Abstract
Purpose
By analyzing possible factors contributing to imaging misevaluation of arterial phase (AP) vascularity, we aimed to provide a more proper way to detect AP hypervascularity of hepatocellular carcinomas (HCCs) using the noninvasive imaging modalities magnetic resonance imaging (MRI) and contrast-enhanced ultrasound (CEUS).
Methods
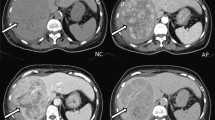
We retrospectively recruited 164 pathologically confirmed HCC lesions from 128 patients. Using CEUS with Sonazoid (SCEUS) and gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid MRI (EOB-MRI), AP vascularity of the lesions was evaluated and inconsistencies in interpretation were examined. Indicators of margin, echogenicity, and halo and mosaic signs of lesions on grayscale US; depth of lesions on SCEUS; and tumoral homogeneity, signal contrast ratio of lesions to the surrounding area on precontrast and AP images on EOB-MRI, and histological grade were investigated.
Results
When precontrast images were used to adjust the AP enhancement ratio, the proportion of inconsistent interpretations of AP vascularity declined from 26.2% (43/164; 29 non-hypervascularity instances using EOB-MRI and 14 using SCEUS) to 16.5% (27/164; 7 using EOB-MRI and 20 using SCEUS). Greater lesion depth (P = 0.017), ill-defined tumoral margin (P = 0.028), absence of halo sign (P = 0.034), and histologically early HCC (P = 0.007) on SCEUS, and small size (P = 0.012) and heterogeneity (P = 0.013) of lesions and slight enhancement (low AP enhancement ratio) (P = 0.018 and 0.009 before and after adjustment) on EOB-MRI, may relate to undetectable hypervascularity.
Conclusions
SCEUS and EOB-MRI may show discrepancies in evaluating AP vascularity in the case of deep, ill-defined, heterogeneous, slightly enhanced lesions, and histologically early HCCs. We recommend adjusting AP with precontrast images in EOB-MRI, and combining both modalities to detect hypervascularity.




Similar content being viewed by others
References
Kitao A, Zen Y, Matsui O, et al. Hepatocarcinogenesis: Multistep changes of drainage vessels at CT during arterial portography and hepatic arteriography–radiologic-pathologic correlation. Radiology. 2009;252:605–14.
Bartolotta TV, Taibbi A, Midiri M, et al. Contrast-enhanced ultrasound of hepatocellular carcinoma: where do we stand? Ultrasonography. 2019;38:200–14.
Takahashi M, Maruyama H, Shimada T, et al. Characterization of hepatic lesions (≤ 30 mm) with liver-specific contrast agents: a comparison between ultrasound and magnetic resonance imaging. Eur J Radiol. 2013;82:75–84.
Cassinotto C, Aube C, Dohan A. Diagnosis of hepatocellular carcinoma: an update on international guidelines. Diagn Interv Imaging. 2017;98:379–91.
Kim DK, An C, Chung YE, et al. Hepatobiliary versus extracellular MRI contrast agents in hepatocellular carcinoma detection: hepatobiliary phase features in relation to disease-free survival. Radiology. 2019;293:594–604.
Ishii T, Numata K, Hao Y, et al. Evaluation of hepatocellular carcinoma tumor vascularity using contrast-enhanced ultrasonography as a predictor for local recurrence following radiofrequency ablation. Eur J Radiol. 2017;89:234–41.
Mandai M, Koda M, Matono T, et al. Assessment of hepatocellular carcinoma by contrast-enhanced ultrasound with perfluorobutane microbubbles: comparison with dynamic CT. Br J Radiol. 2011;84:499–507.
Numata K, Fukuda H, Miwa H, et al. Contrast-enhanced ultrasonography findings using a perflubutane-based contrast agent in patients with early hepatocellular carcinoma. Eur J Radiol. 2014;83:95–102.
Toyota N, Nakamura Y, Hieda M, et al. Diagnostic capability of gadoxetate disodium-enhanced liver MRI for diagnosis of hepatocellular carcinoma: comparison with multi-detector CT. Hiroshima J Med Sci. 2013;62:55–61.
Sugimoto K, Moriyasu F, Shiraishi J, et al. Assessment of arterial hypervascularity of hepatocellular carcinoma: comparison of contrast-enhanced US and gadoxetate disodium-enhanced MR imaging. Eur Radiol. 2012;22:1205–13.
Burns PN, Wilson SR. Focal liver masses: Enhancement patterns on contrast-enhanced images–concordance of US scans with CT scans and MR images. Radiology. 2007;242:162–74.
Stocker D, Becker AS, Barth BK, et al. Does quantitative assessment of arterial phase hyperenhancement and washout improve LI-RADS v2018-based classification of liver lesions? Eur Radiol. 2020;30:2922–33.
Hennedige T, Yang ZJ, Ong CK, et al. Utility of non-contrast-enhanced CT for improved detection of arterial phase hyperenhancement in hepatocellular carcinoma. Abdom Imaging. 2014;39:1247–54.
Kim M, Kang TW, Cha DI, et al. Identification of arterial hyperenhancement in CT and MRI in patients with hepatocellular carcinoma: value of unenhanced images. Korean J Radiol. 2019;20:236–45.
An C, Park MS, Kim D, et al. Added value of subtraction imaging in detecting arterial enhancement in small (< 3 cm) hepatic nodules on dynamic contrast-enhanced MRI in patients at high risk of hepatocellular carcinoma. Eur Radiol. 2013;23:924–30.
Wang F, Numata K, Nihonmatsu H, et al. Application of new ultrasound techniques for focal liver lesions. J Med Ultrason. 2001;2020(47):215–37.
Lyshchik A, Kono Y, Dietrich CF, et al. Contrast-enhanced ultrasound of the liver: technical and lexicon recommendations from the ACR CEUS LI-RADS working group. Abdom Radiol (NY). 2018;43:861–79.
Ohama H, Imai Y, Nakashima O, et al. Images of Sonazoid-enhanced ultrasonography in multistep hepatocarcinogenesis: comparison with Gd-EOB-DTPA-enhanced MRI. J Gastroenterol. 2014;49:1081–93.
Wang F, Numata K, Nakano M, et al. Diagnostic value of imaging methods in the histological four grading of hepatocellular carcinoma. Diagnostics (Basel). 2020;10:321.
Wilson SR, Kim TK, Jang HJ, et al. Enhancement patterns of focal liver masses: discordance between contrast-enhanced sonography and contrast-enhanced CT and MRI. AJR Am J Roentgenol. 2007;189:W7-12.
Dietrich CF, Averkiou M, Nielsen MB, et al. How to perform contrast-enhanced ultrasound (CEUS). Ultrasound Int Open. 2018;4:E2-15.
Greis C. Technical aspects of contrast-enhanced ultrasound (CEUS) examinations: tips and tricks. Clin Hemorheol Microcirc. 2014;58:89–95.
Nihonmatsu H, Numata K, Fukuda H, et al. Low mechanical index contrast mode versus high mechanical index contrast mode: Which is a more sensitive method for detecting Sonazoid microbubbles in the liver of normal subjects? J Med Ultrason. 2001;2016(43):211–7.
Dong Y, Wang WP, Mao F, et al. Application of imaging fusion combining contrast-enhanced ultrasound and magnetic resonance imaging in detection of hepatic cellular carcinomas undetectable by conventional ultrasound. J Gastroenterol Hepatol. 2016;31:822–8.
Kagawa Y, Okada M, Kumano S, et al. Optimal scanning protocol of arterial dominant phase for hypervascular hepatocellular carcinoma with gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced MR. J Magn Reson Imaging. 2011;33:864–72.
Ramalho M, Matos AP, AlObaidy M, et al. Magnetic resonance imaging of the cirrhotic liver: diagnosis of hepatocellular carcinoma and evaluation of response to treatment—part 1. Radiol Bras. 2017;50:38–47.
Kondo F. Histological features of early hepatocellular carcinomas and their developmental process: for daily practical clinical application : hepatocellular carcinoma. Hepatol Int. 2009;3:283–93.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. The requirement for informed consent was waived in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Wang, F., Numata, K., Chuma, M. et al. A study on the inconsistency of arterial phase hypervascularity detection between contrast-enhanced ultrasound using sonazoid and gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid magnetic resonance imaging of hepatocellular carcinoma lesions. J Med Ultrasonics 48, 215–224 (2021). https://doi.org/10.1007/s10396-021-01086-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01086-2