Abstract
Purpose
The goal of the Stanford Tobacco Treatment Initiative was to improve referrals from primary care clinics to a specialty tobacco addiction treatment clinic.
Methods
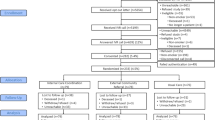
Lean A3 problem solving was used to map current state, perform a cause and effect analysis, develop key drivers for program referrals, and ideate tests of change. We discarded ideas that put any additional burden on on-the-ground providers, favouring automated and sustainable processes. After prioritizing for feasibility and impact, plan-do-study-act (PDSA) cycles were performed on the following interventions: education and outreach, referral champions, and automated referrals.
Results
Following implementation, referrals to the specialty tobacco treatment clinic increased by 600% and had no impact on clinic provider workflow.
Conclusion
The new process spread through all of Stanford Primary Care clinics, has sustained over time, and could serve as a model for other institutions seeking to enhance capacity for tobacco treatment in their health care system using process improvement methodology.


Similar content being viewed by others
References
Babb S (2017) Quitting smoking among adults—United States, 2000–2015. MMWR Morb Mortal Wkly Rep 65:1205–1211
Bloom EL, Burke MV, Kotsen C, Goldstein AO, Ripley-Moffitt C, Steinberg MB, Dailey M, Hunt LE, Bars MP (2018) Billing practices among US tobacco use treatment providers. J Addict Med 12:381. https://doi.org/10.1097/ADM.0000000000000423
Cinciripini PM, Karam-Hage M, Kypriotakis G, Robinson JD, Rabius V, Beneventi D, Minnix JA, Blalock JA (2019) Association of a comprehensive smoking cessation program with smoking abstinence among patients with cancer. JAMA Netw Open 2:e1912251. https://doi.org/10.1001/jamanetworkopen.2019.12251
Deming WE (1986) Out of the crisis. MIT Center for Advanced Engineering Studies Press, Cambridge MA
Gali K, Pike B, Kendra MS, Tran C, Fielding-Singh P, Jimenez K, Mirkin R, Prochaska JJ (2020) Integration of tobacco treatment services into cancer care at Stanford. Int J Environ Res Public Health 17:2101
Ghosh M, Sobek DK II (2015) A problem-solving routine for improving hospital operations. J Health Organ Manag 29:252–270
Killen JD, Fortmann SP, Schatzberg AF, Arredondo C, Murphy G, Hayward C, Celio M, Cromp D, Fong D, Pandurangi M (2008) Extended cognitive behavior therapy for cigarette smoking cessation. Addiction 103:1381–1390. https://doi.org/10.1111/j.1360-0443.2008.02273.x
Larson DB, Mickelsen LJ (2015) Project management for quality improvement in radiology. Am J Roentgenol 205:W470–W477
Laude JR, Bailey SR, Crew E, Varady A, Lembke A, McFall D, Jeon A, Killen D, Killen JD, David SP (2017) Extended treatment for cigarette smoking cessation: a randomized control trial. Addiction 112:1451–1459. https://doi.org/10.1111/add.13806
Levy DE, Klinger EV, Linder JA, Fleegler EW, Rigotti NA, Park ER, Haas JS (2017) Cost-effectiveness of a health system-based smoking cessation program. Nicotine Tob Res 19:1508–1515
Movsisyan A (2019) Evaluating the implementation of a comprehensive tobacco cessation program. Unpublished thesis
Nahhas GJ, Wilson D, Talbot V, Cartmell KB, Warren GW, Toll BA, Carpenter MJ, Cummings KM (2016) Feasibility of implementing a hospital-based “opt-out” tobacco-cessation service. Nicotine Tob Res 19:937–943
Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D (2015) SQUIRE 2.0 (Standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. J Contin Educ Nurs 46:501–507
Rabius V, Karam-Hage M, Blalock JA, Cinciripini PM (2014) “Meaningful use” provides a meaningful opportunity. Cancer 120:464–468
Silagy CA, Stead LF (2001) Physician advice for smoking cessation. Cochrane Database Syst Rev 2001:CD000165 [this is not the most recent version]. https://doi.org/10.1002/14651858.CD000165
Sobek II DK, Smalley A (2008) Understanding A3 thinking: a critical component of Toyota’s PDCA management system. Productivity Press, New York
Solberg LI, Maciosek MV, Edwards NM, Khanchandani HS, Goodman MJ (2006) Repeated tobacco-use screening and intervention in clinical practice: health impact and cost effectiveness. Am J Prev Med 31:62–71
US Department of Health and Human Services (2014) The health consequences of smoking—50 years of progress: a report of the surgeon general. US Department of Health and Human Services, Atlanta, GA. https://onlinelibrary.wiley.com/doi/abs/10.1111/dar.12309. Accessed 8 Dec 2019
Warren GW, Marshall JR, Cummings KM, Zevon MA, Reed R, Hysert P, Mahoney MC, Hyland AJ, Nwogu C, Demmy T (2014) Automated tobacco assessment and cessation support for cancer patients. Cancer 120:562–569
Williams JM, Steinberg ML, Kenefake AN, Burke MV (2016) An argument for change in tobacco treatment options guided by the ASAM criteria for patient placement. J Addict Med 10:291–299. https://doi.org/10.1097/ADM.0000000000000239
Acknowledgements
The authors would like to thank the Clinical Effectiveness and Leadership Training program at Stanford Health Care, Stanford Primary Care, and the Stanford Department of Psychiatry and Behavioral Sciences for sponsoring this quality improvement initiative.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Institutional Review Board review for research was waived because this was a quality improvement project.
Informed consent [optional]
N/A
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kendra, M.S., Dang, J., Artandi, M. et al. Connecting tobacco users in the primary care setting to comprehensive tobacco treatment: a quality improvement initiative. J Public Health (Berl.) 30, 1213–1218 (2022). https://doi.org/10.1007/s10389-020-01401-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-020-01401-0