Abstract
Purpose
Animal studies of endoscopic ultrasound-guided radiofrequency ablation (EUS-RFA) of the liver have rarely been reported. We assessed the effectiveness and safety of EUS-RFA in pigs.
Methods
We conducted four experiments using newly designed RFA electrodes. In the first experiment, we ablated excised liver using 19 G electrodes with active electrode tips with lengths of 1, 1.5, and 2 cm. The second experiment was performed with the same electrodes as those used in the first experiment, but with the electrodes inserted into the livers of live pigs under EUS. In the third experiment, we tested the electrodes for water permeability. In the fourth experiment, we performed EUS-RFA on live pigs, using 19 G electrodes in 7/12 pigs and 18 G electrodes in 5/12 pigs. Complications were evaluated after 7 days of survival.
Results
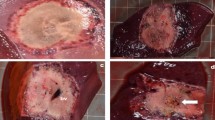
The newly designed RFA electrodes achieved ablation of the liver. In the first experiment, the maximal sizes of the ablation areas were 27, 26, 24, and 25 mm at 10, 20, 30, and 40 W, respectively, with the 2-cm electrode. In the second experiment, the maximal vertical sizes were 22, 23, 22, and 23 mm at 10, 20, 30, and 40 W, respectively, with the 2-cm electrode. In the third experiment, the 18 G electrode had better water permeability than the 19 G electrode. In the fourth experiment, all pigs survived. Complications occurred in 1/5 (18 G electrode) and 4/7 (19 G electrode) pigs.
Conclusion
We performed EUS-RFA in pigs and concluded that it may be feasible to perform RFA of lesions near the stomach.




Similar content being viewed by others
References
Shiina S, Tateishi R, Arano T, Uchino K, Enooku K, Nakagawa H, et al. Radiofrequency ablation for hepatocellular carcinoma: 10-year outcome and prognostic factors. Am J Gastroenterol. 2012;107:569–77.
Makuuchi M. Clinical practice guidelines for hepatocellular carcinoma—the Japan Society of Hepatology 2009 update. Hepatol Res. 2010;40:2–144.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–2.
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56:908–43.
Kokudo N, Takemura N, Hasegawa K, Takayama T, Kubo S, Shimada M, et al. Clinical practice guidelines for hepatocellular carcinoma: the Japan Society of Hepatology 2017 (4th JSH-HCC guidelines) 2019 update. Hepatol Res. 2019;49:1109–13.
Nishigaki Y, Tomita E, Hayashi H, Suzuki Y, Iritani S, Kato T, et al. Efficacy and safety of radiofrequency ablation for hepatocellular carcinoma in the caudate lobe of the liver. Hepatol Res. 2013;43:467–74.
El-Gendi A, El-Shafei M, Abdel-Aziz F, Bedewy E. Intraoperative ablation for small HCC not amenable for percutaneous radiofrequency ablation in child A cirrhotic patients. J Gastrointest Surg. 2013;17:712–8.
Kariyama K, Nouso K, Wakuta A, Kishida M, Nishimura M, Wada N, et al. Percutaneous radiofrequency ablation for treatment of hepatocellular carcinoma in the caudate lobe. Am J Roentgenol. 2011;197:W571–5.
Hirooka M, Iuchi H, Kumagi T, Shigematsu S, Hiraoka A, Uehara T, et al. Virtual sonographic radiofrequency ablation of hepatocellular carcinoma visualized on CT but not on conventional sonography. Am J Roentgenol. 2006;186:S255–S260260.
Crocetti L, Lencioni R, Debeni S, See TC, Pina CD, Bartolozzi C. Targeting liver lesions for radiofrequency ablation: an experimental feasibility study using a CT-US fusion imaging system. Investig Radiol. 2008;43:33–9.
Clasen S, Boss A, Schmidt D, Schraml C, Fritz J, Schick F, et al. MR-guided radiofrequency ablation in a 0.2-T open MR system: technical success and technique effectiveness in 100 liver tumors. J Magn Reson Imaging. 2007;26:1043–52.
Yoshida T, Yamashita Y, Kitano M. Endoscopic ultrasound for early diagnosis of pancreatic cancer. Diagnostics. 2019;9:81.
Nguyen P, Feng JC, Chang KJ. Endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration (FNA) of liver lesions. Gastrointest Endosc. 1999;50:357–61.
Gaidhane M, Smith I, Ellen K, Gatesman J, Habib N, Foley P, et al. Endoscopic ultrasound-guided radiofrequency ablation (EUS-RFA) of the pancreas in a porcine model. Gastroenterol Res Pract. 2012;2012:431451.
Seicean A, Tefas C, Ungureanu B, Saftoiu A. Endoscopic ultrasound guided radiofrequency ablation in pancreas. Hepatogastroenterology. 2014;61:1717–21.
Rustagi T, Chhoda A. Endoscopic radiofrequency ablation of the pancreas. Dig Dis Sci. 2017;62:843–50.
Attili F, Boskoski I, Bove V, Familiari P, Costamagna G. EUS-guided radiofrequency ablation of a hepatocellular carcinoma of the liver. VideoGIE. 2018;3:149–50.
Shibata T, Niinobu T, Ogata N. Comparison of the effects of in-vivo thermal ablation of pig liver by microwave and radiofrequency coagulation. J Hepatobiliary Pancreat Surg. 2000;7:592–8.
Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, et al. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc. 2011;73:149–53.
Lah JJ, Kuo JV, Chang KJ, Nguyen PT. EUS-guided brachytherapy. Gastrointest Endosc. 2005;62:805–8.
Carrara S, Arcidiacono PG, Albarello L, Addis A, Enderle MD, Boemo C, et al. Endoscopic ultrasound-guided application of a new internally gas-cooled radiofrequency ablation probe in the liver and spleen of an animal model: a preliminary study. Endoscopy. 2008;40:759–63.
Di Matteo F, Grasso R, Pacella CM, Martino M, Pandolfi M, Rea R, et al. EUS-guided Nd:YAG laser ablation of a hepatocellular carcinoma in the caudate lobe. Gastrointest Endosc. 2011;73:632–6.
Chai W, Zhao Q, Song H, Cheng C, Tian G, Jiang T. Treatment response and preliminary efficacy of hepatic tumour laser ablation under the guidance of percutaneous and endoscopic ultrasonography. World J Surg Oncol. 2019;17:133.
Varadarajulu S, Jhala NC, Drelichman ER. EUS-guided radiofrequency ablation with a prototype electrode array system in an animal model (with video). Gastrointest Endosc. 2009;70:372–6.
Shibata T, Maetani Y, Isoda H, Hiraoka M. Radiofrequency ablation for small hepatocellular carcinoma: prospective comparison of internally cooled electrode and expandable electrode. Radiology. 2006;238:346–53.
Itoi T, Isayama H, Sofuni A, Itokawa F, Tamura M, Watanabe Y, et al. Evaluation of effects of a novel endoscopically applied radiofrequency ablation biliary catheter using an ex-vivo pig liver. J Hepatobiliary Pancreat Sci. 2012;19:543–7.
Acknowledgements
We would like to thank Taewoong Medical for volunteering to carry out Experiment 3 and providing valuable data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shuya Maeshima, Yoshiyuki Ida, Ryo Shimizu, Yuki Kawaji, Takashi Tamura, Jun-ya Nuta, Kei-ichi Hatamaru, Masahiro Itonaga, Masatoshi Kudo, and Masayuki Kitano declare that they have no conflicts of interest. This research was supported by the Research and Development Committee Program of The Japan Society of Ultrasonics in Medicine. This research was also supported by scholarship donations from Mochida Pharmaceutical, Sumitomo Dainippon Pharma, MSD, Chugai Pharmaceutical, and EA Pharma. The devices used in this research were provided by Century Medical and Taewoong Medical.
Research involving human participants and/or animals
All experiments were performed at Kobe Medical Device Development Center (MEDDEC) (Kobe, Japan) in cooperation with IVTeC (Tokyo, Japan). We performed animal experiments based on the IVTeC guidelines for animal experiments, which were enacted based on the “Act on Welfare and Management of Animals, Act No. 105 of October 1, 1973” and “Ordinances on Welfare and Management of Animals, Hyogo Prefecture Ordinance No. 8 of March 29, 1993,” and taking into account the importance and characteristics of animal experiments in education and research in life sciences. All institutional and national guidelines for the care and use of laboratory animals were followed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Maeshima, S., Ida, Y., Shimizu, R. et al. Endoscopic ultrasound-guided radiofrequency ablation of porcine liver. J Med Ultrasonics 47, 435–443 (2020). https://doi.org/10.1007/s10396-020-01013-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-020-01013-x