Abstract
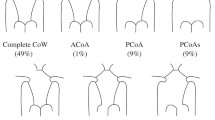
A complete circle of Willis (CoW) is found in approximately 30–50% of the population. Anatomical variations, such as absent or surgically clamped vessels, can result in undesirable flow patterns. These can affect the brain’s ability to maintain cerebral perfusion and the formation of cerebral aneurysms. An experimental test system was developed to simulate cerebral physiological conditions through three flexible 3D patient-specific models of complete and incomplete CoW geometries. Flow visualizations were performed with isobaric dyes and the mapped dye streamlines were tracked throughout the models. Three to seven flow impact locations were observed for all configurations, corresponding to known sites for aneurysmal formation. Uni and bi-directional cross-flows occurred along the communicating arteries. The greatest shunting of flow occurred for a missing pre-communicating anterior (A1) and posterior (P1) cerebral arteries. The anterior cerebral arteries had the greatest reduction (15–37%) in efferent flow rates for missing either a unilateral A1 or bilateral P1 segments. The bi-directional cross-flows, with multiple afferent flow mixing, observed along the communicating arteries may explain the propensity of aneurysm formation at these sites. Reductions in efferent flow rates due to aplastic vessel configurations may affect normal brain function.









Similar content being viewed by others
References
Alastruey, J., K. H. Parker, J. Peiró, S. M. Byrd, and S. J. Sherwin. Modeling the circle of Willis to assess the effects of anatomical variations and occlusions on cerebral flows. J. Biomech. 40(8):1794–1805, 2007.
Asakura, F., H. Yilmaz, G. Sekoranja, et al. Preclinical testing of a new clot-retrieving wire device using polyvinyl alcohol hydrogel vascular models. Neuroradiology 49(3):243–251, 2007.
Cassot, F., M. Zagzoule, and J. P. Marc-Vergnes. Hemodynamic role of circle of Willis in stenoses of internal carotid arteries. An analytical solution of a linear model. J. Biomech. 33(4):395–405, 2000.
Chadwick, A., and J. Morfett. Hydraulics in Civil and Environmental Engineering. London: Chapman and Hall, pp. 375–378, 1997.
Chung, E. M. L., J. P. Hague, M.-A. Chanrion, K. V. Ramnarine, E. Katsogridakis, and D. H. Evans. Embolus trajectory through a physical replica of the major cerebral arteries. Stroke 41(4):647–652, 2010.
Ciceri, E. F., R. P. Klucznik, R. G. Grossman, J. E. Rose, and M. E. Mawad. Endovascular treatment of peripheral aneurysms of the posterior inferior cerebellar artery. Am. J. Neuroradiology 22(1):27–34, 2001.
Devault, K., P. A. Gremaud, V. Novak, M. S. Olufsen, G. Vernières, and P. Zhao. Blood flow in the circle of Willis: modeling and calibration. Multiscale Model Simul. 7(2):888–909, 2008.
Fahrig, R., H. Nikolov, A. J. Fox, and D. W. Holdsworth. A three-dimensional cerebrovascular flow phantom. Med. Phys. 26(8):1589–1599, 1999.
Ford, M. D., N. Alperin, S. H. Lee, D. W. Holdsworth, and D. A. Steinman. Characterization of volumetric flow rate waveforms in the normal internal carotid and vertebral arteries. Physiol. Meas. 26(4):477–488, 2005.
Günther, M. Magnetic resonance techniques to measure distribution of cerebral blood flow. Appl. Cardiopulm. Pathophysiol. 13:212–218, 2009.
Henderson, R. D., M. Eliasziw, A. J. Fox, P. M. Rothwell, and H. J. Barnett. Angiographically defined collateral circulation and risk of stroke in patients with severe carotid artery stenosis. North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group. Stroke 31:128–132, 2000.
Hendrikse, J., M. J. Hartkamp, B. Hillen, W. P. T. M. Mali, and J. V. D. Grond. Collateral ability of the circle of Willis in patients with unilateral internal carotid artery occlusion: border zone infarcts and clinical symptoms. Stroke 32(12):2768–2773, 2001.
Hoksbergen, A. W., B. Fülesdi, D. A. Legemate, and L. Csiba. Collateral configuration of the circle of Willis: transcranial color-coded duplex ultrasonography and comparison with postmortem anatomy. Stroke 31(6):1346–1351, 2000.
Hoksbergen, A. W. J., C. B. L. Majoie, F.-J. H. Hulsmans, and D. A. Legemate. Assessment of the collateral function of the circle of Willis: three-dimensional time-of-flight MR angiography compared with transcranial color-coded duplex sonography. Am. J. Neuroradiol. 24(3):456–462, 2003.
Jou, L.-D., D. H. Lee, and M. E. Mawad. Cross-flow at the anterior communicating artery and its implication in cerebral aneurysm formation. J. Biomech. 43(11):2189–2195, 2010.
Kayembe, K. N., M. Sasahara, and F. Hazama. Cerebral aneurysms and variations in the circle of Willis. Stroke 15(5):846–850, 1984.
Knox, K., C. W. Kerber, S. Singel, et al. Stereolithographic vascular replicas from CT scans: choosing treatment strategies, teaching, and research from live patient scan data. Am. J. Neuroradiol. 26(6):1428–1431, 2005.
Krabbe-Hartkamp, M. J., J. Van Der Grond, F. De Leeuw, J. De Groot, A. Algra, B. Hillen, M. Breteler, and W. Mali. Circle of Willis: morphologic variation on three-dimensional time-of-flight MR angiograms. Radiology 207(1):798–805, 1998.
Krings, T., D. M. Mandell, T.-R. Kiehl, S. Geibprasert, M. Tymianski, H. Alvarez, K. G. Terbrugge, and F.-J. Hans. Intracranial aneurysms: from vessel wall pathology to therapeutic approach. Nat. Rev. Neurol. 7(10):547–559, 2011.
Kudo, T. An operative complication in a patient with a true posterior communicating artery aneurysm: case report and review of the literature. Neurosurgery 27(4):650–653, 1990.
Kwon, O.-K., S. H. Kim, B. J. Kwon, H.-S. Kang, J. H. Kim, C. W. Oh, and M. H. Han. Endovascular treatment of wide-necked aneurysms by using two microcatheters: techniques and outcomes in 25 patients. Am. J. Neuroradiol. 26(4):894–900, 2005.
Lee, J. W., K. C. Lee, Y. B. Kim, and S. K. Huh. Surgery for distal anterior cerebral artery aneurysms. Surg. Neurol. 70(2):153–159, 2008.
Li, L., W. Y. Huo, S. De Bao, H. Goto, and K. Watanabe. Intracranial aneurysms and ischemic cerebrovascular diseases. Int. Congr. Ser. 1259:335–338, 2004.
Liang, F., K. Fukasaku, H. Liu, and S. Takagi. A computational model study of the influence of the anatomy of the circle of Willis on cerebral hyperperfusion following carotid artery surgery. Biomed. Eng. Online 10:84, 2011.
Lippert, H., and R. Pabst. Arterial Variations in Man: Classification and Frequency. Munich: JF Bergmann-Verlag Gmbh, KG, pp. 3–10, 1985.
Maas, S. J., and J. E. Safdieh. Ischemic stroke: pathophysiology and principles of localization. Hosp. Physician Neurol. Board Rev. Manual. 13(2):1–17, 2009.
Macchi, C., R. M. Lova, B. Miniati, M. Gulisano, C. Pratesi, A. A. Conti, and G. F. Gensini. The circle of Willis in healthy older persons. J. Cardiovasc. Surg. 43(6):887–890, 2002.
Macchi, C., R. Molino Lova, B. Miniati, M. Gulisano, C. Pratesi, A. A. Conti, and G. F. Gensini. Relationship between the calibre of carotid arteries and the configuration of the circle of Willis in healthy older persons. J. Cardiovasc. Surg. 44(2):231–236, 2003.
Monson, K. L., W. Goldsmith, N. M. Barbaro, and G. T. Manley. Significance of source and size in the mechanical response of human cerebral blood vessels. J. Biomech. 38(4):737–744, 2005.
Moore, S., T. David, J. G. Chase, J. Arnold, and J. Fink. 3D models of blood flow in the cerebral vasculature. J. Biomech. 39(8):1454–1463, 2006.
Mulder, G., C. B. Bogaerds, P. Rongen, and F. N. van de Vosse. The influence of contrast agent injection on physiological flow in the circle of Willis. Med. Eng. Phys. 33(2):195–203, 2011.
Sforza, D. M., M. Putman, and J. R. Cebral. Hemodynamics of cerebral aneurysms. Annu. Rev. Fluid Mech. 41:91–107, 2009.
Songsaeng, D., S. Geibprasert, R. Willinsky, M. Tymianski, K. G. TerBrugge, and T. Krings. Impact of anatomical variations of the circle of Willis on the incidence of aneurysms and their recurrence rate following endovascular treatment. Clin. Radiol. 65(11):895–901, 2010.
Spetzler, R. F., M. N. Hadley, D. Rigamonti, L. P. Carter, P. A. Raudzens, S. A. Shedd, and E. Wilkinson. Aneurysms of the basilar artery treated with circulatory arrest, hypothermia, and barbiturate cerebral protection. J. Neurosurg. 68(6):868–879, 1988.
Stehbens, W. E. Etiology of intracranial berry aneurysms. J. Neurosurg. 70(6):823–831, 1989.
Stehbens, W. E. Evaluation of aneurysm models, particularly of the aorta and cerebral arteries. Exp. Mol. Pathol. 67(1):1–14, 1999.
Steinman, D. A., Y. Hoi, P. Fahy, L. Morris, et al. Variability of computational fluid dynamics solutions for pressure and flow in a giant aneurysm: the ASME 2012 summer bioengineering conference CDF challenge. J. Biomech. Eng. 135(2):021016, 2013.
Suzuki, J., R. Kwak, and Y. Okudaira. The safe time limit of temporary clamping of cerebral arteries in the direct surgical treatment of intracranial aneurysm under moderate hypothermia. Tohoku J. Exp. Med. 127(1):1–7, 1979.
Suzuki, O., S. Miyachi, M. Negoro, T. Okamoto, Y. Sahara, K. Hattori, N. Kobayashi, T. Kojima, and J. Yoshida. Treatment strategy for aneurysms of the posterior cerebral artery. Interv. Neuroradiol. 9(1):83–88, 2003.
Tanaka, H., N. Fujita, T. Enoki, et al. Relationship between variations in the circle of Willis and flow rates in internal carotid and basilar arteries determined by means of magnetic resonance imaging with semiautomated lumen segmentation: reference data from 125 healthy volunteers. Am. J. Neuroradiol. 27:1770–1775, 2006.
Tateshima, S., J. Grinstead, S. Sinha, et al. Intraaneurysmal flow visualization by using phase-contrast magnetic resonance imaging: feasibility study based on a geometrically realistic in vitro aneurysm model. J. Neurosurg. 100(6):1041–1048, 2004.
Ujiie, H., D. W. Liepsch, M. Goetz, R. Yamaguchi, H. Yonetani, and K. Takakura. Hemodynamic study of the anterior communicating artery. Stroke 27(11):2086–2093, 1996.
Urbanski, P. P., A. Lenos, J. C. Blume, V. Ziegler, B. Griewing, R. Schmitt, A. Diegeler, and M. Dinkel. Does anatomical completeness of the circle of Willis correlate with sufficient cross-perfusion during unilateral cerebral perfusion? Eur. J. Cardiothorac. Surg. 33(3):402–408, 2008.
Vega, C., J. V. Kwoon, and S. D. Lavine. Intracranial aneurysms: current evidence and clinical practice. Am. Fam. Physician 66(4):601–608, 2002.
Weir, B., J. Miller, and D. Russell. Intracranial aneurysms: a clinical, angiographic and computerized tomographic study. Can. J. Neurol. Sci. 4(2):99–105, 1977.
Conflict of interest
We have no conflict of interest issues.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Peter E. McHugh oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Fahy, P., McCarthy, P., Sultan, S. et al. An Experimental Investigation of the Hemodynamic Variations Due to Aplastic Vessels Within Three-Dimensional Phantom Models of the Circle of Willis. Ann Biomed Eng 42, 123–138 (2014). https://doi.org/10.1007/s10439-013-0905-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-013-0905-4