning Commission of the People’s Republic of China: antiretroviral therapy provision is not mandatory]. http://www.chinaaids.cn/zlgh/hdjz6/201606/t20160622_131594.htm.
Zhang D, Li C, Meng S, Qi J, Fu X, Sun J. Attrition of MSM with HIV/AIDS along the continuum of care from screening to CD4 testing in China. AIDS Care. 2014;26(9):1118–21.
Chow EP, Muessig KE, Yuan L, et al. Risk behaviours among female sex workers in China: a systematic review and data synthesis. PLoS ONE. 2015;10(3):e0120595.
Yang GL, Yan J, Liu Y, Huang ZL, Long S. Retention in care and factors affecting it among people living with HIV/AIDS in Changsha City, China. Asia Pac J Public Health. 2015;27(2 Suppl):86s–92s.
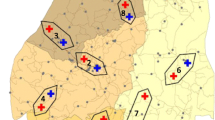
Zhong F, Liang B, Xu H, et al. Increasing HIV and decreasing syphilis prevalence in a context of persistently high unprotected anal intercourse, six consecutive annual surveys among men who have sex with men in Guangzhou, China, 2008–2013. PLoS ONE. 2014;9(7):e103136.
Zhang L, Chow EP, Zhang J, Jing J, Wilson DP. Describing the Chinese HIV surveillance system and the influences of political structures and social stigma. Open AIDS J. 2012;6:163–8.
Christopoulos KA, Das M, Colfax GN. Linkage and retention in HIV care among men who have sex with men in the United States. Clin Infect Dis. 2011;52(Suppl 2):S214–22.
Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157(4):364–75.
Yan H, Zhang R, Wei C, et al. A peer-led, community-based rapid HIV testing intervention among untested men who have sex with men in China: an operational model for expansion of HIV testing and linkage to care. Sex Transm Infect. 2014;90(5):388–93.
Eberhart MG, Yehia BR, Hillier A, et al. Behind the cascade: analyzing spatial patterns along the HIV care continuum. J Acquir Immune Defic Syndr. 2013;64(Suppl 1):S42–51.
Nosyk B, Montaner JS, Colley G, et al. The cascade of HIV care in British Columbia, Canada, 1996–2011: a population-based retrospective cohort study. Lancet Infect Dis. 2014;14(1):40–9.
Belza MJ, Hoyos J, Fernandez-Balbuena S, et al. Assessment of an outreach street-based HIV rapid testing programme as a strategy to promote early diagnosis: a comparison with two surveillance systems in Spain, 2008–2011. Euro Surveill. 2015;20(14):23–33.
Suthar AB, Ford N, Bachanas PJ, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS Med. 2013;10(8):e1001496.
Robertson M, Wei SC, Beer L, et al. Delayed entry into HIV medical care in a nationally representative sample of HIV-infected adults receiving medical care in the USA. AIDS Care. 2016;28(3):325–33.
Zhang D, Lu H, Zhuang M, et al. Enhancing HIV testing and treatment among men who have sex with men in China: a pilot model with two-rapid tests, single blood draw session, and intensified case management in six cities in 2013. PLoS ONE. 2016;11(12):e0166812.
Tucker JD, Muessig KE, Cui R, et al. Organizational characteristics of HIV/syphilis testing services for men who have sex with men in South China: a social entrepreneurship analysis and implications for creating sustainable service models. BMC Infect Dis. 2014;14:601.
Vinikoor MJ, Joseph J, Mwale J, et al. Age at antiretroviral therapy initiation predicts immune recovery, death, and loss to follow-up among HIV-infected adults in urban Zambia. AIDS Res Hum Retroviruses. 2014;30(10):949–55.
Lall P, Lim SH, Khairuddin N, Kamarulzaman A. Review: an urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc. 2015;18(2 Suppl 1):19393.
Wong NS, Reidpath DD, Wong KH, Lee SS. A multilevel approach to assessing temporal change of CD4 recovery following HAART initiation in a cohort of Chinese HIV positive patients. J Infect. 2015;70(6):676–8.
Naftalin CM, Wong NS, Chan DP, Wong KH, Reidpath DD, Lee SS. Three different patterns of CD4 recovery in a cohort of Chinese HIV patients following antiretroviral therapy—a five-year observational study. Int J STD AIDS. 2015;2015(26):803–9.
Wu Z, Zhao Y, Ge X, et al. Simplified HIV testing and treatment in China: analysis of mortality rates before and after a structural intervention. PLoS Med. 2015;12(9):e1001874.
State Council Office. [China’s 13th Five-year Action Plan for Reducing and Preventing the Spread of HIV/AIDS (2016–2020)]. Beijing. 2017.
Zhou W, Zhao M, Wang X, et al. Treatment adherence and health outcomes in MSM with HIV/AIDS: patients enrolled in “one-stop” and standard care clinics in Wuhan China. PLoS ONE. 2014;9(12):e113736.
Ning C, Smith KM, McCann CD, et al. Outcome of sentinel hospital-based and CDC-based ART service delivery: a prospective open cohort of people living with HIV in China. Sci Rep. 2017;7:42637.
Acknowledgements
The authors thank all staff of Guangzhou Center for Disease Control and Prevention for their assistance in the maintenance of the database used in this study. Li Ka Shing Institute of Health Sciences and Stanley Ho Centre for Emerging Infectious Diseases of The Chinese University of Hong Kong are acknowledged for providing technical support in conducting the research.
Funding
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This research was funded by The Project for Key Medicine Discipline Construction of Guangzhou Municipality (Grant Number 2017-2019-07), Bill & Melinda Gates Foundation to the MeSH Consortium (BMGF-OPP1120138), NIH Fogarty International Center Grant, the South China-UNC STD Research Training Center Grant (FIC1D43TW009532-01), SESH R01 Grant (NIAID 1R01AI114310), and Doris Duke International Clinical Research Grant.
Disclaimer
The opinions and assertions contained herein are private views of the authors and do not necessarily reflect their affiliating institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
IRB approval was obtained from the Guangzhou CDC, and the Guangdong Provincial Center for Skin Diseases and STI Control, China, and from University of North Carolina at Chapel Hill.
Rights and permissions
About this article
Cite this article
Wong, N.S., Mao, J., Cheng, W. et al. HIV Linkage to Care and Retention in Care Rate Among MSM in Guangzhou, China. AIDS Behav 22, 701–710 (2018). https://doi.org/10.1007/s10461-017-1893-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1893-4