Abstract
Purpose
Although cellular immunotherapy is expected as a new cancer treatment, its therapeutic efficiency is limited in solid tumors, because most cells return to the bloodstream rather than adhere to the target site. Therefore, we are motivated to develop a technique to concentrate the cells in the blood flow using active control of bubble-surrounded cells under ultrasound exposure considering both aspects of cell controllability and viability.
Methods
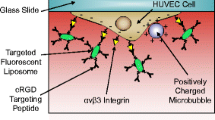
We prepared a lipid bubble conjugating ligand to adhere to the surface of the T-cells. First, we evaluated the cell controllability by retaining the cells on a wall of an artificial blood vessel through continuous ultrasound exposure. Next, we investigated the cell viability under ultrasound exposure in a suspension with various bubble concentrations.
Results
We estimated the concentration of bubbles when the adhesion to the cell surface was saturated. Then, we evaluated the cell viability with various conditions of ultrasound exposure and bubble concentrations. However, it was confirmed that cell damage occurred under conditions that achieved proper control of the cells. Therefore, we exposed the cells to burst waves to reduce the applied ultrasound intensity. Consequently, the significant increase in cell viability was confirmed to be inversely proportional to the duty ratio.
Conclusion
To retain cells on a vessel wall, determining the appropriate ultrasound condition including sound pressure and waveform is important to maintain cell viability.







Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article.
References
Cui C, Enosawa S, Matsunari H, et al. Natural flavonol, myricetin, enhances the function and survival of cryopreserved hepatocytes in vitro and in vivo. Int J Mol Sci. 2019;20:6123.
Hayes C. Cellular immunotherapies for cancer. Ir J Med Sci. 2021;19:41–57.
Riley RS, June CH, Langer R, et al. Delivery technologies for cancer immunotherapy. Nat Rev Drug Discov. 2019;18:175–96.
O’Donnell JS, Teng MWL, Smyth MJ. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat Rev Clin Oncol. 2019;16:151–67.
Aminin D, Wang YM. Macrophages as a “weapon” in anticancer cellular immunotherapy. Kaohsiung J Med Sci. 2021;37:749–58.
Diederich M. Natural compound inducers of immunogenic cell death. Arch Pharmacal Res. 2019;42:629–45.
Wang X, Huang J, Zhang A, et al. Altered expression profile of BAFF receptors on peripheral blood B lymphocytes in Graves’ disease. BMC Endocr Disord. 2021;21:88.
Stoll A, Bruns H, Fuchs M, et al. CD137 (4–1BB) stimulation leads to metabolic and functional reprogramming of human monocytes/macrophages enhancing their tumoricidal activity. Leukemia. 2021;35:3482–96.
Zhang Y, Lin S, Wang XY, et al. Nanovaccines for cancer immunotherapy. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2019;11: e1559.
Fusaroli M, Isgrò V, Cutroneo PM, et al. Post-marketing surveillance of CAR-T-cell therapies: analysis of the FDA adverse event reporting system (FAERS) database. Drug Saf. 2022. https://doi.org/10.1007/s40264-022-01194-z.
Ellard R, Kenyon M, Hutt D, et al. The EBMT immune effector cell nursing guidelines on CAR-T therapy: a framework for patient care and managing common toxicities. Clin Hematol Int. 2022;4:75–88.
Raglow Z, McKenna MK, Bonifant CL, et al. Targeting glycans for CAR therapy: the advent of sweet CARs. Mol Ther. 2022;30:2881–90.
Conejo-Garcia JR, Guevara-Patino JA. Barriers and opportunities for CAR T-Cell targeting of solid tumors. Immunol Invest. 2022. https://doi.org/10.1080/08820139.2022.2096463.
Escoffre JM, Deckers R, Bos C, et al. Bubble-assisted ultrasound: application in immunotherapy and vaccination. Adv Exp Med Biol. 2016;880:243–61.
Kokhuis T, Skachkov I, Naaijkens B, et al. Intravital microscopy of localized stem cell delivery using microbubbles and acoustic radiation force. Biotechnol Bioeng. 2015;112:220–7.
Woudstra L, Meinster E, Van Haren L, et al. StemBell therapy stabilizes atherosclerotic plaques after myocardial infarction. Cytotherapy. 2018;20:1143–54.
Emmens RW, Oedayrajsingh-Varma M, Woudstra L, et al. A comparison in therapeutic efficacy of several time points of intravenous StemBell administration in a rat model of acute myocardial infarction. Cytotherapy. 2017;19:131–40.
Demachi F, Murayama Y, Hosaka N, et al. Preliminary study on forming microbubble-surrounded cells as carriers for cellular therapy and evaluation of ultrasound controllability by fluorescence imaging. Jpn J Appl Phys. 2015;54:07HF19.
Oitate R, Shimomura A, Wada H, et al. Validation of tracking performance of cell–bubble aggregation versus variation of acoustic field. Jpn J Appl Phys. 2017;56:07JF25.
Oitate R, Otsuka T, Seki M, et al. Acoustic field sweeping for active induction of bubble-surrounded T-cells. Jpn J Appl Phys. 2018;57:07JF10.
Seki M, Otsuka T, Oitate R, et al. Viability validation of therapeutic cells according to surrounded amount of microbubbles and ultrasound exposure condition. Jpn J Appl Phys. 2019;58:SGGE13.
Chikaarashi T, Watanabe S, Miyamoto Y, et al. Experimental study of ultrasound retention of bubble-surrounded cells under various conditions of acoustic field and flow velocity. Jpn J Appl Phys. 2022;61:SG1071.
Koda R, Koido J, Hosaka N, et al. Evaluation of active control of bubble liposomes in a bifurcated flow under various ultrasound conditions. Adv Biomed Eng. 2014;3:21–8.
Masuda K, Watarai N, Nakamoto R, et al. Production of local acoustic radiation force to constrain direction of microcapsules in flow. Jpn J Appl Phys. 2010;49:07HF11.
Masuda K, Nakamoto R, Watarai N, et al. Effect of existence of red blood cell in trapping performance of microbubbles by acoustic radiation force. Jpn J Appl Phys. 2011;50:07HF11.
Hosaka N, Koda R, Onogi S, et al. Production and validation of acoustic field to enhance trapping efficiency of microbubbles by using a matrix array transducer. Jpn J Appl Phys. 2013;52:07HF14.
Masuda K, Koda R, Watarai N, et al. (2011) Experimental study of active control of microbubbles in blood flow by forming their aggregations. Proc. IEEE Ultrasonics Symp. 2021–4
Shigehara N, Demachi F, Koda R, et al. Experimental study for active path block in a multi-bifurcated flow by using microbubbles aggregation. Jpn J Appl Phys. 2013;52:07HF15.
Huang G, Zhang M, Han L, et al. Physical investigation of acoustic waves induced by the oscillation and collapse of the single bubble. Ultrason Sonochem. 2021;72: 105440.
Kim C, Choi WJ, Ng Y, et al. Mechanically induced cavitation in biological systems. Life. 2021;11:546.
Zevnik J, Dular M. Liposome destruction by a collapsing cavitation microbubble: a numerical study. Ultrason Sonochem. 2021;78: 105706.
Kudo N, Okada K, Yamamoto K. Sonoporation by single-shot pulsed ultrasound with microbubbles adjacent to cells. Biophys J. 2009;96:4866–76.
Ito Y, Saito T, Watanabe S, et al. Validation of damage on vascular endothelial cells under ultrasound exposure according to adhered situation of bubbles. Jpn J Appl Phys. 2022;61:SG1066.
Yokoe I, Omata D, Unga J, et al. Lipid bubbles combined with low-intensity ultrasound enhance the intratumoral accumulation and antitumor effect of pegylated liposomal doxorubicin in vivo. Drug Deliv. 2021;28:530–41.
Endo-Takahashi Y, Kurokawa R, Sato K, et al. Ternary complexes of pDNA, neuron-binding peptide, and PEGylated polyethyleneimine for brain delivery with nano-bubbles and ultrasound. Pharmaceutics. 2021;13:1003.
Suzuki R, Oda Y, Omata D, et al. Tumor growth suppression by the combination of nanobubbles and ultrasound. Cancer Sci. 2016;107:217–23.
Yamatoya K, Nagai Y, Teramoto N, et al. Cryopreservation of undifferentiated and differentiated human neuronal cells. Regen Ther. 2022;19:58–68.
Miyamoto Y, Ikeuchi M, Noguchi H, et al. Long-term cryopreservation of human and other mammalian cells at −80 °C for 8 Years. Cell Med. 2018;10:2155179017733148.
Zimmerman MA, Biggers CD, Li PA. Rapamycin treatment increases hippocampal cell viability in an mTOR-independent manner during exposure to hypoxia mimetic, cobalt chloride. BMC Neurosci. 2018;19:82.
Acknowledgements
This research was supported by a grant from the Japan Society for the Promotion of Science (JSPS) through KAKENHI Grant No. 20H04547, and the Uehara Memorial Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflicts of interest exist.
Ethical approval
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Kajita, N., Ito, Y., Watanabe, S. et al. Viability variation of T-cells under ultrasound exposure according to adhesion condition with bubbles. J Med Ultrasonics 50, 121–129 (2023). https://doi.org/10.1007/s10396-022-01277-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01277-5