Abstract
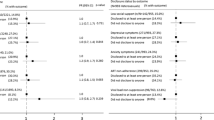
We sought to examine the prevalence and correlates of HIV-disclosure among treatment-experienced individuals in British Columbia, Canada. Study participants completed an interviewer-administered survey between July 2007 and January 2010. The primary outcome of interest was disclosing one’s HIV-positive status to all new sexual partners within the last 6 months. An exploratory logistic regression model was developed to identify variables independently associated with disclosure. Of the 657 participants included in this analysis, 73.4 % disclosed their HIV-positive status to all of their sexual partners. Factors independently associated with non-disclosure included identifying as a woman (adjusted odds ratio [AOR] 1.92; 95 % confidence interval [95 % CI] 1.13–3.27) or as a gay or bisexual man (AOR 2.45; 95 % CI 1.47–4.10). Behaviours that were independently associated with non-disclosure were having sex with a stranger (AOR 2.74; 95 % CI 1.46–5.17), not being on treatment at the time of interview (AOR 2.67; 95 % CI 1.40–5.11), and not always using a condom (AOR 1.78; 95 % CI 1.09–2.90). Future preventative strategies should focus on environmental and social factors that may inhibit vulnerable HIV-positive populations, such as women and gay or bisexual men, from safely disclosing their positive status.
Similar content being viewed by others
References
Pinkerton S, Galletly C. Reducing HIV transmission risk by increasing serostatus disclosure: a mathematical modeling analysis. AIDS Behav. 2007;11:698–705.
Chen S, et al. Unprotected anal intercourse between potentially HIV-serodiscordant men who have sex with men, San Francisco. JAIDS. 2003;33:166–70.
Golden M, et al. Importance of sex partners HIV status in HIV risk assessment among men who have sex with men. JAIDS. 2004;36:734–42.
Klitzman R, et al. It’s not just what you say: relationship of HIV disclosure and risk reduction among MSM in the post-HAART era. AIDS Care. 2007;19:749–56.
Simone J, Pantalone D. Secrets and safety in the age of AIDS: Does HIV disclosure lead to safer sex? Int AIDS Soc USA. 2004;4:109–18.
Bird J, Fingerhurt D, McKirnan. Ethnic differences in HIV-disclosure and sexual risk. AIDS Care. 2011;23:444–8.
King R, et al. Processes and outcomes of HIV serostatus disclosure to sexual partners among people living with HIV in Uganda. AIDS Behav. 2008;12:232–43.
Serovich J. A test of two HIV disclosure theories. AIDS Educ Prev. 2001;13(4):355–64.
Lovejoy N. AIDS: impact on the gay man’s homosexual and heterosexual families. Marriage Fam Rev. 1990;14:285–316.
Macklin E. AIDS: implications for families. Fam Relat. 1998;37:141–9.
Eustace R, Ilagan P. HIV disclosure among HIV positive individuals: a concept analysis. J Adv Nurs. 2010;66:2094–103.
Petrak J, et al. Factors associated with self-disclosure of HIV serostatus to significant others. British J Health Psychol. 2001;6:69–79.
Dempsey A, et al. Patterns of disclosure among youth who are HIV-positive: a multisite study. J Adolesc Health. 2012;50:315–7.
Marks G, Crepaz N. HIV-positive men’s sexual practices in the context of self-disclosure of HIV status. JAIDS. 2001;27:79–85.
Siegel K, Lune H, Meyer I. Stigma management among gay-bisexual men with HIV/AIDS. Qual Sociol. 1998;21(1):3–24.
Logie C, et al. HIV, gender, race, sexual orientation, and sex work: a qualitative study of intersectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS One. 2011;8:11.
Overstreet N, et al. Internalized stigma and HIV status disclosure among HIV-positive black men who have sex with men. AIDS Care. 2013;25(4):466–71.
C.H.A.L. Network, HIV Disclosure and the Criminal Law in Canada: Responding to the Media and the Public. Briefing paper, 2003. 30 Oct 2003.
Kalichman S, et al. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med. 2003;26(4):315–32.
Olley B, Seedat S, Stein D. Self-disclosure of HIV serostatus in recently diagnosed patients with HIV in South Africa. Afr J Reprod Health. 2004;8:71–6.
Stein M, et al. Sexual ethics. Disclosure of HIV-positive status to partners. Arch Intern Med. 1998;158:253–7.
Gorbach P, et al. Don’t ask, don’t tell: patterns of HIV disclosure among HIV positive men who have sex with men with recent STI practicing high-risk behavior in Los Angeles and Seattle. Sex Trans Infect. 2004;80:512–7.
McLean J, et al. Regular partners and risky behavior: why do gay men have unprotected intercourse? AIDS Care. 1994;6:331–41.
Obermeyer C, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: a review. Am J Public Health. 2011;101:1011–22.
Hart J, et al. Effect of directly observed therapy for highly active antiretroviral therapy on virologic, immunologic, and adherence outcomes: a meta-analysis and systematic review. JAIDS. 2010;54:167–79.
Pryzbyla S, et al. Serostatus disclosure to sexual partners among people living with HIV: examining the roles of partner characteristics and stigma. AIDS Care. 2013;25(5):566–72.
Derlega V, et al. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. J Health Psychol. 2002;7:415–32.
Wolitski R, et al. HIV serostatus disclosure among gay and bisexual men in four American cities: general patterns and relation to sexual practices. AIDS Care. 1998;10(5):599–610.
Thompson M, Aberg JA, Cahn P, et al. Antiretroviral treatment of adult HIV infection: 2010 recommendations of the international AIDS society-USA panel. JAMA. 2010;304(3):13.
Akaike H. A new look at the statistical model identification. Inst Stat Math. 1974;19:7160723.
Lin D, Wei L, Wing Z. Model-checking techniques based on cumulative residuals. Biometrics. 2002;58:1–12.
Niccolai L, et al. Disclosure of HIV status to sexual partners: predictors and temporal patterns. Sex Trans Dis. 1999;26:281–5.
Ciccarone D, et al. Sex without disclosure of positive HIV serostatus in a US probability sample of persons receiving medical care for HIV infection. Am J Public Health. 2003;93:949–54.
Kalichman S, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychol. 1999;18(3):281–7.
Gielen A, et al. Women’s lives after an HIV-positive diagnosis: disclosure and violence. Matern Child Health J. 2000;4:111–20.
Vyavaharkar M, et al. HIV-disclosure, social support, and depression among HIV-infected African American women living in the rural Southeastern United States. AIDS Educ Prev. 2011;23:78–90.
Gielen A, et al. Women living with HIV: disclosure, violence, and social support. J Urban Health. 2000;77(3):480–91.
Gielsen A, et al. Women’s lives after an HIV-positive diagnosis: disclosure & violence. Matern Child Health J. 2000;4(2):111–20.
Sowell R, et al. Disclosure of HIV infection: how do women decide to tell? Health Educ Res. 2003;18(1):32–44.
Serovich J, et al. An intervention to assist men who have sex with men disclose their serostatus to casual sex partners: results from a pilot study. AIDS Educ Prev. 2009;21:207–19.
Klitzman R. Self-disclosure of HIV status to sexual partners: a qualitative study of issues faced by gay men. J Gay Lesbian Med Assoc. 1999;3(2):39–49.
Smith R, Rossetto K, Peterson B. A meta-analysis of disclosure of one’s HIV-positive status, stigma and social support. AIDS Care. 2008;20:1266–75.
Parsons J, et al. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005;19(1):s87–97.
Schnell D, Higgins D, Wilson R. Men’s disclosure of HIV test results to male primary sex partners. Am J Public Health. 1992;82(12):1675–6.
Acknowledgments
The LISA research team is thankful for the cooperation of our various research sites. We are inspired by their amazing dedication to their clients and the communities they serve. We would especially like to thank the participants of the LISA study who trust us with sensitive and intimate information and share their stories in hopes of supporting research projects that will make a difference in their communities. We respectfully listen and interpret their experiences and hope that we are doing them justice. We are also grateful for the contributions of the LISA Community Advisory Committee: Terry Howard, Rosa Jamal, Isabella Kirchner, Sandy Lambert, Kecia Larkin, Steve Levine, Melissa Medjuck, Stacie Migwans, Sam Mohan, Lori Montgomery, Glyn Townson, Michelle Webb, Sarah White; and Study Co-Investigators: Dr. Rolando Barrios, Dr. David Burdge, Dr. Marianne Harris, Dr. David Henderson, Dr. Thomas Kerr, Dr. Julio S.G. Montaner, Dr. Thomas Patterson, Dr. Eric Roth, Dr. Mark Tyndall, Dr. Brian Willoughby, and Dr. Evan Wood. Finally, we thank colleagues who have provided additional assistance with the dataset and manuscript: David Milan, Dragan Lesovski, Anya Shen, and Svetlana Draskovic.
Conflict of interest
Dr. Robert Hogg has held grant funding from the National Institutes of Health, Canadian Institutes of Health Research National Health Research Development Program, and Health Canada. He has also received funding from GlaxoSmithKline and Merck Frosst Laboratories for participating in continued medical education programmes. Dr. Julio Montaner has received grants from Abbott, Biolytical, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck and ViiV Healthcare. He is also is supported by the Ministry of Health Services and the Ministry of Healthy Living and Sport, from the Province of British Columbia; through a Knowledge Translation Award from the Canadian Institutes of Health Research (CIHR); and through an Avant-Garde Award (No. 1DP1DA026182-01) from the National Institute of Drug Abuse, at the US National Institutes of Health. He has also received support from the International AIDS Society, United Nations AIDS Program, World Health Organization, National Institute on Drug Abuse, National Institutes of Health Research-Office of AIDS Research, National Institute of Allergy & Infectious Diseases, The United States President’s Emergency Plan for AIDS Relief (PEPfAR), Bill & Melinda Gates Foundation, French National Agency for Research on AIDS & Viral Hepatitis (ANRS), Public Health Agency of Canada. He has academic partnerships with the University of British Columbia, Simon Fraser University, Providence Health Care and Vancouver Coastal Health. This study was supported by a fund received from the Canadian Institutes for Health Research (Grant number 53396).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirsch Allen, A.J., Forrest, J.I., Kanters, S. et al. Factors Associated with Disclosure of HIV Status Among a Cohort of Individuals on Antiretroviral Therapy in British Columbia, Canada. AIDS Behav 18, 1014–1026 (2014). https://doi.org/10.1007/s10461-013-0623-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-013-0623-9