Abstract
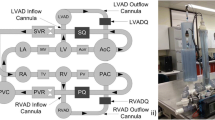
Rotary left ventricular assist devices (LVADs) show weaker response to preload and greater response to afterload than the native heart. This may lead to ventricular suction or pulmonary congestion, which can be deleterious to the patient’s recovery. A physiological control system which optimizes responsiveness of LVADs may reduce adverse events. This study compared eight physiological control systems for LVAD support against constant speed mode. Pulmonary (PVR) and systemic (SVR) vascular resistance changes, a passive postural change and exercise were simulated in a mock circulation loop to evaluate the controller’s ability to prevent suction and congestion and to increase exercise capacity. Three active and one passive control systems prevented ventricular suction at high PVR (500 dyne s cm−5) and low SVR (600 dyne s cm−5) by decreasing LVAD speed (by 200–515 rpm) and by increasing LVAD inflow cannula resistance (up to 1000 dyne s cm−5) respectively. These controllers increased LVAD preload sensitivity (to 0.196–2.415 L min−1 mmHg−1) compared to the other control systems and constant speed mode (0.039–0.069 L min−1 mmHg−1). The same three active controllers increased pump speed (600–800 rpm) and thus LVAD flow by 4.5 L min−1 during exercise which increased exercise capacity. Physiological control systems that prevent adverse events and/or increase exercise capacity may help improve LVAD patient conditions.






Similar content being viewed by others
References
AlOmari, A.-H. H., A. V. Savkin, M. Stevens, D. G. Mason, D. L. Timms, R. F. Salamonsen, and N. H. Lovell. Developments in control systems for rotary left ventricular assist devices for heart failure patients: a review. Physiol. Meas. 34:R1–R27, 2013.
Boston, J. R., J. F. Antaki, and M. A. Simaan. Hierarchical control of heart-assist devices. Robot. Autom. Mag. 10(1):54–64, 2003.
Bullister, E., S. Reich, and J. Sluetz. Physiologic control algorithms for rotary blood pumps using pressure sensor input. Artif. Organs. 26:931–938, 2002.
Casas, F., N. Ahmed, and A. Reeves. Minimal sensor count approach to fuzzy logic rotary blood pump flow control. ASAIO J. 53:140–146, 2007.
Eckberg, D. L., M. Drabinsky, and E. Braunwald. Defective cardiac parasympathetic control in patients with heart disease. N. Engl. J. Med. 285:877–883, 1971.
Epstein, S. E., G. D. Beiser, M. Stampfer, B. F. Robinson, and E. Braunwald. Characterization of the circulatory response to maximal upright exercise in normal subjects and patients with heart disease. Circulation. 35:1049–1062, 1967.
Gaddum, N. R., M. Stevens, E. Lim, J. Fraser, N. Lovell, D. Mason, D. Timms, and R. Salamonsen. Starling-like flow control of a left ventricular assist device: in vitro validation. Artif. Organs. 38:E46–E56, 2014.
Giridharan, G. A., and M. Skliar. Control strategy for maintaining physiological perfusion with rotary blood pumps. Artif. Organs. 27:639–648, 2003.
Gregory, S. D., M. J. Pearcy, and D. Timms. Passive control of a biventricular assist device with compliant inflow cannulae. Artif. Organs. 36:683–690, 2012.
Gregory, S. D., M. Stevens, D. Timms, and M. Pearcy. Replication of the Frank-Starling response in a mock circulation loop. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2011:6825–6828, 2011.
Klabunde, R. E. Cardiovascular Physiology Concepts. Baltimore: Lippincott Williams & Wilkins, 2010.
Lim, E., R. F. Salamonsen, M. Mansouri, N. Gaddum, D. G. Mason, D. L. Timms, M. C. Stevens, J. Fraser, R. Akmeliawati, and N. H. Lovell. Hemodynamic response to exercise and head-up tilt of patients implanted with a rotary blood pump: a computational modeling study. Artif. Organs. 39:E24–E35, 2015.
McClean, D., J. Aragon, A. Jamali, S. Kar, J. Ritzema-Carter, R. Troughton, H. Krum, R. Doughty, W. T. Abraham, J. S. Whiting, and N. Eigler. Noninvasive calibration of cardiac pressure transducers in patients with heart failure: an aid to implantable hemodynamic monitoring and therapeutic guidance. J. Card. Fail. 12:568–576, 2006.
Moscato, F., M. Arabia, F. M. Colacino, P. Naiyanetr, G. A. Danieli, and H. Schima. Left ventricle afterload impedance control by an axial flow ventricular assist device: a potential tool for ventricular recovery. Artif. Organs. 34:736–744, 2010.
Pauls, J. P., Stevens, M. C., Schummy, E., Tansley, G., Fraser, J. F., Timms, D., Gregory, S.D. In vitro comparison of active and passive physiological control systems for biventricular assist devices. Ann. Biomed. Eng., 2015. doi:10.1007/s10439-015-1425-1.
Reesink, K., A. Dekker, Nagel T. Van Der, C. Beghi, F. Leonardi, P. Botti, Cicco G. De, R. Lorusso, Veen F. Van Der, and J. Maessen. Suction due to left ventricular assist : implications for device control and management. Artif. Organs. 31:542–549, 2007.
Rose, E. A., A. J. Moskowitz, M. Packer, J. A. Sollano, D. L. Williams, A. R. Tierney, D. F. Heitjan, P. Meier, D. D. Ascheim, R. G. Levitan, A. D. Weinberg, L. W. Stevenson, P. A. Shapiro, R. M. Lazar, J. T. Watson, D. J. Goldstein, and A. C. Gelijns. The REMATCH trial: rationale, design, and end points. Ann. Thorac. Surg. 67:723–730, 1999.
Salamonsen, R. F., D. G. Mason, and P. J. Ayre. Response of rotary blood pumps to changes in preload and afterload at a fixed speed setting are unphysiological when compared with the natural heart. Artif. Organs. 35:E47–E53, 2011.
Salamonsen, R. F., V. Pellegrino, J. F. Fraser, K. Hayes, D. Timms, N. H. Lovell, and C. Hayward. Exercise studies in patients with rotary blood pumps: cause, effects, and implications for Starling-like control of changes in pump flow. Artif. Organs. 37:695–703, 2013.
Slaughter, M. S., F. D. Pagani, J. G. Rogers, L. W. Miller, B. Sun, S. D. Russell, R. C. Starling, L. Chen, A. J. Boyle, S. Chillcott, R. M. Adamson, M. S. Blood, M. T. Camacho, K. A. Idrissi, M. Petty, M. Sobieski, S. Wright, T. J. Myers, and D. J. Farrar. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J. Hear. Lung Transplantationl Soc. Hear. Transplant. 29:S1–39, 2010.
Stevens, M. C., S. Wilson, A. Bradley, J. Fraser, and D. Timms. Physiological control of dual rotary pumps as a biventricular assist device using a master/slave approach. Artif. Organs. 38:766–774, 2014.
Timms, D. L., S. D. Gregory, N. A. Greatrex, M. J. Pearcy, J. F. Fraser, and U. Steinseifer. A compact mock circulation loop for the in vitro testing of cardiovascular devices. Artif. Organs. 35:384–391, 2011.
Troughton, R. W., J. Ritzema, N. L. Eigler, I. C. Melton, H. Krum, P. B. Adamson, S. Kar, P. K. Shah, J. S. Whiting, J. T. Heywood, S. Rosero, J. P. Singh, L. Saxon, R. Matthews, I. G. Crozier, and W. T. Abraham. Direct left atrial pressure monitoring in severe heart failure: long-term sensor performance. J. Cardiovasc. Transl. Res. 4:3–13, 2011.
Vollkron, M., H. Schima, L. Huber, R. Benkowski, G. Morello, and G. Wieselthaler. Development of a suction detection system for axial blood pumps. Artif. Organs. 28:709–716, 2004.
Wu, Y., P. E. Allaire, G. Tao, M. Adams, Y. Liu, H. Wood, and D. B. Olsen. A bridge from short-term to long-term left ventricular assist device–experimental verification of a physiological controller. Artif. Organs. 28:927–932, 2004.
Acknowledgements
The authors would like to recognize the financial assistance provided by The Prince Charles Hospital Foundation (NR2013-222 and PRO2014-08), the ACTIONS National Health and Medical Research Council Centre for Research Excellence (APP1079421), Queensland Health Research Fellowship and Griffith University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ellen Kuhl oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Pauls, J.P., Stevens, M.C., Bartnikowski, N. et al. Evaluation of Physiological Control Systems for Rotary Left Ventricular Assist Devices: An In-Vitro Study. Ann Biomed Eng 44, 2377–2387 (2016). https://doi.org/10.1007/s10439-016-1552-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-016-1552-3