Abstract
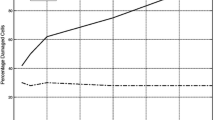
Deep tissue injury (DTI) is a severe pressure ulcer, which initiates in muscle tissue under a bony prominence, and progresses outwards. It is associated with mechanical pressure and shear that may cause capillaries to collapse and thus, induce ischemic conditions. Recently, some investigators stipulated that ischemia alone cannot explain the etiology of DTI, and other mechanisms, particularly excessive cellular deformations may be involved. The goal of this study was to evaluate the functioning of capillaries in loaded muscle tissue, using animal and finite element (FE) models. Pressures of 12, 37, and 78 kPa were applied directly to one gracilis muscle of 11 rats for 2 h. Temperatures of the loaded and contralateral muscles were recorded with time using infrared thermography (IRT) as a measure of the ischemic level. In addition, a non-linear large deformation muscle-fascicle-level FE model was developed and subjected to pressures of 12–120 kPa without and with simultaneous shear strain of up to 8%. For each simulation case, the accumulative percentage of open capillary cross-sectional area and the number of completely closed capillaries were determined. After 2 h, temperature of the loaded muscles was 2.4 ± 0.3 °C (mean ± standard deviation) lower than that of the unloaded contralateral limbs (mean of plateau temperature values across all pressure groups). Temperature of the loaded muscles dropped within 10 min but then remained stable and significantly higher than room temperature for at least 30 additional minutes in all pressure groups, indicating that limbs were not completely ischemic within the first 40 min of the trials. Our FE model showed that in response to pressures of 12–120 kPa and no shear, the accumulative percentage of open capillary cross-sectional area decreased by up to 71%. When shear strains were added, the open capillary cross-sectional area decreased more rapidly, but even for maximal loading, only 46% of the capillaries were completely closed. Taken together, the animal and FE model results suggest that acute ischemia does not develop in skeletal muscles under physiological load levels within a timeframe of 40 min. Since there is evidence that DTI develops within a shorter time, ischemia is unlikely to be the only factor causing DTI.











Similar content being viewed by others
References
Adachi H., L. C. Becker, G. Ambrosio, K. Takeda, A. F. Dipaula, W. A. Baumgartner, A. M. Borkon, B. A. Reitz. Assessment of myocardial blood flow by real-time infrared imaging. J. Surg. Res. 43:94–102, 1987
Agam, L., and A. Gefen. Pressure ulcers and deep tissue injury: a biomechanical perspective. J. Wound Care, accepted for publication, 2007
Bennett L., B. Y. Lee. Pressure versus shear in pressure causation. In: Chronic Ulcers of the Skin, edited by B. Y. Lee. New York: McGraw-Hill, 1985, pp. 39–56
Bilston L. E. The effect of perfusion on soft tissue mechanical properties: a computational model Comput. Methods Biomech. Biomed. Eng. 5:283–290, 2002
Black, J., M. Baharestani, J. Cuddigan, B. Dorner, L. Edsberg, D. Langemo, M. E. Posthauer, C. Ratliff, and G. Taler. National pressure ulcer advisory panel. National pressure ulcer advisory panel’s updated pressure ulcer staging system. Urol. Nurs. 27:144–150, 156, 2007
Bouten C. V., C. W. Oomens, F. P. Baaijens, D. L. Bader. The etiology of pressure ulcers: skin deep or muscle bound? Arch. Phys. Med. Rehabil. 84:616–619, 2003
Breuls R. G., C. V. Bouten, C. W. Oomens, D. Bader, F. P. Baaijens. A theoretical analysis of damage evolution in skeletal muscle tissue with reference to pressure ulcer development. J. Biomech. Eng. 125:902–909, 2003
Defloor T. The risk of pressure sores: a conceptual scheme J. Clin. Nurs. 8:206–216, 1999
Doughty D., J. Ramundo, P. Bonham, J. Beitz, P. Erwin-Toth, R. Anderson, B. S. Rolstad. Issues and challenges in staging of pressure ulcers. J. Wound Ostomy Continence Nurs. 33:125–130, 2006
Fan C. L., P. J. Gao, Y. J. Gu, X. F. Tang, J. J. Liu, J. Wei, K. Inoue, D. L. Zhu. Therapeutic angiogenesis by intramuscular injection of fibrin particles into ischaemic hindlimbs Clin. Exp. Pharmacol. Physiol. 33:617–622, 2006
Farid, K. J. Applying observations from forensic science to understanding the development of pressure ulcers. Ostomy Wound Manage. 53:26–28, 30, 32 passim, 2007
Gawlitta D., W. Li, C. W. Oomens, F. P. Baaijens, D. L. Bader, C. V. Bouten. The relative contributions of compression and hypoxia to development of muscle tissue damage: an in vitro study. Ann. Biomed. Eng. 35:273–284, 2007
Gefen, A. The biomechanics of sitting-acquired pressure ulcers in patients with spinal cord injury or lesions. Int. Wound J., (in press), 2007a
Gefen, A. Bioengineering models of deep tissue injury. Adv. Skin Wound Care, accepted for publication, 2007b
Gefen A. Risk factors for a pressure-related deep tissue injury: a theoretical model. Med. Biol. Eng. Comp. 45: 563–573, 2007c
Gefen A., N. Gefen, E. Linder-Ganz, S. Margulies. In vivo muscle stiffening under bone compression promotes deep pressure sores. J. Biomech. Eng. 127:512–524, 2005
Herrman E. C., C. F. Knapp, J. C. Donofrio, R. Salcido. Skin perfusion responses to surface pressure-induced ischemia: implication for the developing pressure ulcer J. Rehabil. Res. Dev. 36:109–120, 1999
Knight S., R. Taylor, A. Polliack, D. Bader. Establishing predictive indicators for the status of loaded soft tissues J. Appl. Physiol. 90:2231–2237, 2001
Kosiak M. Etiology and pathology of ischemic ulcers. Arch. Phys. Med. Rehabil. 40:62–69, 1959
Landis E. Micro-injection studies of capillary blood pressure in human skin. Heart 15:209–228, 1930
Linder-Ganz E., S. Engelberg, M. Scheinowitz, A. Gefen. Pressure-time cell death threshold for albino rat skeletal muscles as related to pressure sore biomechanics. J. Biomech. 39:2725–2732, 2006
Linder-Ganz E., A. Gefen. Mechanical compression-induced pressure sores in rat hindlimb: muscle stiffness, histology, and computational models. J. Appl. Physiol. 96:2034–2049, 2004
Linder-Ganz, E., N. Shabshin, Y. Itzchak, I. Siev-Ner, and A. Gefen. Peak gluteal muscle strain and stress values during sitting are greater in paraplegics than in normals. Summer Bioengineering Conference, Keystone Resort & Conference Center, Keystone, CO., USA, June 20–24, 2007
Linder-Ganz E., N. Shabshin, Y. Itzchak, A. Gefen. Assessment of mechanical conditions in sub-dermal tissues during sitting: a combined experimental-MRI and finite element approach. J. Biomech. 40:1443–1454, 2007
Lozano D. D., E. A. Kahl, H. P. Wong, L. L. Stephenson, W. A. Zamboni. L-Selectin and Leukocyte function in skeletal muscle reperfusion injury. Arch. Surg. 134:1079–1081, 1999
Nixon J., G. Cranny, S. Bond. Pathology, diagnosis, and classification of pressure ulcers: comparing clinical and imaging techniques Wound Repair Regen. 13:365–372, 2005
Ogden R. Elements of the theory of finite elasticity. In: Nonlinear elasticity: Theory and applications (London Mathematical Society Lecture Note Series 283), edited by Fu Y., R. Ogden. Cambridge: Cambridge University Press, United Kingdom, 2001, p. 20
Okada Y., T. Kawamata, A. Kawashima, T. Hori. Intraoperative application of thermography in extracranial–intracranial bypass surgery Neurosurgery 60:362–365, 2007
Peeters E. A., C. V. Bouten, C. W. Oomens, F. P. Baaijens. Monitoring the biomechanical response of individual cells under compression: a new compression device. Med. Biol. Eng. Comput. 41:498–503, 2003
Reichel S. M. Shearing force as a factor in decubitus ulcers in paraplegics J. Am. Med. Assoc. 166:762–763, 1958
Rowland, J. Pressure ulcers. A literature review and a treatment scheme. Aust. Fam. Phys. 22:1819, 1822–1827, 1993
Salcido R., S. B. Fisher, J. C. Donofrio, M. Bieschke, C. Knapp, R. Liang, E. K. LeGrand, J. M. Carney. An animal model and computer-controlled surface pressure delivery system for the production of pressure ulcers. J. Rehabil. Res. Dev. 32:149–161, 1995
Stekelenburg A., G. J. Strijkers, H. Parusel, D. L. Bader, K. Nicolay, C. W. Oomens. Role of ischemia and deformation in the onset of compression-induced deep tissue injury: MRI-based studies in a rat model J. Appl. Physiol. 102:2002–2011, 2007
Sugano M., K. Tsuchida, N. Makino. Intramuscular gene transfer of soluble tumor necrosis factor-alpha receptor 1 activates vascular endothelial growth factor receptor and accelerates angiogenesis in a rat model of hindlimb ischemia Circulation 109:797–802, 2004
Thomlinson R. H., L. H. Gray. The histological structure of some human lung cancers and the possible implications for radiotherapy. Brit. J. Cancer 9:539–549, 1955
Vankan W. J., J. M. Huyghe, J. D. Janssen, A. Huson. A 3-D finite element model of blood perfused rat gastrocnemius medialis muscle. Eur. J. Morphol. 34:19–24, 1996
van Donkelaar C. C., J. M. Huyghe, W. J. Vankan, M. R. Drost. Spatial interaction between tissue pressure and skeletal muscle perfusion during contraction. J. Biomech. 34:631–637, 2001
Watson J. C., A. M. Gorbach, R. M. Pluta, R. Rak, J. D. Heiss, E. H. Oldfield. Real-time detection of vascular occlusion and reperfusion of the brain during surgery by using infrared imaging. J. Neurosurg. 96:918–923, 2002
Acknowledgments
We appreciate the help of Mr. T. Berger from Infrared Technologies Co., Israel, in conducting the IRT studies. We also thank Dr. S. Engelberg from the Laboratory for Vascular Biology, Sheba Medical Center, Israel, for conducting and interpreting the muscle histology studies. Funding was provided by the Slezak Super Center for Cardiac Research and Biomedical Engineering (AG).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Linder-Ganz, E., Gefen, A. The Effects of Pressure and Shear on Capillary Closure in the Microstructure of Skeletal Muscles. Ann Biomed Eng 35, 2095–2107 (2007). https://doi.org/10.1007/s10439-007-9384-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-007-9384-9