Abstract
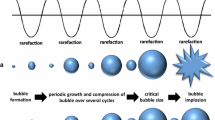
Therapeutic approaches that enhance thrombolysis by combining recombinant tissue plasminogen activator (rtPA), ultrasound, and/or microbubbles (MBs) are known as sonothrombolysis techniques. To date, sonothrombolysis approaches have primarily utilized commercially available MB formulations (or derivatives thereof) with diameters in the range 1–4 µm and circulation lifetimes between 5 and 15 min. The present study evaluated the in vitro sonothrombolysis efficacy of large diameter MBs (d MB ≥ 10 µm) with much shorter lifetimes that were produced on demand and in close proximity to the blood clot using a flow-focusing microfluidic device. MBs with a N2 gas core and a non-crosslinked bovine serum albumin shell were produced with diameters between 10 and 20 µm at rates between 50 and 950 × 103 per second. Use of these large MBs resulted in approximately 4.0–8.8 fold increases in thrombolysis rates compared to a clinical rtPA dose and approximately 2.1–4.2 fold increases in thrombolysis rates compared to sonothrombolysis techniques using conventional MBs. The results of this study indicate that the large diameter microbubbles with transient stability are capable of significantly enhanced in vitro sonothrombolysis rates when delivered directly to the clot immediately following production by a flow focusing microfluidic device placed essentially in situ adjacent to the clot.





Similar content being viewed by others
References
Acconcia, C. N., B. Y. Leung, and D. E. Goertz. The microscale evolution of the erosion front of blood clots exposed to ultrasound stimulated microbubbles. J. Acoust. Soc. Am. 139:135, 2016.
Acconcia, C., B. Y. C. Leung, A. Manjunath, and D. E. Goertz. Interactions between individual ultrasound-stimulated microbubbles and fibrin clots. Ultrasound Med. Biol. 40:2134–2150, 2014.
Ahadi, G., et al. Transcranial sonothrombolysis using high-intensity focused ultrasound: impact of increasing output power on clot fragmentation. J. Ther. Ultrasound 1:22, 2013.
Alexandrov, A. V., et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N. Engl. J. Med. 351:2170–2178, 2004.
Bader, K. B., M. J. Gruber, and C. K. Holland. Shaken and stirred: mechanisms of ultrasound-enhanced thrombolysis. Ultrasound Med. Biol. 41:187–196, 2015.
Borrelli, M. J., et al. Influences of microbubble diameter and ultrasonic parameters on in vitro sonothrombolysis efficacy. J. Vasc. Interv. Radiol. 23:1677–1684, 2012.
Brujan, E. A., T. Ikeda, and Y. Matsumoto. Jet formation and shock wave emission during collapse of ultrasound-induced cavitation bubbles and their role in the therapeutic applications of high-intensity focused ultrasound. Phys. Med. Biol. 50:4797, 2005.
Brujan, E.-A., and Y. Matsumoto. Collapse of micrometer-sized cavitation bubbles near a rigid boundary. Microfluid Nanofluidics 13:957–966, 2012.
Chen, J. L., A. H. Dhanaliwala, A. J. Dixon, A. L. Klibanov, and J. A. Hossack. Synthesis and characterization of transiently stable albumin-coated microbubbles via a flow-focusing microfluidic device. Ultrasound Med. Biol. 40:400–409, 2014.
Chuang, Y. H., P. W. Cheng, and P. C. Li. Combining radiation force with cavitation for enhanced sonothrombolysis. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 60:97–104, 2013.
Daffertshofer, M., et al. Transcranial low-frequency ultrasound-mediated thrombolysis in brain ischemia: increased risk of hemorrhage with combined ultrasound and tissue plasminogen activator: results of a phase II clinical trial. Stroke 36:1441–1446, 2005.
Datta, S., et al. Correlation of cavitation with ultrasound enhancement of thrombolysis. Ultrasound Med. Biol. 32:1257–1267, 2006.
Dayton, P. A., J. S. Allen, and K. W. Ferrara. The magnitude of radiation force on ultrasound contrast agents. J. Acoust. Soc. Am. 112:2183–2192, 2002.
Dhanaliwala, A. H., J. L. Chen, S. Wang, and J. A. Hossack. Liquid flooded flow-focusing microfluidic device for in situ generation of monodisperse microbubbles. Microfluid Nanofluidics 14:457–467, 2013.
Dhanaliwala, A. H., et al. In vivo imaging of microfluidic-produced microbubbles. Biomed. Microdevices 17:23, 2015.
Dixon, A. J., A. H. Dhanaliwala, J. L. Chen, and J. A. Hossack. Enhanced intracellular delivery of a model drug using microbubbles produced by a microfluidic device. Ultrasound Med. Biol. 39:1267–1276, 2013.
Dixon, A. J., et al. Microbubble-mediated intravascular ultrasound imaging and drug delivery. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 62:1674–1685, 2015.
Enden, T., et al. Long-term outcome after additional catheter-directed thrombolysis vs. standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study): a randomised controlled trial. The Lancet 379:31–38, 2012.
Go, A. S., et al. Heart disease and stroke statistics—2014 update a report from the American Heart Association. Circulation 129:e28–e292, 2014.
Goertz, D., C. Acconcia, and B. Leung. Microscale interactions between ultrasound stimulated microbubbles and the fibrin networks of clots. J. Acoust. Soc. Am. 138:1819, 2015.
Helps, S. C., M. Meyer-Witting, P. L. Reilly, and D. F. Gorman. Increasing doses of intracarotid air and cerebral blood flow in rabbits. Stroke 21:1340–1345, 1990.
Hettiarachchi, K., E. Talu, M. L. Longo, P. A. Dayton, and A. P. Lee. On-chip generation of microbubbles as a practical technology for manufacturing contrast agents for ultrasonic imaging. Lab. Chip 7:463, 2007.
Kearon, C. Natural history of venous thromboembolism. Circulation 107:I-22–I-30, 2003.
Klibanov, A. L., et al. Targeting of ultrasound contrast material: selective imaging of microbubbles in vitro. Acad. Radiol. 5(Suppl 1):S243–S246, 1998.
Liebeskind, D. S., et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke 42:1237–1243, 2011.
Marler, J. Tissue plasminogen activator for acute ischemic stroke. N. Engl. J. Med. 333:1581–1588, 1995.
Marmottant, P., and S. Hilgenfeldt. A bubble-driven microfluidic transport element for bioengineering. Proc. Natl. Acad. Sci. U.S.A. 101:9523–9527, 2004.
Molina, C. A., et al. Transcranial ultrasound in clinical sonothrombolysis (TUCSON) trial. Ann. Neurol. 66:28–38, 2009.
O’Reilly, M. A., Y. Huang, and K. Hynynen. Impact of standing wave effects on transcranial focused ultrasound disruption of the blood-brain barrier in a rat model. Phys. Med. Biol. 55:5251–5267, 2010.
Owen, J., P. Grove, P. Rademeyer, and E. Stride. The influence of blood on targeted microbubbles. J. R. Soc. Interface 11(100):20140622, 2014.
Petit, B., et al. Sonothrombolysis: the contribution of stable and inertial cavitation to clot lysis. Ultrasound Med. Biol. 41:1402–1410, 2015.
Ribo, M., et al. Intra-arterial administration of microbubbles and continuous 2-MHz ultrasound insonation to enhance intra-arterial thrombolysis. J. Neuroimaging 20:224–227, 2010.
Roessler, F. C., et al. The platelet-rich plasma clot: a standardized in vitro clot formation protocol for investigations of sonothrombolysis under physiological flows. Blood Coag. Fibrinol. 22:407–415, 2011.
Schwamm, L. H., et al. Temporal trends in patient characteristics and treatment with intravenous thrombolysis among acute ischemic stroke patients at get with the guidelines-stroke hospitals. Circ. Cardiovasc. Qual. Outcomes 6(5):543–549, 2013.
Sutton, J. T., N. M. Ivancevich, S. R. Perrin, D. C. Vela, and C. K. Holland. Clot retraction affects the extent of ultrasound-enhanced thrombolysis in an ex vivo porcine thrombosis model. Ultrasound Med. Biol. 39:813–824, 2013.
Unnikrishnan, S., and A. L. Klibanov. Microbubbles as ultrasound contrast agents for molecular imaging: preparation and application. AJR Am. J. Roentgenol. 199:292–299, 2012.
Wang, S., A. H. Dhanaliwala, J. L. Chen, and J. A. Hossack. Production rate and diameter analysis of spherical monodisperse microbubbles from two-dimensional, expanding-nozzle flow-focusing microfluidic devices. Biomicrofluidics 7:014103, 2013.
Weiss, H. L., et al. Mechanical clot damage from cavitation during sonothrombolysis. J. Acoust. Soc. Am. 133:3159–3175, 2013.
Acknowledgments
Partial support for this research is provided by the National Institutes of Health under Grant NIH S10 RR025594 to JAH and by NSF GRFP and Virginia Space Grant Consortium pre-doctoral fellowships to AJD. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NSF, or VGSC.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Agata A. Exner oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.

10439_2017_1965_MOESM1_ESM.gif
Supplementary Video 1: Video (30 FPS) of 25 s of a sonothrombolysis experiment (Group F). The effect of radiation force on the stream of MBs is evident as the stream is pushed onto the surface of the clot when the ultrasound is on, and is separated from the clot when the ultrasound is off. The experiments were performed with 2 s of ultrasound application followed by 2 s of no ultrasound, repeated for the 30 min duration of the experiment. Supplementary material 1 (GIF 3066 kb)
Supplementary Video 2: Compilation of still images taken at 1 min intervals during a 30 min sonothrombolysis experiment (Group F). For reference, the ID of the tube is 3.05 mm. Supplementary material 2 (WMV 3174 kb)
Rights and permissions
About this article
Cite this article
Dixon, A.J., Rickel, J.M.R., Shin, B.D. et al. In Vitro Sonothrombolysis Enhancement by Transiently Stable Microbubbles Produced by a Flow-Focusing Microfluidic Device. Ann Biomed Eng 46, 222–232 (2018). https://doi.org/10.1007/s10439-017-1965-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-017-1965-7