Abstract
The assessment of functional coronary lesion severity using intracoronary hemodynamic parameters like the pressure-derived fractional flow reserve and the flow-derived coronary flow reserve are known to rely critically on the establishment of maximal hyperemia. We evaluated a hyperemia-free index, basal pressure drop coefficient (bCDP), that combines pressure and velocity for simultaneous assessment of the status of both epicardial and microvascular circulations. In 23 pigs, simultaneous measurements of distal coronary arterial pressure and flow were performed using a dual-sensor tipped guidewire in the settings of both normal and abnormal microcirculation with the presence of epicardial lesions of area stenosis (AS) < 50% and AS > 50%. The bCDP, a parameter based on fundamental fluid dynamics principles, was calculated as the transtenotic pressure-drop divided by the dynamic pressure in the distal vessel, measured under baseline (without hyperemia) conditions. The group mean values of bCDP for normal (84 ± 18) and abnormal (124.5 ± 15.6) microcirculation were significantly different. Similarly, the mean values of bCDP from AS < 50% (72.5 ± 16.1) and AS > 50% (136 ± 17.2) were also significantly different (p < 0.05). The bCDP could significantly distinguish between lesions of AS < 50% to AS > 50% under normal microcirculation (52.1 vs. 85.8; p < 0.05) and abnormal microcirculation (84.9 vs. 172; p < 0.05). Further, the bCDP correlated linearly and significantly with the hyperemic parameters FFR (r = 0.42, p < 0.05) and CDP (r = 0.50, p < 0.05). The bCDP is a promising clinical diagnostic parameter that can independently assess the severity of epicardial stenosis and microvascular impairment. We believe that it has an immediate appeal for detection of coronary artery disease if validated clinically.









Similar content being viewed by others
References
Banerjee, R. K., K. D. Ashtekar, M. A. Effat, T. A. Helmy, E. Kim, E. W. Schneeberger, R. A. Sinha, W. M. Gottliebson, and L. H. Back. Concurrent assessment of epicardial coronary artery stenosis and microvascular dysfunction using diagnostic endpoints derived from fundamental fluid dynamics principles. J. Invasive Cardiol. 21:511–517, 2009.
Banerjee, R. K., A. Sinha Roy, L. H. Back, M. R. Back, S. F. Khoury, and R. W. Millard. Characterizing momentum change and viscous loss of a hemodynamic endpoint in assessment of coronary lesions. J. Biomech. 40:652–662, 2007.
Cubero, J. M., L. S. D. de la Llera, P. C. García, M. V. Gil-Ortega, J. B. Mazuecos, and A. Sanchez-Gonzalez. A comparative study between intravenous and intracoronary administration of high doses adenosine for fractional flow reserve measurements, in the “fame” era. J. Am. Coll. Cardiol. 59:E1465–E1465, 2012.
Cumming, G., F. Fidler, and D. L. Vaux. Error bars in experimental biology. J. Cell Biol. 177:7–11, 2007.
De Bruyne, B., N. H. J. Pijls, E. Barbato, J. Bartunek, J.-W. Bech, W. Wijns, and G. R. Heyndrickx. Intracoronary and intravenous adenosine 5′-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation 107:1877–1883, 2003.
Fearon, W. F., L. B. Balsam, H. M. O. Farouque, R. C. Robbins, P. J. Fitzgerald, P. G. Yock, and A. C. Yeung. Novel index for invasively assessing the coronary microcirculation. Circulation 107:3129–3132, 2003.
Heusch, G. Adenosine and maximum coronary vasodilation in humans: myth and misconceptions in the assessment of coronary reserve. Basic Res. Cardiol. 105:1–5, 2010.
Hoffman, J. I. Problems of coronary flow reserve. Ann. Biomed. Eng. 28:884–896, 2000.
Jeremias, A., R. J. Whitbourn, S. D. Filardo, P. J. Fitzgerald, D. J. Cohen, E. M. Tuzcu, W. D. Anderson, A. A. Abizaid, G. S. Mintz, A. C. Yeung, et al. Adequacy of intracoronary vs. intravenous adenosine-induced maximal coronary hyperemia for fractional flow reserve measurements. Am. Heart J. 140:651–657, 2000.
Kern, M. J. Coronary physiology revisited: practical insights from the cardiac catheterization laboratory. Circulation 101:1344–1351, 2000.
Kern, M. J., A. Lerman, J. W. Bech, B. De Bruyne, E. Eeckhout, W. F. Fearon, S. T. Higano, M. J. Lim, M. Meuwissen, J. J. Piek, et al. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation 114:1321–1341, 2006.
Kim, J. S., H. D. Lee, Y. K. Suh, J. H. Kim, K. J. Chun, Y. H. Park, J. Kim, D. C. Han, and C. B. Sohn. Prediction of fractional flow reserve without hyperemic induction based on resting baseline Pd/Pa. Korean Circ. J. 43:309–315, 2013.
Kleiman, N. S. Bringing it all together: integration of physiology with anatomy during cardiac catheterization. J. Am. Coll. Cardiol. 58:1219–1221, 2011.
Kolli, K. K., R. K. Banerjee, S. V. Peelukhana, M. A. Effat, M. A. Leesar, I. Arif, E. W. Schneeberger, P. Succop, W. M. Gottliebson, and T. A. Helmy. Effect of changes in contractility on pressure drop coefficient and fractional flow reserve in a porcine model. J Invasive Cardiol. 24:6–12, 2012.
Kolli, K. K., R. K. Banerjee, S. V. Peelukhana, T. A. Helmy, M. A. Leesar, I. Arif, E. W. Schneeberger, D. Hand, P. Succop, W. M. Gottliebson, and M. A. Effat. Influence of heart rate on fractional flow reserve, pressure drop coefficient, and lesion flow coefficient for epicardial coronary stenosis in a porcine model. Am. J. Physiol. Heart Circ. Physiol. 300:H382–H387, 2011.
Kolli, K. K., T. A. Helmy, S. V. Peelukhana, I. Arif, M. A. Leesar, L. H. Back, R. K. Banerjee, and M. A. Effat. Functional diagnosis of coronary stenoses using pressure drop coefficient: a pilot study in humans. Catheter. Cardiovasc. Interv. 83:377–385, 2014.
Kolli, K. K., A. K. Paul, L. H. Back, M. A. Effat, and R. K. Banerjee. Optimization of balloon obstruction for simulating equivalent pressure drop in physiological stenoses. Biorheology 50:257–268, 2013.
Leone, A. M., I. Porto, A. R. De Caterina, E. Basile, A. Aurelio, A. Gardi, D. Russo, D. Laezza, G. Niccoli, F. Burzotta, et al. Maximal hyperemia in the assessment of fractional flow reserve: intracoronary adenosine vs. intracoronary sodium nitroprusside vs. intravenous adenosine: The NASCI (Nitroprussiato vs. Adenosina nelle Stenosi Coronariche Intermedie) Study. JACC Cardiovasc. Interv. 5:402–408, 2012.
MacCarthy, P., A. Berger, G. Manoharan, J. Bartunek, E. Barbato, W. Wijns, G. R. Heyndrickx, N. H. Pijls, and B. De Bruyne. Pressure-derived measurement of coronary flow reserve. J. Am. Coll. Cardiol. 45:216–220, 2005.
Members, W. C., S. C. Smith, T. E. Feldman, J. W. Hirshfeld, A. K. Jacobs, M. J. Kern, S. B. King, D. A. Morrison, W. W. O’Neill, H. V. Schaff, et al. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention—Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). Circulation 113:156–175, 2006.
Meuwissen, M., M. Siebes, S. A. Chamuleau, B. L. van Eck-Smit, K. T. Koch, R. J. de Winter, J. G. Tijssen, J. A. Spaan, and J. J. Piek. Hyperemic stenosis resistance index for evaluation of functional coronary lesion severity. Circulation 106:441–446, 2002.
Payton, M. E., M. H. Greenstone, and N. Schenker. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J. Insect Sci. 3:34, 2003.
Peelukhana, S. V., L. H. Back, and R. K. Banerjee. Influence of coronary collateral flow on coronary diagnostic parameters: an in vitro study. J. Biomech. 42:2753–2759, 2009.
Peelukhana, S. V., R. K. Banerjee, K. K. Kolli, M. A. Effat, T. A. Helmy, M. A. Leesar, E. W. Schneeberger, P. Succop, W. Gottliebson, and I. Arif. Effect of heart rate on hemodynamic endpoints under concomitant microvascular disease in a porcine model. Am. J. Physiol. Heart Circ. Physiol. 302:H1563–H1573, 2012.
Peelukhana, S. V., K. K. Kolli, M. A. Leesar, M. A. Effat, T. A. Helmy, I. Arif, E. W. Schneeberger, P. Succop, and R. K. Banerjee. Effect of myocardial contractility on hemodynamic end points under concomitant microvascular disease in a porcine model. Heart Vessels 29:97–109, 2014.
Pijls, N. H., M. J. Kern, P. G. Yock, and B. De Bruyne. Practice and potential pitfalls of coronary pressure measurement. Catheter. Cardiovasc. Interv. 49:1–16, 2000.
Pijls, N. H., and P. A. Tonino. The crux of maximum hyperemia: the last remaining barrier for routine use of fractional flow reserve. JACC Cardiovasc. Interv. 4:1093–1095, 2011.
Pijls, N. H., B. Van Gelder, P. Van der Voort, K. Peels, F. A. Bracke, H. J. Bonnier, and M. I. el Gamal. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 92:3183–3193, 1995.
Pijls, N. H., P. van Schaardenburgh, G. Manoharan, E. Boersma, J. W. Bech, M. van’t Veer, F. Bar, J. Hoorntje, J. Koolen, W. Wijns, and B. de Bruyne. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J. Am. Coll. Cardiol. 49:2105–2111, 2007.
Sen, S., J. Escaned, I. S. Malik, G. W. Mikhail, R. A. Foale, R. Mila, J. Tarkin, R. Petraco, C. Broyd, R. Jabbour, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) Study. J. Am. Coll. Cardiol. 59:1392–1402, 2012.
Siebes, M., B. J. Verhoeff, M. Meuwissen, R. J. de Winter, J. A. Spaan, and J. J. Piek. Single-wire pressure and flow velocity measurement to quantify coronary stenosis hemodynamics and effects of percutaneous interventions. Circulation 109:756–762, 2004.
Silber, S., P. Albertsson, F. F. Aviles, P. G. Camici, A. Colombo, C. Hamm, E. Jorgensen, J. Marco, J. E. Nordrehaug, W. Ruzyllo, et al. Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur. Heart J. 26:804–847, 2005.
Sinha Roy, A., M. R. Back, S. F. Khoury, E. W. Schneeberger, L. H. Back, V. V. Velury, R. W. Millard, and R. K. Banerjee. Functional and anatomical diagnosis of coronary artery stenoses. J. Surg. Res. 150:24–33, 2008.
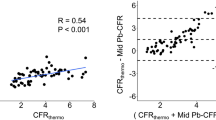
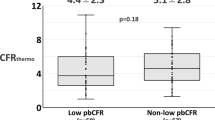
van de Hoef, T. P., F. Nolte, P. Damman, R. Delewi, M. Bax, S. A. J. Chamuleau, M. Voskuil, M. Siebes, J. G. P. Tijssen, J. A. E. Spaan, et al. Diagnostic accuracy of combined intracoronary pressure and flow velocity information during baseline conditions: adenosine-free assessment of functional coronary lesion severity. Circ. Cardiovasc. Interv. 5:508–514, 2012.
van de Hoef, T. P., F. Nolte, M. C. Rolandi, J. J. Piek, J. P. van den Wijngaard, J. A. Spaan, and M. Siebes. Coronary pressure-flow relations as basis for the understanding of coronary physiology. J. Mol. Cell. Cardiol. 52:786–793, 2012.
Wijns, W., and P. H. Kolh. Experience with revascularization procedures does matter: low volume means worse outcome. Eur. Heart J. 31:1954–1957, 2010.
Acknowledgments
The authors are grateful to Dr. Mahesh Krishnamoorthy, Dr. Subhashish Das Gupta, Marwan Al-Rjoub and Bhaskar Konala of Transport in Engineering and Medicine Laboratory at University of Cincinnati for their assistance during the experiments. This study is supported by Grant-In-Aid of Great Rivers Affiliate, National-Scientific Development Grant of American Heart Association (Grant reference #s: 0755236B and 0335270N) and a Department of Veteran Affairs Merit Review Grant (I01CX000342).
Disclosure
The authors report no financial relationships or conflicts of interest regarding the content herein.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Dan Elson oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Kolli, K.K., Effat, M.A., Peelukhana, S.V. et al. Hyperemia-Free Delineation of Epicardial and Microvascular Impairments Using a Basal Index. Ann Biomed Eng 42, 1681–1690 (2014). https://doi.org/10.1007/s10439-014-1020-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-014-1020-x