Abstract
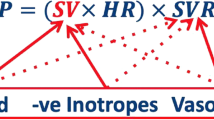
Hypertensive disorders are quite common, complicating about 10% of pregnancies, while preeclampsia occurs in 2–8% of cases. The most recognized etiopathogenetic factor for the development of preeclampsia is deficient remodeling of the spiral arteries during trophoblastic invasion. Recently, some authors speculated about the “cardiovascular origin of preeclampsia”; in particular, they postulate that placental dysfunction is not the primum movens of preeclampsia, but it could be caused by a failure of the maternal cardiovascular system to adapt to the pregnancy itself. Moreover, several studies have also shown that developing preeclampsia in pregnancy is associated with an increased risk of cardiovascular disease later in life. Due to the importance of this pathology, it would be crucial to have an effective screening in order to implement a prophylaxis; for this purpose, it could be useful to have an accurate and noninvasive device for the assessment of maternal hemodynamic variables. USCOM® (Ultrasonic Cardiac Output Monitor) is a noninvasive Doppler ultrasonic technology which combines accuracy, reproducibility, noninvasiveness, and a fast learning curve. Maternal hemodynamic evaluation is important in order to monitor the changes that the maternal organism encounters, in particular a reduction in blood pressure, a decrease in total peripheral resistances, and an increase in cardiac output, resulting in a hyperdynamic circle. These hemodynamic modifications are lacking in pregnancies complicated by preeclampsia. For these reasons, it is crucial to have a tool that allows these parameters to be easily evaluated in order to identify those women at higher risk of hypertensive complications and more severe outcomes.


Similar content being viewed by others
References
Brown MA, Magee LA, Kenny LC, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018;72:24–43.
Huppertz B. Placental origins of preeclampsia: challenging the current hypothesis. Hypertension. 2008;51:970–5.
Redman CWG, Staff AC, Roberts JM. Syncytiotrophoblast stress in preeclampsia: the convergence point for multiple pathways. Am J Obstet Gynecol. 2021;226:S907–27.
Staff AC, Fjeldstad HE, Fosheim IK, et al. Failure of physiological transformation and spiral artery atherosis: their roles in preeclampsia. Am J Obstet Gynecol. 2020;226:S895–906.
Karumanchi SA, Maynard SE, Stillman IE, et al. Preeclampsia: a renal perspective. Kidney Int. 2005;67:2101–13.
Powe CE, Levine RJ, Karumanchi SA. Preeclampsia, a disease of the maternal endothelium: the role of antiangiogenic factors and implications for later cardiovascular disease. Circulation. 2011;123:2856–69.
O’Gorman N, Nicolaides KH, Poon LC. The use of ultrasound and other markers for early detection of preeclampsia. Womens Health (Lond). 2016;12:199–207.
Kalafat E, Thilaganathan B. Cardiovascular origins of preeclampsia. Curr Opin Obstet Gynecol. 2017;29:383–9.
Melchiorre K, Giorgione V, Thilaganathan B. The placenta and preeclampsia: villain or victim? Am J Obstet Gynecol. 2021;226:S954–62.
Lovgren TR, Dugoff L, Galan HL. Uterine artery Doppler and prediction of preeclampsia. Clin Obstet Gynecol. 2010;53:888–98.
Poon LC, Nicolaides KH. First-trimester maternal factors and biomarker screening for preeclampsia. Prenat Diagn. 2014;34:618–27.
Verlohren S, Perschel FH, Thilaganathan B, et al. Angiogenic markers and cardiovascular indices in the prediction of hypertensive disorders of pregnancy. Hypertension. 2017;69:1192–7.
Melchiorre K, Wormald B, Leslie K, et al. First-trimester uterine artery Doppler indices in term and preterm pre-eclampsia. Ultrasound Obstet Gynecol. 2008;32:133–7.
Sotiriadis A, Hernandez-Andrade E, da Silva CF, et al. ISUOG Practice Guidelines: role of ultrasound in screening for and follow-up of pre-eclampsia. Ultrasound Obstet Gynecol. 2019;53:7–22.
Roberge S, Bujold E, Nicolaides KH. Aspirin for the prevention of preterm and term preeclampsia: systematic review and metaanalysis. Am J Obstet Gynecol. 2018;218:287-93.e1.
Rolnik DL, Wright D, Poon LC, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377:613–22.
Rolnik DL, Wright D, Poon LCY, et al. ASPRE trial: performance of screening for preterm pre-eclampsia. Ultrasound Obstet Gynecol. 2017;50:492–5.
McDonald SD, Malinowski A, Zhou Q, et al. Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J. 2008;156:918–30.
Sibai BM, el-Nazer A, Gonzalez-Ruiz A. Severe preeclampsia-eclampsia in young primigravid women: subsequent pregnancy outcome and remote prognosis. Am J Obstet Gynecol. 1986;155:1011–6.
Melchiorre K, Sharma R, Khalil A, et al. Maternal cardiovascular function in normal pregnancy: evidence of maladaptation to chronic volume overload. Hypertension. 2016;67:754–62.
Melchiorre K, Sharma R, Thilaganathan B. Cardiac structure and function in normal pregnancy. Curr Opin Obstet Gynecol. 2012;24:413–21.
Melchiorre K, Sharma R, Thilaganathan B. Cardiovascular implications in preeclampsia: an overview. Circulation. 2014;130:703–14.
Melchiorre K, Sutherland GR, Baltabaeva A, et al. Maternal cardiac dysfunction and remodeling in women with preeclampsia at term. Hypertension. 2011;57:85–93.
Melchiorre K, Thilaganathan B. Maternal cardiac function in preeclampsia. Curr Opin Obstet Gynecol. 2011;23:440–7.
Ghi T, Degli Esposti D, Montaguti E, et al. Post-partum evaluation of maternal cardiac function after severe preeclampsia. J Matern Fetal Neonatal Med. 2014;27:696–701.
Melchiorre K, Sutherland GR, Liberati M, et al. Preeclampsia is associated with persistent postpartum cardiovascular impairment. Hypertension. 2011;58:709–15.
Mulder E, Basit S, Oben J, et al. Accuracy and precision of USCOM versus transthoracic echocardiography before and during pregnancy. Pregnancy Hypertens. 2019;17:138–43.
Cheng YW, Xu F, Li J. Identification of volume parameters monitored with a noninvasive ultrasonic cardiac output monitor for predicting fluid responsiveness in children after congenital heart disease surgery. Medicine (Baltimore). 2018;97: e12289.
Deep A, Goonasekera CD, Wang Y, et al. Evolution of haemodynamics and outcome of fluid-refractory septic shock in children. Intensive Care Med. 2013;39:1602–9.
Hodgson LE, Venn R, Forni LG, et al. Measuring the cardiac output in acute emergency admissions: use of the non-invasive ultrasonic cardiac output monitor (USCOM) with determination of the learning curve and inter-rater reliability. J Intensive Care Soc. 2016;17:122–8.
Zheng ML, He SR, Liu YM, et al. Measurement of inotropy and systemic oxygen delivery in term, low- and very-low-birth-weight neonates using the Ultrasonic Cardiac Output Monitor (USCOM). J Perinat Med. 2020;48:289–95.
Vinayagam D, Thilaganathan B, Stirrup O, et al. Maternal hemodynamics in normal pregnancy: reference ranges and role of maternal characteristics. Ultrasound Obstet Gynecol. 2018;51:665–71.
Vasapollo B, Novelli GP, Valensise H. Total vascular resistance and left ventricular morphology as screening tools for complications in pregnancy. Hypertension. 2008;51:1020–6.
Tiralongo GM, Lo Presti D, Pisani I, et al. Assessment of total vascular resistance and total body water in normotensive women during the first trimester of pregnancy. A key for the prevention of preeclampsia. Pregnancy Hypertens. 2015;5:193–7.
Gagliardi G, Tiralongo GM, LoPresti D, et al. Screening for pre-eclampsia in the first trimester: role of maternal hemodynamics and bioimpedance in non-obese patients. Ultrasound Obstet Gynecol. 2017;50:584–8.
Montaguti E, Youssef A, Cavalera M, et al. Maternal hemodynamic assessment by USCOM(®) device in the first trimester of pregnancy. J Matern Fetal Neonatal Med. 2021. https://doi.org/10.1080/14767058.2021.1887129.
Montaguti E, Di Donna G, Pilu G. 2021 Usefulness of USCOM® evaluation in women with chronic hypertension who developed severe preeclampsia with low platelets and elevated liver enzymes. J Matern Fetal Neonatal Med. 2021. https://doi.org/10.1080/14767058.2021.1873269.
Valensise H, Farsetti D, Pisani I, et al. (2020) Hemodynamic maladaptation and left ventricular dysfunction in chronic hypertensive patients at the beginning of gestation and pregnancy complications: a case control study. J Matern Fetal Neonatal Med. 2020. https://doi.org/10.1080/14767058.2020.1818206.
Vasapollo B, Novelli GP, Gagliardi G, et al. Pregnancy complications in chronic hypertensive patients are linked to pre-pregnancy maternal cardiac function and structure. Am J Obstet Gynecol. 2020;223:425.
Di Pasquo E, Ghi T, Dall’Asta A, et al. Maternal cardiac parameters can help in differentiating the clinical profile of preeclampsia and in predicting progression from mild to severe forms. Am J Obstet Gynecol. 2019;221:633.
Ferrazzi E, Stampalija T, Monasta L, et al. Maternal hemodynamics: a method to classify hypertensive disorders of pregnancy. Am J Obstet Gynecol. 2018;218:124.
Foo FL, Mahendru AA, Masini G, et al. Association between prepregnancy cardiovascular function and subsequent preeclampsia or fetal growth restriction. Hypertension. 2018;72:442–50.
Di Pasquo E, Ghi T, Dall’Asta A, et al. Hemodynamic findings in normotensive women with small-for-gestational-age and growth-restricted fetuses. Acta Obstet Gynecol Scand. 2020;100:876–83.
Valensise H, Farsetti D, Lo Presti D, et al. Preterm delivery and elevated maternal total vascular resistance: signs of suboptimal cardiovascular adaptation to pregnancy? Ultrasound Obstet Gynecol. 2016;48:491–5.
Kalafat E, Barratt I, Nawaz A, et al. Maternal cardiovascular function and risk of intrapartum fetal compromise in women undergoing induction of labor: pilot study. Ultrasound Obstet Gynecol. 2020;56:233–9.
Valensise H, Lo Presti D, Tiralongo GM, et al. Foetal heart rate deceleration with combined spinal-epidural analgesia during labour: a maternal haemodynamic cardiac study. J Matern Fetal Neonatal Med. 2016;29:1980–6.
Valensise H, Tiralongo GM, Pisani I, et al. Maternal hemodynamics early in labor: a possible link with obstetric risk? Ultrasound Obstet Gynecol. 2018;51:509–13.
Acknowledgements
The authors report no acknowledgements.
Funding
There is no funding sources.
Author information
Authors and Affiliations
Contributions
EM devised the topic, did literature search, and drafted and wrote the paper. GDD participated in writing, literature searching, and arranging of the references. AY provided expertise and participated in writing and editing of the text. GP participated in writing and editing of the text. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical approval
Given the nature of the review article, no ethical committee approval was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Montaguti, E., Di Donna, G., Youssef, A. et al. Hypertensive disorders and maternal hemodynamic changes in pregnancy: monitoring by USCOM® device. J Med Ultrasonics 49, 405–413 (2022). https://doi.org/10.1007/s10396-022-01225-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-022-01225-3