Abstract
In India, 5 to 18 % of females attending infertility clinics are diagnosed to be suffering from genital tuberculosis. The present study was conducted to find out the prevalence of endometrial tuberculosis in infertility and its correlation with hysteroscopic changes. Patients attending infertility clinic with history of more than 2 years of unexplained infertility, failure to conceive in spite of successful ovulation induction in anovulatory infertility, and secondary infertility with a history of unexplained abortion or ectopic pregnancy were included in the study. In all the 105 cases, hysteroscopy was done, and the endometrium was subjected to DNA-PCR (polymerase chain reaction) testing for detection of Mycobacterium tuberculosis infection. Hysteroscopy features were compared in tuberculosis positive (39 %) and negative (61 %) cases for correlation. Tuberculosis was detected in 43.75 % of ostial and periostial fibrosis, 48.48 % of intrauterine fibrosis, and 66.67 % of the irregular cavity surface. A complete 6-month course of antitubercular treatment was given to the tuberculosis positive cases among which 39 % conceived without any additional treatment. The pregnancy rate of 64.7 % in secondary infertility and 20.8 % in primary infertility was very much promising. Tuberculosis is one of the major etiological factors in female infertility in developing countries. Preliminary assessment by hysteroscopy followed by PCR testing for Mycobacterium tuberculosis will detect it early. Subsequent antitubercular treatment may reverse the reproductive capability and prevent permanent damage to the female reproductive organs.
Similar content being viewed by others
Introduction
Genital tuberculosis (TB) in females is by no means uncommon, particularly in communities where pulmonary or other forms of extragenital TB are common. TB can affect any organ in the body, can exist without any clinical manifestation, and can recur. Female genital TB is typically understood as a disease of young women, with 80 to 90 % of cases diagnosed in patients 20 to 40 years old, often during workup for infertility [1]. Genital tuberculosis in females is found in 0.75 to 1 % of gynecological admissions in India, with considerable variation from place to place [2]. The disease is responsible for 5 % of all female pelvic infections and occurs in 10 % of cases of pulmonary tuberculosis [3]. It is estimated that a third of the world’s population is infected with tuberculosis and that a new infection occurs every second [4]. Most of these infections are asymptomatic and may not cause disease. However, TB remains a major health problem in many developing countries, and in these areas, genital TB is responsible for a significant proportion of female infertility [5].
It is often a secondary complication as a result of the reactivation of a silent bacillemia, primarily from the lungs, affecting most commonly the fallopian tubes (92–100 %), endometrium (50 %), ovaries (10–30 %), cervix (5 %), and the vagina and vulva (<1 %) [2, 6] but in some instances also from the kidney and intestines, etc. [7]. However, a few reports have found the endometrium to be the most commonly involved site [8, 9]. Direct inoculation of Mycobacterium can also take place over the vulva or vagina during sexual intercourse with a partner suffering from tuberculosis of the genitalia [10]. Establishment of the true incidence and prevalence of female genital tuberculosis is difficult because asymptomatic latent cases predominate over symptomatic ones [11].
This silent invader of the genital tract tends to create diagnostic dilemmas because of varied clinical presentations and diverse findings on imaging and endoscopy. Although the histopathologic evidence of mycobacterial infection is highly indicative of genital TB, its absence fails to exclude the infection. Identical lesions may also be seen in fungal and sarcoid diseases [12]. Similarly, culture methods, which have been considered a gold standard in proving genital TB, fail to exclude the infection. Furthermore, Mycobacterium is a temperamental bacillus that needs 4–5 weeks to grow on Lowenstein-Jensen (LJ) media and 2 weeks time to grow on radiometric BACTEC media [13]. The minimum Mycobacterium concentration at which histopathologic evidence appears is 10,000 bacilli/ml. For positive cultures, the required concentrations are 1,000 bacilli/ml for LJ and 10–100 bacilli/ml for BACTEC media. But by utilizing DNA-PCR (polymerase chain reaction) technique with high sensitivity of 96.4 % and specificity of 100 %, tuberculosis can be detected in the concentration as low as 10 bacilli/ml [14].
Therefore, the present study was conducted to identify the tubercular infection of the endometrium by TB-PCR analysis and correlate it with hysteroscopy features and posttreatment outcomes.
Materials and methods
This prospective study was conducted in Vishakha Steel General Hospital between November 2008 and December 2011.
Inclusion criteria
The couples presenting to the outpatient department for treatment of infertility meeting the following criteria were included in the study:
-
1)
Couples with more than 2 years of unexplained infertility where all investigations were within normal limits.
-
2)
Couples with diagnosed anovulatory infertility who failed to conceive even after 6 cycles of successful ovulation induction.
-
3)
Couples with secondary infertility following a history of unexplained abortion or ectopic pregnancy.
-
4)
Primary or secondary infertility with hypomenorrhea of the female partner (scanty flow defined by menstrual loss of 2 days or less).
Exclusion criteria
Couples with severe male factor or bilateral tubal damage were excluded from the study.
In all the cases, a detailed history was taken followed by clinical examination and basic hematological investigations. Specialized infertility investigations like hormonal assay, thyroid profile, follicular study, tubal factor assessment, including laparoscopy were performed wherever indicated before including in the study. Hysteroscopy with simultaneous TB-PCR testing of the endometrium was done for all the cases who qualified as per the inclusion criteria.
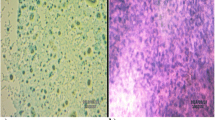
During diagnostic hysteroscopy, normal saline was used as the distension medium. A continuous flow double sheath hysteroscope was used to visualize the uterine cavity. The uterine wall and fundus were looked at for fibrosis, adhesion bands, ridges, and synechiae, indicating intrauterine fibrosis (Figs. 1, 2, 3, 4, and 5). Internal tubal ostia were checked for stenosis, a pinhole opening, blocks, and periostial fibrosis (Fig. 6). The surface of the uterine cavity was examined for irregularity (Fig. 7) or any other abnormality (Fig. 8). After the completion of hysteroscopy, a sample from the endometrium was collected by sharp curettage and stored in normal saline for TB-PCR testing.
Mycobacterium DNA was extracted from endometrial tissue using Qiagen DNA Mini Kit. DNA binds specifically to the silica-gel membrane while contaminants pass through. PCR inhibitors such as divalent cations and proteins are completely removed in two efficient wash steps, leaving purified DNA. The protocol mentioned by the manufacturer was exactly followed to obtain a final elute of 200 μl which was then subjected to real time PCR.
Oligonucleotides-designated Sp1 (5_-ACCTCCTTTCTAAGGAGCACC-3_) and Sp2 (5_-GATGCTCG CAACCACTATCCA-3_) were used to amplify an approximately 220-bp fragment of the ITS (16S-23S rDNA internal transcribed spacer) sequence (European Bioinformatics Institute accession number L15623) from Mycobacterium. Amplified product was detected by using modified specific fluorescent probes. In order to specifically identify mycobacterium tuberculosis (MTB), paired fluorogenic hybridization probes were designed to recognize a region in the ITS fragment [15].
For each sample, 10 μl of template DNA was incorporated into a 50-μl PCR containing the amplification oligonucleotides and MTB-ITS hybridization probes using the QuantiTect Probe kit (Qiagen). The optimized PCR protocol included an initial denaturation step at 95 °C for 30 s and was followed by a three-step PCR cycle 95 °C for 30 s, 59 °C for 5 s, and 72 °C for 30 s for 40 cycles. Fluorescence measurements are made in every cycle. The threshold cycle (Ct) value is the cycle at which there is a significant increase in fluorescence, and this value is associated with an exponential growth of PCR product during the log-linear phase. Positive and negative controls were used in each run. A melt curve analysis performed on the Rotor-Gene 3000 confirmed the presence of ITS fragment amplification specific to mycobacterium tuberculosis complex (MTC) in all specimens.
The hysteroscopy findings were analyzed and correlated with TB-PCR results. Those cases were found to be positive for TB-PCR were given a 6-month course of antitubercular treatment (ATT). The ATT consists of a four-drug regimen, i.e., rifampicin, isoniazid, ethambutol, and pyrazinamide for 2 months, followed by rifampicin and isoniazid for 4 months. Liver function test (LFT) was performed before starting ATT and repeated every month. Those showing common adverse effects like nausea and vomiting were managed with domperidone and ranitidine. Complaints of neuropathic symptoms were managed by a pyridoxine supplement.
Results
In this study, a total number of 105 patients with complaints of infertility, meeting the inclusion criteria, were analyzed for the correlation of TB-PCR results with hysteroscopy findings. The treatment outcomes in terms of pregnancy rates were also analyzed. Majority (38 %) of cases presented between 26 and 30 years of age followed by the age group of 20 to 25 years (35 %) (Table 1). Fifty-eight percent of the cases had primary infertility, and 42 % had secondary infertility. In 39 % of cases, the presence of Mycobacterium tuberculosis was detected in the endometrial tissue (TB-PCR positive) (Table 2).
Analyzing the hysteroscopy findings, it was found that among patients showing ostial and periostial fibrotic changes, there was 43.75 % of positive TB-PCR cases. Intrauterine fibrosis was associated with positive TB-PCR in 48.48 % of cases. Patients having irregular cavity wall was found to have 66.67 % of positive TB-PCR rate. At last, there was a single case of spotted endometrium and the same was positive for TB-PCR (Table 3).
Out of all TB PCR positive cases, 39 % conceived with antitubercular treatment only without any surgical intervention (Table 2). A successful conception rate of 64.7 % was noted in secondary infertility whereas it was 20.8 % in primary infertility (Table 2).
The most common side effects of ATT were nausea and vomiting which was managed with domperidone and ranitidine. Neuralgia and tingling sensation were complained by very few patients and were managed successfully by 100 mg of pyridoxine supplementation per day. Abnormal liver function test with icterus and high values of liver enzymes leading to abandonment of treatment was observed in two patients during the initial 2 months of treatment and were hence excluded from the study.
Discussion
Female genital tuberculosis is a rare disease in developed countries but is a frequent cause of chronic pelvic inflammatory disease and infertility in underdeveloped and developing countries. Various studies show genital TB as a cause of infertility in 1–18 % of the cases, around 1 % in the developed countries and 18 % in India [1, 5].
Generally, Mycobacterium gains access through respiratory passage in lungs and then disseminates to different organs via the lymphatic drainage and blood circulation. The female genital tract is also an important site in this dissemination process. Once the immunity to M. tuberculosis contains and overrides the growth of small number of disseminated TB bacilli after primary infection, the infection may remain silent throughout life until lowered immunity or overwhelming reinfection precipitates the disease [16]. Increased circulation and hormone dependence of the female genital organs after sexual maturity may in part explain why the genital system is vulnerable to this infection after puberty [17]. The tuberculous process generally is localized to the endometrium, being most extensive in the fundus and decreases toward the cervix. The myometrium is not usually involved. In premenopausal patients, much of the infected tissue is shed during the menstruation, only to have the endometrium reinfected from the tubes with each cycle.
In genital TB, there is a high incidence of involvement of the endometrium. Schaefer reported an incidence of 50–60 % [1], Onuigbo, an incidence of 60 % [18], and Nogales-Ortiz and colleagues, an incidence of 79 % [8], whereas Sutherland estimated 90 % involvement of the endometrium in genital TB [9].
In endometrial tuberculosis, infertility is due to functionally altered endometrium or associated tuberculous salpingitis [19]. Tubercular infection greatly suppresses the sensitivity of the endometrium to ovarian hormones leading to deficient secretory phase and defective secretion of glycogen [20]. This results in defective implantation of an ovum, leading to infertility [21]. Therefore, if the infection could be diagnosed and treated early enough before permanent damage to the genital organs ensues, it may be possible to regain the reproductive capability.
Traditionally, the laboratory diagnosis of TB depends on demonstration of the causative organism, by acid-fast staining and/or growth of the organism on Lowenstein-Jensen (LJ) medium. The diagnosis of tubercular involvement of the endometrium is difficult because it is a paucibacillary infection, and infected endometrium is shed off during menstruation. Culture methods fail to exclude the infection, and it needs 4–5 weeks to show growth on LJ media and 2 weeks time on radiometric BACTEC media. The minimum Mycobacterium concentration at which histopathological evidence appears is 10,000 bacilli/ml. For positive culture, the required concentrations are 1,000 bacilli/ml for LJ and 10–100 bacilli/ml for BACTEC media [14]. Therefore, a more sensitive method is required for the early diagnosis of endometrial tuberculosis specifically in latent cases.
During the 1990s, nucleic acid amplification (NAA) techniques evolved and dramatically altered the way in which we can detect and identify M. tuberculosis. NAA technique is a PCR-based test that amplifies M. tuberculosis DNA for the detection of M. tuberculosis from samples containing as low as 10 bacilli/ml [14]. Due to this reason, DNA-PCR techniques were utilized to identify M. tuberculosis directly from the clinical specimens, and the results were available in a day or two with high sensitivity (96.4 %) and high specificity (100 %) [22].
In our study, we tried to correlate the hysteroscopic changes to the presence of Mycobacterium in the endometrial tissue in cases of infertility where there were no other obvious causes detected. As we can understand that the major physical changes to the endometrium takes a long time to appear because of the repeated shedding, we have concentrated on the subtle as well as gross hysteroscopic changes that may suggest any low-grade inflammation. Therefore, minimal changes like pinhole ostium, periostial fibrosis and gross changes like fundal fibrosis, intrauterine fibrotic bands, and blocked ostia were all taken into consideration for assessing the possible involvement of the endometrium.
Because of targeting a very selective group of population and including subtle changes as abnormal, we found only 2.86 % of normal-looking endometrium. In our study, ostial and periostial fibrosis was associated with positive TB-PCR in 43.75 % and intrauterine fibrosis was associated with positive TB-PCR in 48.48 % of cases. This finding strongly suggests looking for the presence of M. tuberculosis in such types of hysteroscopic pictures in infertility. Although irregular cavity surface and spotted endometrium were associated with 66.67 and 100 % of positive TB-PCR, respectively, the number of patients was too minimal to derive any conclusion (Table 2). Baxi et al. reported 44.44 % positive TB-PCR in ostial fibrosis and 50 % positive TB-PCR in intrauterine fibrosis [23]. These reports were comparable to our study (p = 0.47). The overall incidence of 32.18 % reported by Baxi et al. is also in close agreement with our report of 39 % (Table 4).
Out of all TB-PCR positive cases in our study, 39 % conceived with antitubercular treatment only, which is very a encouraging result. There was a drastic difference in conception rate between primary and secondary infertility. The conception rate of 64.7 % in secondary infertility as against 20.8 % of that in primary infertility (p = 0.002) indicates a higher singular contributory role of tuberculosis toward infertility in the first group (Table 2). The lower pregnancy rate in primary infertility may indicate additional contributing factors apart from this acquired disease. Hence, subsequent IVF could be an ideal option for those who could not conceive after ATT.
Conclusion
Genital tuberculosis leading to tuberculous endometritis is one of the most intractable causes of infertility. Early diagnosis in the latent phase is possible by detecting the subtle hysteroscopic changes, supplemented by TB-PCR testing. A subsequent complete course of ATT may prevent the development of overt genital tuberculosis and reverse the reproductive capability. The results are very encouraging and more apparent in secondary than in primary infertility. Therefore, a large-scale study is recommended to establish the exact role of latent endometrial tuberculosis in infertility in developing countries where tuberculosis is endemic.
References
Schaefer G (1976) Female genital tuberculosis. Clin Obstet Gynecol 19:223
Varma TR (1991) Genital tuberculosis and subsequent fertility. Int J Gynaecol Obstet 35:1–11
Dawn CS (1998) Pelvic infections. In: Dawn CS 9th ed. Textbook of gynaecology and contraception: 9th ed. Calcutta: Arati Dawn p 321
Bartlett JG (2007) Tuberculosis and HIV infection: partners in human tragedy. J Inf Dis 196:S124–S125
Muir DG, Belsey MA (1980) Pelvic inflammatory disease and its consequences in the developing world. Am J Obstet Gynecol 138:913–928
Arora VK, Johri A, Arora R et al (1994) Tuberculosis of the vagina in a HIV seropositive case. Tuber Lung Dis 75:239–240
Simon HB, Weinstein AJ, Pasternak MS et al (1977) Genitourinary tuberculosis: clinical features in a general hospital population. Am J Med 63:410–420
Nogales-Ortiz F, Tarancion I, Nogales FF Jr (1979) The pathology of female genital tuberculosis: a 31-year study of 1436 cases. Obstet Gynecol 53:422
Sutherland AM (1960) Genital tuberculosis in women. Am J Obstet Gynecol 79:486
Richards MJ, Angus D (1998) Possible sexual transmission of genitourinary tuberculosis. Int J Tuberc Lung Dis 2:439
Rom W, Garay S (1996) Tuberculosis, 1st edn. Little Brown, New York
Krishna UR, Sheth SS, Motashaw ND (1979) Place of laparoscopy in pelvic inflammatory disease. J Obstet Gynaecol India 29(3):505–510
Katoch VM (2004) Newer diagnostic techniques for tuberculosis. Indian J Med Res 120:418–428
Bhanu NV, Singh UB, Chakraborty M et al (2005) Improved diagnostic value of PCR in the diagnosis of female genital tuberculosis leading to infertility. J Med Microbiol 54(Pt10):927–931
Kraus G, Cleary T, Miller N, Seivright R, Young AK, Spruill G, Hnatyszyn HJ (2001) Rapid and specific detection of Mycobacterium tuberculosis using fluorogenic probes and real-time PCR. Mol Cell Probes 15:375–383
Arora VK, Gupta R, Arora R (2003) Female genital tuberculosis—need for more research. Indian J Tuberc 50:9
Choudhary NN (1996) Overview of tuberculosis of the female genital tract. J Indian Med Assoc 94:345–361
Onuigbo WIB (1979) Genital tuberculosis and reproductive function. J Reprod Med 21:249
Falk V, Ludriksson K, Agnon C (1980) Genital tuberculosis in women. Am J Obstet Gynecol 138:933
Fox H, Buckely CH (1981) Histopathological study of endometrium in infertility cases. Recent advances in histopathology
Hughes EC (1945) Relationship of glycogen to problems of sterility and ovular life. Am J Obstet Gynecol 49:10–18
Rozati R, Roopa S, Naga Rajeshwari C (2006) Evaluation of women with infertility and genital tuberculosis. J Obstet Gynecol India 56:423–426
Asha B, Hansali N, Manila K, Priti S, Dhawal B (2011) J Obstet Gynecol India 61(3):301–306
Conflict of interest
Subrat Kumar Mohakul, Venkata Radha Kumari Bella, and Purnima Tiru declare that they have no conflict of interest.
Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mohakul, S.K., Beela, V.R.K. & Tiru, P. Hysteroscopy findings and its correlation with latent endometrial tuberculosis in infertility. Gynecol Surg 12, 31–39 (2015). https://doi.org/10.1007/s10397-014-0865-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-014-0865-1