Abstract
Aim
It is well known that the use of routine health check-ups is associated with socio-demographic and lifestyle factors. However, the link between psychological factors and the use of routine health check-ups has not been investigated intensively so far. Consequently, the purpose of this study was to determine the psychological factors associated with routine health check-ups.
Subjects and methods
Cross-sectional data were obtained from a population-based study (German Aging Survey) of individuals ≥40 years of age and residing in private households in Germany in the year 2014 (n = 7708). Screening data and data on psychological factors were collected in self-administered questionnaires. Multiple logistic regressions were used to identify psychological correlates of screening behavior, adjusted for socio-demographic, lifestyle and health-related variables.
Results
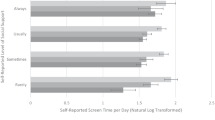
Of the participants, 65.4% used routine health check-ups regularly. After adjusting for various potential confounders, multiple logistic regressions showed that the use of routine health check-ups was positively associated with life satisfaction, positive affect, optimism, self-efficacy, self-esteem and self-regulation, whereas the outcome measure was not significantly associated with loneliness, negative affect and perceived stress. Furthermore, the outcome measure was positively associated with age, being married and living together with a spouse or partner, body mass index, being a non-daily smoker, drinking alcohol less than once a day and exercising. However, it was not associated with gender, income, number of physical illnesses or region.
Conclusions
The current study stresses the importance of the association between screening behavior and psychological factors. This may help to identify individuals at risk for underuse.
Similar content being viewed by others
Change history
30 January 2018
The journal had been advised to revise the title so that Clarivate Analytics can try to count the citations more accurately. There’s been confusion due to the existence of another journal with the same name.
References
Antonovsky A (1993) The structure and properties of the sense of coherence scale. Soc Sci Med 36:725–733
Bowen DJ, Alfano CM, McGregor BA, Andersen MR (2004) The relationship between perceived risk, affect, and health behaviors. Cancer Detect Prev 28:409–417
Brandtstädter J, Wentura D (1994) Veränderungen der Zeit-und Zukunftsperspektive im Übergang zum höheren Erwachsenenalter: entwicklungspsychologische und differentielle Aspekte. Z Entwickl Padagogis 26:2–21
Bundesministerium für Gesundheit (2016) Teilnahme am gesetzlichen Gesundheits-Check-up. Gliederungsmerkmale: Jahre, Deutschland, Alter, Geschlecht. www.gbe-bund.de. Accessed 26 Sep 2016
Calnan M (1985) Patterns in preventive behavior: A study of women in middle age. Soc Sci Med 20:263–268
Casey MM, Call KT, Klingner JM (2001) Are rural residents less likely to obtain recommended preventive healthcare services? Am J Prev Med 21:182–188
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Crawford JR, Henry JD (2004) The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br J Clin Psychol 43:245–265
Freund AM, Baltes PB (2002) Life-management strategies of selection, optimization and compensation: Measurement by self-report and construct validity. J Pers Soc Psychol 82:642–662
Gierveld JDJ, Van Tilburg T (2006) A 6-item scale for overall, emotional, and social loneliness confirmatory tests on survey data. Res Aging 28:582–598
Hautzinger M, Bailer M (1993) ADS-Allgemeine Depressions-Skala. Weinheim, Beltz
Hoebel J, Richter M, Lampert T (2013) Sozialer Status und Teilnahme am Gesundheits-Check-up von Männern und Frauen in Deutschland: Ergebnisse der GEDA-Studie 2009 und 2010 Deutsches Ärzteblatt 110:679–685
Hoebel J, Starker A, Jordan S, Richter M, Lampert T (2014) Determinants of health check attendance in adults: findings from the cross-sectional German Health Update (GEDA) study. BMC Public Health 14:913
Jo H, Lee S, Ahn MO, Jung SH (2003) Structural relationship of factors affecting health promotion behaviors of Korean urban residents. Health Promot Int 18:229–236
Kinney AY, Bloor LE, Martin C, Sandler RS (2005) Social ties and colorectal cancer screening among blacks and whites in North Carolina. Cancer Epidemiol Biomark Prev 14: 182–189
Kivimäki M, Feldt T, Vahtera J, Nurmi J-E (2000) Sense of coherence and health: evidence from two cross-lagged longitudinal samples. Soc Sci Med 50:583–597
Klaus D, Engstler H (2016) Daten und Methoden des Deutschen Alterssurveys. In: Mahne K, Wolff JK, Simonson J, Tesch-Römer C (eds) Altern im Wandel: Zwei Jahrzehnte Deutscher Alterssurvey (DEAS). Berlin pp 25–42
Klaus D, Engstler H, Mahne K, Wolff JK, Simonson J, Wurm S, Tesch-Römer C (2017) Cohort profile: The German Ageing Survey (DEAS). Int J Epidemiol: 1–8. https://doi.org/10.1093/ije/dyw326
Lin EH, Peterson C (1990) Pessimistic explanatory style and response to illness. Behav Res Ther 28:243–248
Lüngen M, Siegel M, Drabik A, Büscher G, von Törne I (2009) Ausmaß und Gründe für Ungleichheiten der gesundheitlichen Versorgung in Deutschland Studien zu Gesundheit, Medizin und Gesellschaft 5/2009
Mulkana SS, Hailey BJ (2001) The role of optimism in health-enhancing behavior. Am J Health Behav 25:388–395
Neller K (2005) Kooperation und Verweigerung. Eine Non-Response-Studie ZUMA Nachrichten 29:9–36
Ng DM, Jeffery RW (2003) Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol 22:638–642
O'Malley AS, Mandelblatt J (2003) Delivery of preventive services for low-income persons over age 50: a comparison of community health clinics to private doctors' offices. J Community Health 28:185–197
Oscarsson MG, Wijma BE, Benzein EG (2008) ‘I do not need to… I do not want to… I do not give it priority…’—Why women choose not to attend cervical cancer screening. Health Expect 11:26–34
Pavot W, Diener E (1993) Review of the satisfaction with life scale. Psychol Assess 5:164–172
Pirraglia PA, Sanyal P, Singer DE, Ferris TG (2004) Depressive symptom burden as a barrier to screening for breast and cervical cancers. J Women's Health 13:731–738
Richter M, Brand H, Rössler G (2002) Sozioökonomische Unterschiede in der Inanspruchnahme von Früherkennungsuntersuchungen und Maßnahmen der Gesundheitsförderung in NRW. Gesundheitswesen 64:417–424
Ridolfi DR, Crowther JH (2013) The link between women's body image disturbances and body-focused cancer screening behaviors: A critical review of the literature and a new integrated model for women. Body Image 10:149–162
Rimer BK, Orleans CT, Keintz MK, Cristinzio S, Fleisher L (1990) The older smoker. Status, challenges and opportunities for intervention. Chest J 97:547–553
Rosenberg M (1965) Society and the adolescent self-image. Princeton University Press, Princeton
Schwarzer R, Jerusalem M (1999) Skalen zur Erfassung von Lehrer- und Schülermerkmalen. Dokumentation der psychometrischen Verfahren im Rahmen der Wissenschaftlichen Begleitung des Modellversuchs Selbstwirksame Schulen. Freie Universität Berlin, Berlin
Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S (2006) Dispositional optimism and health behaviour in community-dwelling older people: Associations with healthy ageing. Br J Health Psychol 11:71–84
Thorpe JM, Kalinowski CT, Patterson ME, Sleath BL (2006) Psychological distress as a barrier to preventive care in community-dwelling elderly in the United States. Med Care 44:187–191
Tolma EL, Reninger BM, Evans A, Ureda J (2006) Examining the theory of planned behavior and the construct of self-efficacy to predict mammography intention. Health Educ Behav 33:233–251
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 30:473–483
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54:1063–1070
Woolhandler S, Himmelstein DU (1988) Reverse targeting of preventive care due to lack of health insurance. Jama 259:2872–2874
Ylöstalo P, Ek E, Laitinen J, Knuuttila M (2003) Optimism and life satisfaction as determinants for dental and general health behavior—oral health habits linked to cardiovascular risk factors. J Dent Res 82:194–199
Zhang P, Too G, Irwin KL (2000) Utilization of preventive medical services in the United States: a comparison between rural and urban populations. J Rural Health 16:349–356
Ziegelmann JP, Lippke S (2006) Selbstregulation in der Gesundheitsverhaltensänderung: Strategienutzung und Bewältigungsplanung im jungen, mittleren und höheren Alter. Z Gesundheitspsychol 14:82–90
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Please note that an ethical statement for the DEAS study was not necessary because criteria for the need of an ethical statement were not met (risk for the respondents, lack of information about the aims of the study, examination of patients).
Informed consent
Prior to the interview, written informed consent was given by all study participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
The original version of this article was revised: Due to the existence of another journal with the same name, the Publisher has added a subtitle, “From Theory to Practice.” Effective as of January 2018, the new title of this Journal is Journal of Public Health: From Theory to Practice.
A correction to this article is available online at https://doi.org/10.1007/s10389-017-0893-1.
Electronic supplementary material
ESM 1
(DOC 213 kb)
Rights and permissions
About this article
Cite this article
Hajek, A., Bock, JO. & König, HH. The use of routine health check-ups and psychological factors—a neglected link. Evidence from a population-based study. J Public Health 26, 137–144 (2018). https://doi.org/10.1007/s10389-017-0840-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-017-0840-1