Abstract
We examined the relationship between residential eviction and exhibiting detectable plasma HIV-1 RNA viral load (VL) among a prospective cohort of antiretroviral therapy (ART)-exposed HIV-seropositive people who use illicit drugs (PWUD) in Vancouver, Canada. We used multivariable generalized estimating equations to estimate the effect of residential eviction on detectable VL and examine ART adherence as a mediating variable. Between June 2007 and May 2014, 705 ART-exposed participants were included in the study, among whom 500 (70.9 %) experienced at least one period of detectable VL. In a time-updated multivariable model, eviction independently increased the odds of detectable VL among those who were homeless [adjusted odds ratio (AOR) = 2.25; 95 % confidence interval (CI) 1.18–4.29] as well as not homeless (AOR = 1.76; 95 % CI 1.17–2.63) post eviction. The results of mediation analyses suggest that this association was mediated by incomplete ART adherence. These findings suggest the need for further development and evaluation of interventions to prevent evictions and promote ART adherence among PWUD facing eviction.
Similar content being viewed by others
Introduction
Over the past two decades, significant advances in the development and distribution of combination antiretroviral therapy (ART) have contributed to substantial reductions in HIV-related morbidity and mortality among diverse HIV-seropositive populations worldwide [1]. High levels of adherence to ART have been shown to suppress plasma HIV-1 RNA viral load (VL) to undetectable levels, thereby conserving immune function, hindering HIV disease progression and extending survival [2]. In addition, it is now accepted that ART-attributable VL suppression is extremely effective at preventing HIV transmission [3]. Accordingly, HIV treatment as prevention (TasP) currently constitutes a key strategy in the global response to HIV/AIDS. Endorsed by the World Health Organization and the Joint United Nations Programme on HIV/AIDS (UNAIDS), TasP and its related UN 90-90-90 target are being implemented in many countries worldwide [4].
Despite the availability of effective treatment, HIV-seropositive people who use illicit drugs (PWUD) continue to suffer from high rates of suboptimal virologic outcomes, including viral rebound [5, 6] and failure to achieve viral suppression [7–10]. Although behavioral factors, such as ongoing illicit drug use, can complicate the medical management of HIV [11], in recent years, there has been growing research interest in contextual determinants of HIV-related vulnerabilities among PWUD [12–14]. One conceptual framework to guide the investigation of such determinants is the risk environment framework [14, 15]. First used to describe how social, physical, political and economic factors interact at macro- and micro-environmental levels to determine risk of HIV acquisition [14], the risk environment framework has recently been extended to identify social- and structural-level factors promoting HIV disease progression among PWUD [13]. These factors include incarceration [16], lack of legal income [17] and limited social support [18], which contribute to suboptimal ART adherence, premature discontinuation of treatment, and poor virologic outcomes among HIV-seropositive PWUD. Additionally, housing status has been identified as a key element of the risk environment that impacts HIV treatment outcomes [13, 19]. For instance, homelessness and unstable housing have been associated with lower levels of ART adherence [20, 21], contributing to lower rates of VL suppression [22] among PWUD. Homelessness has also been linked to other adverse health outcomes among people living with HIV, including lower self-rated mental and physical health and higher rates of emergency department utilization and death [23, 24].
While there is a wealth of research focused on the relationship between housing status and HIV treatment outcomes among vulnerable populations [13], we know of no studies that have investigated the unique impact of residential eviction (i.e., removal of a tenant from leased residential premises by legal procedure) on HIV treatment outcomes among PWUD. This is a notable research gap given previous research suggesting that dynamics within the broader risk environment, including gentrification in inner-city neighbourhoods [25] and crime-free social housing models [26, 27], render PWUD disproportionately vulnerable to evictions and make rehousing a challenge [28, 29]. Further, housing displacement has been shown to impede healthcare access and adherence among drug-using and other marginalized populations [30, 31]. The present study was therefore undertaken to examine the longitudinal effect of residential eviction on detectable VL among a community-recruited cohort of ART-exposed HIV-seropositive PWUD in a setting of universal access to healthcare and free HIV treatment. We hypothesized that ART adherence would mediate the effect of residential eviction on detectable VL.
Methods
Study Design
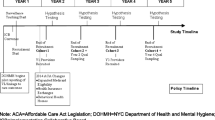
Data were collected using the AIDS Care Cohort to Evaluate Access to Survival Services (ACCESS), an open prospective cohort study of HIV-seropositive PWUD in Vancouver, Canada. The specific methods employed have been described in detail elsewhere [32]. In brief, beginning in 1996, participants were recruited through self-referral and street-based outreach from Vancouver’s Downtown Eastside neighborhood (DTES), a postindustrial area with a large open drug market and high levels of illicit drug use, poverty, and homelessness. ACCESS eligibility criteria include: aged 18 years or older, HIV-infected, having used illicit drugs other than cannabis in the previous month, and having provided written informed consent.
At baseline and semi-annually, participants complete an interviewer-administered questionnaire soliciting demographic data, information on drug use patterns, as well as other characteristics and exposures. At each of these visits, participants also undergo an examination by a study nurse and provide blood samples for serologic analyses. A nominal financial stipend ($30 CDN) is offered to participants at each study visit. Information collected at each study interview is augmented by comprehensive information on HIV care and treatment outcomes from the local centralized HIV/AIDS registry. Specifically, through a confidential linkage, a complete clinical profile of all CD4 T cell counts, HIV-1 RNA VL observations, and exposure to specific antiretroviral agents for each participant are obtained. In British Columbia, all provision of ART is centralized through a province-wide ART dispensation program, where ART and related care are provided free of charge. The ACCESS study has been approved by the University of British Columbia/Providence Healthcare Research Ethics Board.
Study Participants
We included all individuals who had received at least one day of ART at the time of the baseline interview. Individuals who were ART-naïve at baseline but who initiated treatment during follow-up were included from the next follow-up interview forward after initiating ART. As well, to be included in these analyses, at least one observation of both CD4 cell count and VL had to be completed within ±180 days of the day the participant entered the study so as to be able to adjust for disease status at baseline.
Variable Selection
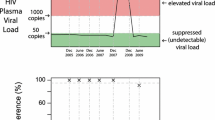
The primary outcome of interest was detectable VL in the previous six months, defined as exhibiting an HIV-1 RNA viral load >50 copies/mL plasma (yes vs. no). In the event that more than one VL observation was collected within a six-month follow-up, we used the median of all the observations, which was then categorized into either exhibiting an HIV-1 RNA viral load >50 copies/mL plasma or not. The primary explanatory variable of interest was reporting recent residential eviction. Given our interest in isolating the unique effect of eviction on VL, distinct from the effect of homelessness, we characterized this variable as a three-level measure (evicted in the last 6 months and homeless at the time of the study interview vs. evicted in the last 6 months and not homeless at the time of the study interview vs. no eviction in the last 6 months as the reference level). This variable was measured longitudinally at each follow-up and was included in the analysis as a time-updated measure. To estimate the effect of residential eviction on VL, we considered secondary explanatory variables that may potentially confound this relationship. These included a range of demographic, socioeconomic and behavioral variables such as age (per year older); gender (men vs. women and transgender individuals); ancestry (Caucasian vs. non-Caucasian); education (≥high school diploma vs. <high school diploma); DTES residence (yes vs. no); relationship (married or common law vs. other); employment (yes vs. no); injection drug use (yes vs. no); non-injection drug use (yes vs. no); binge alcohol use (yes vs. no); and prohibited income generation (yes vs. no). Employment was defined as having salaried or temporary work in the licit labor market at any time during the previous 6 months. Binge alcohol use was defined as any period of elevated alcohol use in the previous 6 months. Prohibited income generation was defined as reporting income from drug dealing or sex work in the previous 6 months. Additionally, we included the following clinical variables: CD4 cell count in the last 6 months (per 100 cells/mL); enrollment in methadone maintenance therapy (MMT) (yes vs. no); and HIV physician experience. Enrollment in MMT was considered as a potential confounder given that previous local studies of HIV-seropositive PWUD have observed positive associations between MMT and ART initiation and adherence as well as favorable HIV treatment outcomes, including VL suppression and CD4 cell count rise [33, 34]. HIV physician experience was defined as the number of patients that the participant’s prescribing physician had previously enrolled in the province-wide HIV treatment registry at the time of their initiation of treatment, dichotomized as >6 patients vs. ≤6 patients; this variable was included given that HIV physician experience has been shown to be independently associated with higher rates of VL suppression among local HIV-seropositive PWUD [35]. ART adherence was also included in our analyses and defined as the quotient of the number of days that ART was dispensed divided by the total number of days since an individual initiated ART, capped at 180 days; this proportion was dichotomized as ≥95 vs. <95 %. This validated measure using pharmacy refill data has been used extensively in previous research and has been shown to reliably predict VL suppression [36] and survival [1]. All time-varying variables are time-updated and refer to the six-month period prior to the follow-up interview unless otherwise indicated.
Statistical Analyses
As a first step, we examined the baseline characteristics of our sample, stratified by whether or not participants exhibited detectable VL in the six months prior to the baseline interview. Categorical variables were analyzed using Pearson’s X2 test and continuous variables were analyzed using the Wilcoxon Rank-Sum test. Next, we used generalized estimating equations (GEE) to estimate unadjusted odds ratios (OR) for the effect of residential eviction and all other secondary explanatory variables on detectable VL. We used GEE for the analysis of correlated data since the factors potentially associated with detectable VL during follow-up were time-dependent measures. We only included individuals with complete data at each given time point.
To estimate the independent effect of residential eviction on detectable VL, we constructed a multivariable model using an a priori variable selection process proposed by Maldonado and Greenland [37]. In this process, we employed a conservative p value cutoff ≤0.20 to determine which variables were possibly associated with detectable VL in GEE analyses described above. We then fit a full model including these explanatory variables, noting the value of the coefficient associated with residential eviction. In a manual stepwise manner, we removed the secondary explanatory variable corresponding to the smallest relative change in the effect of residential eviction on detectable VL from further consideration. We continued this iterative process until the maximum change of the value of the coefficient for residential eviction from the full model exceeded 5 %. Remaining variables were considered confounders in the multivariable model. We have previously used this approach to estimate the independent relationship between a primary explanatory variable and an outcome of interest [16, 38]. ART adherence was not considered for inclusion in the multivariable model given that this variable was hypothesized to mediate the relationship between residential eviction and detectable VL.
As a subanalysis, we conducted a mediation analysis to determine whether the relationship between residential eviction and detectable VL was mediated by incomplete ART adherence, using previously described methods [38]. We fit an additional multivariable GEE model that included ART adherence and the same set of covariates included in the primary multivariable model to determine whether the residential eviction variable maintained its significance after the ART adherence variable was added. We conducted all statistical analyses with R version 3.2.0 (The R Foundation, Vienna, Austria) and all p values are 2-sided.
Results
Between June 2007 and May 2014, 705 HIV-seropositive PWUD met the inclusion criteria for this analysis. Participants contributed 2674 person-years of follow-up over the study period. The median age at baseline was 45 years [interquartile range (IQR) = 41–52], 463 (65.7 %) were men and 381 (54.0 %) were of Caucasian ancestry. At baseline, a total of 50 (7.1 %) participants reported experiencing residential eviction in the last six months, with 17 (2.4 % total) becoming homeless post eviction and 33 (4.7 % total) not becoming homeless post eviction. A total of 149 (21.1 %) participants reported at least one residential eviction during the study period, with 110 (15.6 % total) becoming homeless post eviction and 39 (5.5 % total) not becoming homeless post eviction. At baseline, detectable VL was observed in 391 (55.5 %) participants and, in total, 500 (70.9 %) participants exhibited at least one period of detectable VL during the study period. Table 1 presents the baseline characteristics of the study sample stratified by detectable VL at baseline.
Table 2 presents the results of the crude and adjusted longitudinal estimates of the odds of detectable VL. In unadjusted analyses, residential eviction was associated with significantly higher odds of exhibiting detectable VL among those who were homeless post eviction [OR = 3.14, 95 % confidence interval (95 % CI) 1.71–5.78, p < 0.001] as well as those who were not homeless post eviction (OR = 1.79, 95 % CI 1.25–2.55, p = 0.002). Other variables that were positively associated with exhibiting detectable VL in unadjusted analyses included: DTES residence (OR = 1.44, 95 % CI 1.17–1.77, p < 0.001); injection drug use (OR = 1.86, 95 % CI 1.50–2.30, p < 0.001); non-injection drug use (OR = 1.26, 95 % CI 1.07–1.49, p = 0.007); and prohibited income generation (OR = 1.48, 95 % CI 1.00–2.20, p = 0.048). Age (OR = 0.96, 95 % CI 0.95–0.98, p < 0.001); gender (OR = 0.73, 95 % CI 0.57–0.93, p = 0.011); MMT enrollment (OR = 0.66, 95 % CI 0.53–0.82, p < 0.001); CD4 cell count (OR = 0.75, 95 % CI 0.70–0.79, p < 0.001); and ART adherence (OR = 0.20, 95 % CI 0.16–0.24, p < 0.001) were inversely associated with exhibiting detectable VL. In the multivariable confounding model, after adjusting for age, MMT enrollment, HIV physician experience, and CD4 cell count, residential eviction remained independently associated with significantly higher odds of detectable VL among those who were homeless post eviction [adjusted odds ratio (AOR) = 2.25, 95 % CI 1.18–4.29, p = 0.013] as well as those who were not homeless post eviction (AOR = 1.76, 95 % CI 1.17–2.63, p = 0.006).
In a subanalysis, when ART adherence was added to the multivariable model, the effect of recent residential eviction on detectable VL was no longer significant among those who were homeless (AOR = 1.73, 95 % CI 0.83–3.64, p = 0.146) or not homeless (AOR = 1.32, 95 % CI 0.84–2.05, p = 0.225) post eviction. These findings provide evidence that the relationship between residential eviction and detectable VL was mediated by ART adherence.
Discussion
In this prospective community-recruited cohort of more than 700 ART-exposed HIV-seropositive PWUD in Vancouver, Canada, we observed that residential evictions were relatively common, with over one-fifth of participants reporting at least one eviction over the seven-year study period. In addition, we found that over 70 % of participants experienced at least one period of detectable VL over the seven-year study period. In the adjusted model, residential eviction was independently associated with significantly higher odds of detectable VL among those who were homeless as well as not homeless post eviction, although the effect was more pronounced among those who became homeless. In a subanalysis, we found that incomplete ART adherence mediated the relationship between residential eviction and detectable VL.
To our knowledge, the present study is the first to identify an association between residential eviction and elevated risk of detectable VL among HIV-seropositive PWUD. This effect held among those who became homeless as well as not homeless post eviction, providing evidence that the disruption and dislocation associated with eviction uniquely contributes to risk for detectable VL, separate from resulting housing status. As universal access to no-cost healthcare, including free HIV medications, is provided in this setting, we believe these findings are independent of the potential confounding effects of financial barriers to care. Our findings are consistent with previous research suggesting that housing displacement may hinder access and adherence to prescriptions and healthcare. A study of 160 public housing residents (primarily PWUD) in Atlanta, Georgia found that housing relocation was associated with substantial declines in spatial access to healthcare [30]. Additionally, housing loss due to mortgage foreclosure was associated with elevated rates of healthcare and prescription nonadherence in a study comparing 250 people undergoing mortgage foreclosure to a community sample in Philadelphia, Pennsylvania [31]. Our findings also build upon established evidence of the deleterious impacts of housing instability on ART adherence and virologic outcomes among HIV-seropositive PWUD. Two previous studies of PWUD found that homelessness and lack of stable housing were associated with lower ART adherence [20, 21]. Additionally, in a study of 240 PWUD in Vancouver, homelessness was independently associated with lower rates of VL suppression following ART initiation, a relationship mediated by lower ART adherence [22]. Similar results were observed in a multisite study of 466 people who inject drugs in the United States; those with stable housing had over three times the odds of VL suppression after adjustment for a range of individual and interpersonal factors [18].
The observed association between residential eviction and elevated risk of detectable VL suggests that evictions are a critical event occurring within the risk environment of PWUD that increase vulnerability to HIV disease progression. This association is likely explained by disruptions associated with eviction that may exacerbate or generate new barriers to accessing and adhering to appropriate HIV treatment and care. For instance, evicted PWUD may lack space to safely store medication and may need to prioritize immediate concerns, such as securing new housing and storage for their belongings, over the secondary demands of ART adherence [39, 40]. Additionally, these individuals may be displaced to other neighborhoods, impeding spatial access to primary HIV care providers, pharmacies and other healthcare services [30]. Further, the stress and volatility associated with eviction and housing instability may exacerbate drug use among those recently evicted, which has been shown to undermine adherence [11, 41]. However, these interpretations cannot be confirmed by the present study and further research, ideally incorporating qualitative research methods, is necessary to elucidate the specific processes through which eviction impacts VL among PWUD.
Our findings support the further development and evaluation of strategies to address housing instability as a means for improving the health of PWUD and other marginalized HIV-seropositive groups. In particular, our finding of elevated risk of detectable VL among PWUD who were homeless as well as not homeless post eviction suggests that, in addition to literal homelessness, evictions are an important feature of housing that should receive greater policy and research attention. For instance, future research should examine the potential health benefits of imposing restrictions on renovation and demolition in low-income neighbourhoods, implementing affordable housing initiatives, and repealing rental policies, such as crime-free housing programs, that increase the potential for eviction among PWUD [26, 27]. Additionally, further research is needed to determine if strengthening legal mechanisms to protect the rights of tenants, particularly those who are marginalized by social-structural inequity, and increasing accessibility of legal advocacy to contest evictions may help to prevent housing displacement and empower tenants to enforce their housing rights [42]. Future research should also examine if providing housing assistance confers benefits for HIV-seropositive PWUD at risk of or facing eviction [22], as has been found with studies of other marginalized populations. For example, the provision of emergency housing aid, including financial assistance and housing relocation and stabilization services, to individuals facing eviction as part of the American Recovery and Reinvestment Act of 2009 resulted in a 15 % reduction in eviction rates in Milwaukee [43]. Further, a recent randomized controlled trial found that providing housing assistance to homeless and marginally-housed people living with HIV resulted in significant improvements in CD4 cell count and VL [44]. Thus, there is evidence to suggest that such interventions may delay disease progression among vulnerable HIV-seropositive groups and reduce the risk of HIV transmission [44]. However, further research is needed to formally evaluate the effectiveness of housing interventions in response to suboptimal adherence and treatment outcomes among HIV-seropositive PWUD, particularly in contexts without universal access to free care where these interventions may have attenuated benefits given additional structural barriers to treatment [22].
For HIV-seropositive PWUD who face eviction, our findings point to the need to develop and evaluate programs to help them adhere to treatment once they are displaced. For example, further research should be conducted to determine if efforts to strengthen collaborations between pharmacies and transitional housing services and to expand the reach of outreach programs to coordinate daily medication dispensation may promote ART adherence and improve HIV treatment outcomes among recently-evicted and unstably-housed seropositive PWUD.
This study has several limitations that should be noted. First, although a number of techniques are undertaken to ensure the sample is representative, including recruiting from community settings and long-term follow-up, the ACCESS cohort is a non-random sample of HIV-seropositive PWUD. Therefore, our findings may not be generalizable to HIV-seropositive drug-using populations in local or other settings. A second limitation is that the study included some data derived from self report and therefore may be subject to reporting biases, including socially desirability bias. Lastly, our analyses primarily considered individual-level characteristics as potential confounders. We were unable to adjust for structural and environmental factors associated with gentrification and redevelopment, including rent increases, building renovations, increased surveillance of public and residential spaces, and the expansion of crime free social models, as this information was either not collected or not available for the entire study period. We were also unable to adjust for important healthcare access variables, including access to mental health counselling and case management programs, as this information was not available for the entire study period. Thus, the possibility of residual confounding must be considered when interpreting the observed association between residential eviction and detectable VL. Future studies examining this association should consider the potentially confounding effects of a broader set of factors, including the aforementioned structural, environmental and healthcare access factors.
In summary, over one-fifth of HIV-seropositive PWUD in the present study experienced residential eviction over the seven-year study period and over two-thirds exhibited detectable VL. We observed that residential eviction was independently associated with increased odds of detectable VL among HIV-seropositive PWUD, regardless of whether or not evicted persons became homeless post eviction. This relationship was mediated by incomplete ART adherence. Additional research is required to further elucidate the precise mechanisms underlying the association between residential eviction and detectable VL. Nonetheless, the findings of the present study support the need for further development and evaluation of innovative interventions, including eviction prevention policy reforms and the provision of housing assistance, in effort to improve housing stability and support the health of HIV-seropositive PWUD.
References
Wood E, Hogg RS, Lima V, et al. Highly active antiretroviral therapy and survival in HIV-infected injection drug users. JAMA. 2008;300(5):550–4.
Wood E, Hogg RS, Yip B, Harrigan PR, Montaner JSG. Why are baseline HIV RNA levels 100,000 copies/mL or greater associated with mortality after the initiation of antiretroviral therapy? J Acquir Immune Defic Syndr. 2005;38(3):289–95.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. New Engl J Med. 2011;365(6):493–505.
World Health Organization. Programmatic update: antiretroviral treatment as prevention (TASP) of HIV and TB: executive summary. 2012. http://apps.who.int//iris/handle/10665/70904.
Robbins GK, Johnson KL, Chang Y, et al. Predicting virologic failure in an HIV clinic. Clin Infect Dis. 2010;50(5):779–86.
Lucas GM, Chaisson RE, Moore RD. Highly active antiretroviral therapy in a large urban clinic: risk factors for virologic failure and adverse drug reactions. Ann Intern Med. 1999;131(2):81–7.
Lucas GM, Cheever LW, Chaisson RE, Moore RD. Detrimental effects of continued illicit drug use on the treatment of HIV-1 infection. J Acquir Immune Defic Syndr. 2001;27(3):251–9.
Palepu A, Tyndall M, Yip B, O’Shaughnessy MV, Hogg RS, Montaner JSG. Impaired virologic response to highly active antiretroviral therapy associated with ongoing injection drug use. J Acquir Immune Defic Syndr. 2003;32(5):522–6.
Chander G, Himelhoch S, Fleishman JA, et al. HAART receipt and viral suppression among HIV-infected patients with co-occurring mental illness and illicit drug use. AIDS Care. 2009;21(5):655–63.
Weber R, Huber M, Rickenbach M, et al. Uptake of and virological response to antiretroviral therapy among HIV-infected former and current injecting drug users and persons in an opiate substitution treatment programme: the Swiss HIV Cohort Study. HIV Med. 2009;10(7):407–16.
Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet. 2010;376(9738):367–87.
Strathdee SA, Hallett TB, Bobrova N, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376(9737):268–84.
Milloy M-J, Marshall BDL, Kerr T, et al. Social and structural factors associated with HIV disease progression among illicit drug users: a systematic review. AIDS. 2012;26(9):1049–63.
Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61(5):1026–44.
Rhodes T. The, “risk environment”: a framework for understanding and reducing drug-related harm. Int J Drug Policy. 2002;13(2):85–94.
Milloy MJ, Kerr T, Buxton J, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis. 2011;203(9):1215–21.
Piketty C, Castiel P, Giral P, et al. Lack of legal income is strongly associated with an increased risk of AIDS and death in HIV-infected injecting drug users. AIDS Care. 1999;11(4):429–36.
Knowlton A, Arnsten J, Eldred L, et al. Individual, interpersonal, and structural correlates of effective HAART use among urban active injection drug users. J Acquir Immune Defic Syndr. 2006;41(4):486–92.
Milloy M-J, Marshall BDL, Montaner J, Wood E. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–74.
Palepu A, Milloy M-J, Kerr T, Zhang R, Wood E. Homelessness and adherence to antiretroviral therapy among a cohort of HIV-infected injection drug users. J Urban Health. 2011;88(3):545–55.
Knowlton AR, Arnsten JH, Eldred LJ, et al. Antiretroviral use among active injection-drug users: the role of patient-provider engagement and structural factors. AIDS Patient Care STDS. 2010;24(7):421–8.
Milloy M-J, Kerr T, Bangsberg DR, et al. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS. 2012;26(1):60–7.
Kidder DP, Wolitski RJ, Campsmith ML, Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–45.
Lieb S, Brooks RG, Hopkins RS, et al. Predicting death from HIV/AIDS: a case-control study from Florida public HIV/AIDS clinics. J Acquir Immune Defic Syndr. 2002;30(3):351–8.
Chum A. The impact of gentrification on residential evictions. Urban Geogr. 2015;2015:1–16.
Carey CA. No second chance: people with criminal records denied access to public housing. U Tol L Rev. 2004;2005(36):545.
Dickson-Gomez JB, Convey M, Hilario H, Corbett AM, Weeks M. Structural and personal factors related to access to housing and housing stability among urban drug users in Hartford, Connecticut. Contemp Drug Probl. 2008;35(1):115–52.
Dickson-Gomez JB, Cromley E, Convey M, Hilario H. How much choice is there in housing choice vouchers? Neighborhood risk and free market rental housing accessibility for active drug users in Hartford, Connecticut. Subst Abuse Treat Prev Policy. 2009;4(1):5.
Phinney R, Danziger S, Pollack HA, Seefeldt K. Housing instability among current and former welfare recipients. Am J Public Health. 2007;97(5):832–7.
Cooper HLF, Wodarski S, Cummings J, et al. Public housing relocations in Atlanta, Georgia, and declines in spatial access to safety net primary care. Health Place. 2012;18(6):1255–60.
Pollack CE, Lynch J. Health status of people undergoing foreclosure in the philadelphia region. Am J Public Health. 2009;99(10):1833–9.
Strathdee SA, Palepu A, Cornelisse PG, et al. Barriers to use of free antiretroviral therapy in injection drug users. JAMA. 1998;280(6):547–9.
Palepu A, Tyndall MW, Joy R, et al. Antiretroviral adherence and HIV treatment outcomes among HIV/HCV co-infected injection drug users: the role of methadone maintenance therapy. Drug Alcohol Depend. 2006;84(2):188–94.
Uhlmann S, Milloy M-J, Kerr T, et al. Methadone maintenance therapy promotes initiation of antiretroviral therapy among injection drug users. Addiction. 2010;105(5):907–13.
Sangsari S, Milloy M-J, Ibrahim A, et al. Physician experience and rates of plasma HIV-1 RNA suppression among illicit drug users: an observational study. BMC Infect Dis. 2012;12(1):22.
Wood E, Montaner JSG, Yip B, et al. Adherence and plasma HIV RNA responses to highly active antiretroviral therapy among HIV-1 infected injection drug users. CMAJ. 2003;169(7):656–61.
Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923–36.
Ti L, Milloy M-J, Shannon K, et al. Suboptimal plasma HIV-1 RNA suppression and adherence among sex workers who use illicit drugs in a Canadian setting: an observational cohort study. Sex Transm Infect. 2014;90(5):418–22.
Bangsberg D, Tulsky JP, Hecht FM, Moss AR. Protease inhibitors in the homeless. JAMA. 1997;278(1):63–5.
Scott A, Ellen J, Clum G, Leonard L. HIV and housing assistance in four U.S. cities: variations in local experience. AIDS Behav. 2007;11(6 Suppl):140–8.
Azar P, Wood E, Nguyen P, et al. Drug use patterns associated with risk of non-adherence to antiretroviral therapy among HIV-positive illicit drug users in a Canadian setting: a longitudinal analysis. BMC Infect Dis. 2015;15:193.
Thiele B. The human right to adequate housing: a tool for promoting and protecting individual and community health. Am J Public Health. 2002;92(5):712–5.
Desmond M. Eviction and the reproduction of urban poverty. Am J Sociol. 2012;118(1):88–133.
Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503.
Acknowledgments
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. We would specifically like to thank Cody Callon, Deborah Graham, Peter Vann, Steve Kain, Kristie Starr, Tricia Collingham, and Carmen Rock for their research and administrative assistance. The study was supported by the United States National Institutes of Health (R01DA021525 and R01DA033147). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine, which supports Dr. Evan Wood. Mary Clare Kennedy is supported by Mitacs through the Mitacs Accelerate Program. M-J Milloy is supported in part by the United States National Institutes of Health (R01DA021525). Ryan McNeil is supported by the Michael Smith Foundation for Health Research. Dr. Julio Montaner is supported with grants paid to his institution by the British Columbia Ministry of Health and the US National Institutes of Health (NIDA-R01DA036307). He has also received limited unrestricted funding, paid to his institution, from Abbvie, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck, and ViiV Healthcare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kennedy, M.C., Kerr, T., McNeil, R. et al. Residential Eviction and Risk of Detectable Plasma HIV-1 RNA Viral Load Among HIV-Positive People Who Use Drugs. AIDS Behav 21, 678–687 (2017). https://doi.org/10.1007/s10461-016-1315-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1315-z