Abstract
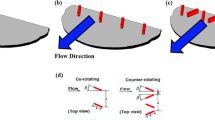
Blood damage and platelet activation are inherent problems with present day bi-leaflet mechanical heart valve designs. Passive flow control through different arrangements of vortex generators (VG) as means of improving pressure gradients and reducing turbulence are investigated. Rectangular VG arrays were mounted on the downstream surfaces of a 23 mm 3D printed mechanical valve. The effect of VGs on the resulting flow structures were assessed under pulsatile physiological flow conditions where high resolution particle image velocimetry measurement was performed. The co-rotating VGs showed lower Reynolds shear stresses and improved pressure gradients (PG) compared with the counter-rotating ones and the no-VG control one (that showed higher turbulence). RSS was found 38.13 ± 0.89, 12.95 ± 0.32, 15.75 ± 0.71, 24.54 ± 0.84 and 16.33 ± 0.58 Pa for the control, co-rotating VGs, 8 counter-rotating VGs, 4 far-spaced VGs and 4 closely-spaced VGs, respectively. PG of 10.45 ± 0.94 mmHg was obtained with co-rotating VGs and the difference was significant compared with the other configurations (control 14.88 ± 0.4 mmHg; 8 counter-rotating VGs 13.76 ± 0.51 mmHg; 4 far-spaced VGs 13.84 ± 0.09 mmHg; and 4 closely-spaced VGs 15.37 ± 0.16 mmHg). Co-rotating VGs for this application induce a more delayed flow separation and a more homogenized and streamlined transition of flow compared with the counter-rotating VGs. Passive flow control techniques deployed on BHMVs is potentially beneficial as significant control of flow at small length scales without inducing large-scale design modifications of the valve.










Similar content being viewed by others
Abbreviations
- VG:
-
Vortex generators
- PG:
-
Pressure gradient
- RSS:
-
Reynolds shear stress
- PIV:
-
Particle image velocimetry
- EOA:
-
Effective orifice area
- BMHV:
-
Bi-leaflet mechanical heart valve
References
Antiga, L., and D. A. Steinman. Rethinking turbulence in blood. Biorheology 46(2):77–81, 2009.
Baudet, E. M., et al. A 5 1/2 year experience with the St. Jude Medical cardiac valve prosthesis. Early and late results of 737 valve replacements in 671 patients. J. Thorac. Cardiovasc. Surg. 90(1):137–144, 1985.
Bradbury, L., and A. Khadem. The distortion of a jet by tabs. J. Fluid Mech. 70(4):801–813, 1975.
Cannegieter, S. C., et al. Optimal oral anticoagulant therapy in patients with mechanical heart valves. N. Engl. J. Med. 333(1):11–17, 1995.
Chandran, K. B., S. E. Rittgers, and A. P. Yoganathan. Biofluid Mechanics: The Human Circulation. Boca Raton: CRC Press, 2006.
Chang, B., et al. Long-term results with St. Jude Medical and CarboMedics prosthetic heart valves. J. Heart Valve Dis. 10(2):185–194, 2001; discussion 195.
Dale, J., and E. Myhre. Intravascular hemolysis in the late course of aortic valve replacement. Relation to valve type, size, and function. Am. Heart J. 96(1):24–30, 1978.
Dasi, L. P., et al. Passive flow control of bileaflet mechanical heart valve leakage flow. J. Biomech. 41(6):1166–1173, 2008.
Dasi, L. P., et al. Fluid mechanics of artificial heart valves. Clin. Exp. Pharmacol. Physiol. 36(2):225–237, 2009.
David, T., and C. Hsu. The integrated design of mechanical bi-leaflet prosthetic heart valves. Med. Eng. Phys. 18(6):452–462, 1996.
Dovgal, A., V. Kozlov, and A. Michalke. Laminar boundary layer separation: instability and associated phenomena. Prog. Aerosp. Sci. 30(1):61–94, 1994.
Giersiepen, M., et al. Estimation of shear stress-related blood damage in heart valve prostheses-in vitro comparison of 25 aortic valves. Int. J. Artif. Organs 13(5):300–306, 1990.
Godard, G., and M. Stanislas. Control of a decelerating boundary layer. Part 1: optimization of passive vortex generators. Aerosp. Sci. Technol. 10(3):181–191, 2006.
Govindarajan, V., et al. Impact of design parameters on bi-leaflet mechanical heart valve flow dynamics. J. Heart Valve Dis. 18(5):535, 2009.
Harker, L. A., and S. J. Slichter. Studies of platelet and fibrinogen kinetics in patients with prosthetic heart valves. N. Engl. J. Med. 283(24):1302–1305, 1970.
Hatoum, H., and L. P. Dasi. Sinus hemodynamics in representative stenotic native bicuspid and tricuspid aortic valves: an in-vitro study. Fluids 3(3):56, 2018.
Hatoum, H., F. Heim, and L. P. Dasi. Stented valve dynamic behavior induced by polyester fiber leaflet material in transcatheter aortic valve devices. J. Mech. Behav. Biomed. Mater. 86:232–239, 2018.
Hatoum, H., B. L. Moore, and L. P. Dasi. On the significance of systolic flow waveform on aortic valve energy loss. Ann. Biomed. Eng. 2018. https://doi.org/10.1007/s10439-018-2102-y.
Hatoum, H., et al. Aortic sinus flow stasis likely in valve-in-valve transcatheter aortic valve implantation. J. Thorac. Cardiovasc. Surg. 154(1):32e1–43e1, 2017.
Hatoum, H., et al. An in-vitro evaluation of turbulence after transcatheter aortic valve implantation. J. Thorac. Cardiovasc. Surg. 2018. https://doi.org/10.1016/j.jtcvs.2018.05.042.
Hatoum, H., et al. Impact of patient morphologies on sinus flow stasis in transcatheter aortic valve replacement: an in vitro study. J. Thorac. Cardiovasc. Surg. 2018. https://doi.org/10.1016/j.jtcvs.2018.05.086.
Hatoum, H., et al. Implantation depth and rotational orientation effect on valve-in-valve hemodynamics and sinus flow. Ann. Thorac. Surg. 106(1):70–78, 2018.
Hatoum, H., et al. Effect of severe bioprosthetic valve tissue ingrowth and inflow calcification on valve-in-valve performance. J. Biomech. 74:171–179, 2018.
Hatoum, H., et al. Sinus hemodynamics variation with tilted transcatheter aortic valve deployments. Ann. Biomed. Eng. 2018. https://doi.org/10.1007/s10439-018-02120-0.
Hund, S. J., J. F. Antaki, and M. Massoudi. On the representation of turbulent stresses for computing blood damage. Int. J. Eng. Sci. 48(11):1325–1331, 2010.
Hung, T., et al. Shear-induced aggregation and lysis of platelets. ASAIO J. 22(1):285–290, 1976.
Ibrahim, M., et al. The St. Jude Medical prosthesis: a thirteen-year experience. J. Thorac. Cardiovasc. Surg. 108(2):221–230, 1994.
Kameneva, M. V., et al. Effects of turbulent stresses upon mechanical hemolysis: experimental and computational analysis. ASAIO J. 50(5):418–423, 2004.
Khalili, F., P. Gamage, and H.A. Mansy. Hemodynamics of a bileaflet mechanical heart valve with different levels of dysfunction. arXiv preprint. arXiv:1711.11153, 2017.
Langan, K. J., and J. J. Samuels. Experimental investigation of maneuver performance enhancements on an advanced fighter/attack aircraft. In: AIAA 33rd Aerospace Sciences Meeting, Reno, NV, 1995.
Lin, J. Control of turbulent boundary-layer separation using micro-vortex generators. In: 30th Fluid Dynamics Conference, 1999.
Lin, J. C. Review of research on low-profile vortex generators to control boundary-layer separation. Prog. Aerosp. Sci. 38(4–5):389–420, 2002.
Masters, R., et al. Comparative results with the St. Jude Medical and Medtronic Hall mechanical valves. J. Thorac. Cardiovasc. Surg. 110(3):663–671, 1995.
Murphy, D. W., et al. Reduction of procoagulant potential of b-datum leakage jet flow in bileaflet mechanical heart valves via application of vortex generator arrays. J. Biomech. Eng. 132(7):071011, 2010.
Poller, L., et al. Managing oral anticoagulant therapy. Chest 119:22S–38S, 2001.
Quinlan, N. J., and P. N. Dooley. Models of flow-induced loading on blood cells in laminar and turbulent flow, with application to cardiovascular device flow. Ann. Biomed. Eng. 35(8):1347–1356, 2007.
Ramstack, J., L. Zuckerman, and L. Mockros. Shear-induced activation of platelets. J. Biomech. 12(2):113–125, 1979.
Simpson, R. L. Turbulent boundary-layer separation. Annu. Rev. Fluid Mech. 21(1):205–232, 1989.
Vandenmeer, F., et al. (1993) Bleeding complications in patients treated with oral anticoagulants in a routine situation. In: Thrombosis and Haemostasis. Stuttgart: FK Schattauer Verlag Gmbh.
Vongpatanasin, W., L. D. Hillis, and R. A. Lange. Prosthetic heart valves. N. Engl. J. Med. 335(6):407–416, 1996.
Williams, A. Release of serotonin from human platelets by acoustic microstreaming. J. Acoust. Soc. Am. 56(5):1640–1643, 1974.
Yin, W., et al. Flow-induced platelet activation in bileaflet and monoleaflet mechanical heart valves. Ann. Biomed. Eng. 32(8):1058–1066, 2004.
Yoganathan, A. P., Z. He, and S. Casey Jones. Fluid mechanics of heart valves. Annu. Rev. Biomed. Eng. 6:331–362, 2004.
Acknowledgments
The research done was partly supported by National Institutes of Health (NIH) under Award Number R01HL119824 and R01HL135505.
Conflict of interest
Dr. Dasi reports having two patent applications on novel surgical and transcatheter valves. He also has a patent issued on vortex generators on heart valves and a patent application on super hydrophobic vortex generator enhanced mechanical heart valves. No other conflicts were reported.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Aleksander S. Popel oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1 Fluid particles streaks for every valve case in every model over the cardiac cycle (AVI 9111 kb)
Rights and permissions
About this article
Cite this article
Hatoum, H., Dasi, L.P. Reduction of Pressure Gradient and Turbulence Using Vortex Generators in Prosthetic Heart Valves. Ann Biomed Eng 47, 85–96 (2019). https://doi.org/10.1007/s10439-018-02128-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-018-02128-6