Abstract
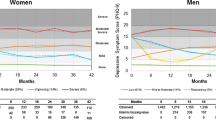
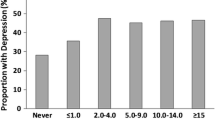
Cocaine use is prevalent among HIV-infected individuals. While cross-sectional studies suggest that cocaine users may be at increased risk for depression, long-term effects of cocaine on depressive symptoms remain unclear. This is a longitudinal study of 341 HIV-infected and uninfected men (135 cocaine users and 206 controls) ages 30–60 enrolled in the Multicenter AIDS Cohort Study during 1996–2009. The median baseline age was 41; 73% were African-American. In mixed-effects models over a median of 4.8 years of observation, cocaine use was associated with higher depressive symptoms independent of age, education level, and smoking (n = 288; p = 0.02); HIV infection modified this association (p = 0.03). Latent class mixed models were used to empirically identify distinct depressive trajectories (n = 160). In adjusted models, cocaine use was associated with threefold increased odds of membership in the class with persistent high depressive symptoms (95% confidence interval (CI) 1.38–6.69) and eightfold increased odds (95% CI (2.73–25.83) when tested among HIV-infected subjects only. Cocaine use is a risk factor for chronic depressive symptoms, particularly among HIV-infected men, highlighting the importance of integrating mental health and substance use treatments to address barriers to well-being and successful HIV-care.

Similar content being viewed by others
References
Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus–infected adults in the United States. Arch Gen Psychiatry. 2001;58(8):721–8.
Baum MK, Rafie C, Lai S, Sales S, Page B, Campa A. Crack-cocaine use accelerates HIV disease progression in a cohort of HIV-positive drug users. J Acquir Immune Defic Syndr. 2009;50(1):93–9.
Daskalopoulou M, Rodger A, Phillips AN, Sherr L, Speakman A, Collins S, et al. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: results from the cross-sectional ASTRA study. Lancet HIV. 2014;1(1):e22–31.
Mimiaga MJ, Reisner SL, Grasso C, Crane HM, Sa Safren, Kitahata MM, et al. Substance use among HIV-infected patients engaged in primary care in the United States: findings from the Centers for AIDS Research Network of Integrated Clinical Systems cohort. Am J Public Health. 2013;103:1457–67.
Cook JA, Burke-Miller JK, Cohen MH, Cook RL, Vlahov D, Wilson TE, et al. Crack cocaine, disease progression, and mortality in a multi-center cohort of HIV-1 positive women. AIDS. 2008;22(11):1355–63.
Duncan R, Shapshak P, Page JB, Chiappelli F, McCoy CB, Messiah SE. Crack cocaine: effect modifier of RNA viral load and CD4 count in HIV infected African American women. Front Biosci. 2007;12:1488–95.
Shoptaw S, Stall R, Bordon J, Kao U, Cox C, Li X, et al. Cumulative exposure to stimulants and immune function outcomes among HIV-positive and HIV-negative men in the Multicenter AIDS Cohort Study. Int J STD AIDS. 2012;23(8):576–80.
Cofrancesco J Jr, Scherzer R, Tien PC, Gibert CL, Southwell H, Sidney S, et al. Illicit drug use and HIV treatment outcomes in a US cohort. AIDS. 2008;22(3):357.
Palamar JJ, Davies S, Ompad DC, Cleland CM, Weitzman M. Powder cocaine and crack use in the United States: an examination of risk for arrest and socioeconomic disparities in use. Drug Alcohol Depend. 2015;149:108–16.
Drug Enforcement Administration. National drug threat assessment summary 2014. US Department of Justice. 2013;401–3.
Meade CS, Conn NA, Skalski LM, Safren SA. Neurocognitive impairment and medication adherence in HIV patients with and without cocaine dependence. J Behav Med. 2011;34(2):128–38.
Rosenberg ES, Grey JA, Sanchez TH, Sullivan PS. Rates of prevalent HIV infection, prevalent diagnoses, and new diagnoses among men who have sex with men in US States, metropolitan statistical areas, and counties, 2012–2013. JMIR Public Health Surveill. 2016;2(1):e22.
Centre for Disease Control and Prevention. Diagnoses of HIV infection among adolescents and young adults in the United States and 6 dependent areas, 2010–2014. HIV Surveill Suppl Rep. 2016;2016(21):3.
Pathela P, Jamison K, Braunstein SL, Schillinger JA, Varma JK, Blank S. Incidence and Predictors of HIV Infection Among Men Who Have Sex with Men Attending Public Sexually Transmitted Disease Clinics, New York City, 2007–2012. AIDS Behav. 2016;21:1–8.
Hatsukami DK, Fischman MW. Crack cocaine and cocaine hydrochloride: are the differences myth or reality? JAMA. 1996;276(19):1580–8.
Koblin BA, Chesney MA, Husnik MJ, Bozeman S, Celum CL, Buchbinder S, et al. High-risk behaviors among men who have sex with men in 6 US cities: baseline data from the EXPLORE Study. Am J Public Health. 2003;93(6):926–32.
Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, et al. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159(10):1002–12.
Colfax G, Coates TJ, Husnik MJ, Huang Y, Buchbinder S, Koblin B, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of san francisco men who have sex with men. J Urban Health. 2005;82(1 Suppl 1):62–70.
Hayashi K, Wood E, Kerr T, Dong H, Nguyen P, Puskas CM, et al. Factors associated with optimal pharmacy refill adherence for antiretroviral medications and plasma HIV RNA non-detectability among HIV-positive crack cocaine users: a prospective cohort study. BMC Infect Dis. 2016;16(1):455.
Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, et al. Impact of Active Drug Use on Antiretroviral Therapy Adherence and Viral Suppression in HIV-infected Drug Users. J Gen Intern Med. 2002;17(5):377–81.
Hinkin CH, Barclay TR, Castellon SA, Levine AJ, Durvasula RS, Marion SD, et al. Drug use and medication adherence among HIV-1 infected individuals. AIDS Behav. 2007;11(2):185–94.
Woicik PA, Moeller SJ, Alia-Klein N, Maloney T, Lukasik TM, Yeliosof O, et al. The neuropsychology of cocaine addiction: recent cocaine use masks impairment. Neuropsychopharmacology. 2009;34(5):1112–22.
Potvin S, Stavro K, Rizkallah E, Pelletier J. Cocaine and cognition: a systematic quantitative review. J Addict Med. 2014;8(5):368–76.
Spronk DB, van Wel JH, Ramaekers JG, Verkes RJ. Characterizing the cognitive effects of cocaine: a comprehensive review. Neurosci Biobehav Rev. 2013;37(8):1838–59.
Waldrop-Valverde D, Ownby RL, Kumar M. Influence of depression and HIV serostatus on the neuropsychological performance of injecting drug users. Psychiatry Clin Neurosci. 2005;59(4):372–8.
Kjome KL, Lane SD, Schmitz JM, Green C, Ma L, Prasla I, et al. Relationship between impulsivity and decision making in cocaine dependence. Psychiatry Res. 2010;178(2):299–304.
Hammond ER, Lai S, Wright CM, Treisman GJ. Cocaine Use May be Associated with Increased Depression in Persons Infected with HIV. AIDS Behav. 2016;20(2):345–52.
Meade CS, Towe SL, Skalski LM, Robertson KR. Independent effects of HIV infection and cocaine dependence on neurocognitive impairment in a community sample living in the southern United States. Drug Alcohol Depend. 2015;149:128–35.
Heaton RK, Franklin, Ellis RJ, McCutchan JA, Letendre SL, Leblanc S, et al. HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol. 2011;17(1):3–16.
Millar BM, Starks TJ, Gurung S, Parsons JT. The impact of comorbidities, depression, and substance use problems on quality of life among older adults living with HIV. AIDS Behav. 2016;21:1–7.
Meade CS, Sikkema KJ. HIV risk behavior among adults with severe mental illness: a systematic review. Clin Psychol Rev. 2005;25(4):433–57.
Reisner SL, Mimiaga MJ, Skeer M, Bright D, Cranston K, Isenberg D, et al. Clinically significant depressive symptoms as a risk factor for HIV infection among black MSM in Massachusetts. AIDS Behav. 2009;13(4):798–810.
Gilmer WS, Trivedi M, Rush A, Wisniewski S, Luther J, Howland R, et al. Factors associated with chronic depressive episodes: a preliminary report from the STAR-D project. Acta Psychiatr Scand. 2005;112(6):425–33.
Tsao JC, Stein JA, Ostrow D, Stall RD, Plankey MW. The mediating role of pain in substance use and depressive symptoms among Multicenter AIDS Cohort Study (MACS) participants. Pain. 2011;152(12):2757–64.
Bolla KI, Funderburk FR, Cadet JL. Differential effects of cocaine and cocaine alcohol on neurocognitive performance. Neurology. 2000;54(12):2285–92.
Colzato LS, van den Wildenberg WPM, Hommel B. Reduced attentional scope in cocaine polydrug users. PLoS ONE. 2009;4:e6043.
Farrin L, Hull L, Unwin C, Wykes T, David A. Effects of depressed mood on objective and subjective measures of attention. J Neuropsychiatry Clin Neurosci. 2003;15:98–104.
You ZB, Wang B, Zitzman D, Azari S, Wise RA. A role for conditioned ventral tegmental glutamate release in cocaine seeking. J Neurosci. 2007;27(39):10546–55.
Gu H, Salmeron BJ, Ross TJ, Geng X, Zhan W, Stein EA, et al. Mesocorticolimbic circuits are impaired in chronic cocaine users as demonstrated by resting-state functional connectivity. NeuroImage. 2010;53(2):593–601.
Durvasula RS, Myers HF, Satz P, Miller EN, Morgenstern H, Richardson MA, et al. HIV-1, cocaine, and neuropsychological performance in African American men. J Int Neuropsychol Soc. 2000;6(3):322–35.
Meyer VJ, Rubin LH, Martin E, Weber KM, Cohen MH, Golub ET, et al. HIV and recent illicit drug use interact to affect verbal memory in women. J Acquir Immune Defic Syndr. 2013;63(1):67–76.
Weber E, Morgan EE, Iudicello JE, Blackstone K, Grant I, Ellis RJ, et al. Substance use is a risk factor for neurocognitive deficits and neuropsychiatric distress in acute and early HIV infection. J Neurovirol. 2013;19(1):65–74.
Richert L, Brault M, Mercie P, Dauchy FA, Bruyand M, Greib C, et al. Decline in locomotor functions over time in HIV-infected patients. Aids. 2014;28(10):1441–9.
Gold JA, Grill M, Peterson J, Pilcher C, Lee E, Hecht FM, et al. Longitudinal characterization of depression and mood states beginning in primary HIV infection. AIDS Behav. 2014;18(6):1124–32.
Arseniou S, Arvaniti A, Samakouri M. HIV infection and depression. Psychiatry Clin Neurosci. 2014;68(2):96–109.
Anagnostopoulos A, Ledergerber B, Jaccard R, Shaw SA, Stoeckle M, Bernasconi E, et al. Frequency of and risk factors for depression among participants in the Swiss HIV Cohort Study (SHCS). PLoS ONE. 2015;10(10):e0140943.
Becker JT, Kingsley LA, Molsberry S, Reynolds S, Aronow A, Levine AJ, et al. Cohort Profile: Recruitment cohorts in the neuropsychological substudy of the Multicenter AIDS Cohort Study. Int J Epidemiol. 2014;24:1–11.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401.
Miller EN. California computerized assessment package. Encyclopedia of Clinical Neuropsychology. New York: Springer; 2011. p. 473–5.
Kupprat SA, Halkitis PN, Pérez-Figueroa R, Solomon TM, Ashman T, Kingdon MJ, et al. Age-and education-matched comparison of aging HIV + men who have sex with men to general population on common neuropsychological assessments. J Health Psychol. 2015;20(9):1175–85.
Boyle PA, Wilson RS, Yu L, Barr AM, Honer WG, Schneider JA, 478, et al. Much of late life cognitive decline is not due to common neurodegenerative pathologies. Ann Neurol. 2013;74(3):478–89.
Wadsworth LP, Lorius N, Donovan NJ, Locascio JJ, Rentz DM, Johnson KA, et al. Neuropsychiatric symptoms and global functional impairment along the Alzheimer’s continuum. Dement Geriatr Cogn Disord. 2012;34(2):96–111.
Philipps V, Amieva H, Andrieu S, Dufouil C, Berr C, Dartigues JF, et al. Normalized mini-mental state examination for assessing cognitive change in population-based brain aging studies. Neuroepidemiology. 2014;43(1):15–25.
Fallu JS, Briere FN, Janosz M. Latent classes of substance use in adolescent cannabis users: predictors and subsequent substance-related harm. Front Psychiatry. 2014;5(9):1–10.
Ostbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981–2006). Int J Epidemiol. 2011;40(1):240–50.
Marioni RE, Proust-Lima C, Amieva H, Brayne C, Matthews FE, Dartigues JF, et al. Cognitive lifestyle jointly predicts longitudinal cognitive decline and mortality risk. Eur J Epidemiol. 2014;29(3):211–9.
Andruff H, Carraro N, Thompson A, Gaudreau P. Latent Class Growth Modelling: a Tutorial. Tutor Quant Methods Psychol. 2009;5(1):11–24.
Vistisen D, Witte DR, Tabák AG, Herder C, Brunner EJ, Kivimäki M, et al. Patterns of obesity development before the diagnosis of type 2 diabetes: the Whitehall II cohort study. PLoS Med. 2014;11(2):e1001602.
Mimiaga MJ, Reisner SL, Fontaine YM, Bland SE, Driscoll MA, Isenberg D. Walking the line: stimulant use during sex and HIV risk behavior among Black urban MSM. Drug Alcohol Depend. 2010;110(1–2):30–7.
Friedman, Stall R, Silvestre AJ, Wei C, Shoptaw S, Herrick A, et al. Effects of syndemics on HIV viral load and medication adherence in the multicentre AIDS Cohort Study. AIDS. 2015;29(9):1087–96.
Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18(1):10–25.
Radcliffe J, Doty N, Hawkins LA, Gaskins CS, Beidas R, Rudy BJ. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS Patient Care STDs. 2010;24(8):493–9.
Oh DL, Sarafian F, Silvestre A, Brown T, Jacobson L, Badri S, et al. Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among White, Hispanic, and Black men in the MACS Cohort. J Acquir Immune Defic Syndr. 2009;52(2):290–3.
Fox HC, Jackson ED, Sinha R. Elevated cortisol and learning and memory deficits in cocaine dependent individuals: relationship to relapse outcomes. Psychoneuroendocrinology. 2009;34(8):1198–207.
Wisniewski AB, Brown TT, John M, Cofranceso J, Jr., Golub ET, Ricketts EP, et al. Cortisol levels and depression in men and women using heroin and cocaine. Psychoneuroendocrinology. 2005;31(2):250–5.
Dyer TP, Shoptaw S, Guadamuz TE, Plankey M, Kao U, Ostrow D, et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. J Urban Health. 2012;89(4):697–708.
Levine AJ, Reynolds S, Cox C, Miller EN, et al. The longitudinal and interactive effects of HIV status, stimulant use, and host genotype upon neurocognitive functioning. J Neurovirol. 2014;20(3):243–57.
Molsberry SA, Lecci F, Kingsley L, Junker B, Reynolds S, Goodkin K, et al. Mixed membership trajectory models of cognitive impairment in the multicenter AIDS cohort study. Aids. 2015;5:29.
Grant I, Olshen RA, Atkinson JH, Heaton RK, Nelson J, McCutchan JA, et al. Depressed mood does not explain neuropsychological deficits in HIV-infected persons. Neuropsychology. 1993;7(1):53.
Castellon SA, Hardy DJ, Hinkin CH, Satz P, Stenquist PK, van Gorp WG, et al. Components of depression in HIV-1 infection: their differential relationship to neurocognitive performance. J Clin Exp Neuropsychol. 2006;28(3):420–37.
Cysique LA, Deutsch R, Atkinson JH, Young C, Marcotte TD, Dawson L, et al. Incident major depression does not affect neuropsychological functioning in HIV-infected men. J Int Neuropsychol Soc. 2007;13(01):1–11.
Milanini B, Catella S, Perkovich B, Esmaeili-Firidouni P, Wendelken L, Paul R, et al. Psychiatric symptom burden in older people living with HIV with and without cognitive impairment: the UCSF HIV over 60 cohort study. AIDS Care. 2017. doi:10.1080/09540121.2017.1281877.
Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS ONE. 2011;6(8):e17502.
Acknowledgements
The authors are grateful to Drs. Steven Wolinsky, Cecile Proust-Lima, and Dorene Rentz for discussion of primary data and the analysis, and Ms. Elizabeth Carpelan for assistance with manuscript preparation. The data for this manuscript was obtained by the Multicenter AIDS Cohort Study (MACS) with centers at: Baltimore (U01-AI35042): The Johns Hopkins University Bloomberg School of Public Health: Joseph B. Margolick (PI), Jay Bream, Todd Brown, Barbara Crain, Adrian Dobs, Richard Elion, Richard Elion, Michelle Estrella, Lisette Johnson-Hill, Sean Leng, Anne Monroe, Cynthia Munro, Michael W. Plankey, Wendy Post, Ned Sacktor, Jennifer Schrack, Chloe Thio; Chicago (U01-AI35039): Feinberg School of Medicine, Northwestern University, and Cook County Bureau of Health Services: Steven M. Wolinsky (PI), John P. Phair, Sheila Badri, Dana Gabuzda, David Ostrow, Frank J. Palella, Jr., Sudhir Penugonda, Susheel Reddy, Matthew Stephens, Linda Teplin; Los Angeles (U01-AI35040): University of California, UCLA Schools of Public Health and Medicine: Roger Detels (PI), Otoniel Martínez-Maza (Co-P I), Aaron Aronow, Peter Anton, Robert Bolan, Elizabeth Breen, Anthony Butch, Shehnaz Hussain, Beth Jamieson, Eric N. Miller, John Oishi, Harry Vinters, Dorothy Wiley, Mallory Witt, Otto Yang, Stephen Young, Zuo Feng Zhang; Pittsburgh (U01-AI35041): University of Pittsburgh, Graduate School of Public Health: Charles R. Rinaldo (PI), Lawrence A. Kingsley (Co-PI), James T. Becker, Phalguni Gupta, Kenneth Ho, Susan Koletar, Jeremy J. Martinson, John W. Mellors, Anthony J. Silvestre, Ronald D. Stall; Data Coordinating Center (UM1-AI35043): The Johns Hopkins University Bloomberg School of Public Health: Lisa P. Jacobson (PI), Gypsyamber D’Souza (Co-PI), Alison, Abraham, Keri Althoff, Jennifer Deal, Priya Duggal, Sabina Haberlen, Alvaro Muoz, Derek Ng, Janet Schollenberger, Eric C. Seaberg, Sol Su, Pamela Surkan.
Funding
This work was supported by NIH grants to D.G. (R01 DA28994, R01 DA30985, R01 DA40391, R01 MH110259). The work was also supported in part by NIH funding to the Northwestern University Clinical Research Unit of the MACS (U01-AI35039, with additional co-funding from National Institute on Drug Abuse (NIDA), and National Institute of Mental Health (NIMH)). Training and educational support for S.S.M and A.D. was provided by NIH T32-AG000222. Additional support for S.S.M included Harvard Catalyst Master’s Program in Clinical and Translational Investigation funded by the NIH Clinical and Translational Science Award Program (1UL1-TR001102), and Catalyst Biostatistical Consultation with contributions from Harvard Medical School and affiliated hospitals. The MACS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID) [U01-AI35039, U01-AI35040; U01-AI35041; U01-AI35042; and UM1-AI35043], with additional co-funding from the National Cancer Institute (NCI), National Institute on Drug Abuse (NIDA), and National Institute of Mental Health (NIMH) at the National Institutes of Health (NIH). MACS data collection is also supported by UL1-TR000424 (JHU CTSA). Website located at http://www.statepi.jhsph.edu/macs/macs.html.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All Authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mukerji, S., Haghighat, R., Misra, V. et al. Longitudinal Modeling of Depressive Trajectories Among HIV-Infected Men Using Cocaine. AIDS Behav 21, 1985–1995 (2017). https://doi.org/10.1007/s10461-017-1801-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-017-1801-y