Abstract
Aim
International research has shown that the characteristics of areas such as neighbourhood socioeconomic disadvantage, are associated with mental health; however, multilevel modelling approaches have shown that little variance in depression scores is explained at the area level. This study investigated the distribution of depression across suburbs in the Canberra and surrounding region of Australia, and the influence of area- and individual-level measures of socioeconomic position.
Subject and methods
Analysis of data is taken from Wave 3 of the Personality and Total Health (PATH) through Life study with 3,342 respondents aged 28–32 years or 48–52 years who were residents of Canberra and Queanbeyan. Depression was assessed with the Patient Health Questionnaire. Multilevel logistic regression models were used to evaluate variance components and compare suburb measures of socioeconomic circumstances and respondent-reported household income.
Results
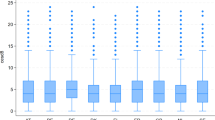
Less than 1% of variance in the distribution of depression was explained at the area level. While area-level socioeconomic measures were associated with depression; this effect was weak and largely explained by the inclusion of individual-level income. Further analysis did demonstrate a non-linear relationship between area-level socioeconomic measures and depression, with some evidence of an association between the most disadvantaged suburbs and greater prevalence of depression over and above the effect of individual characteristics.
Conclusion
We found little evidence of variance in depression at the area level but did find that the prevalence of depression was elevated in the most disadvantaged suburbs. Individual risk factors appear to have the strongest influence on depression.


Similar content being viewed by others
References
Anstey KJ, Christensen H, Butterworth P, Easteal S, Mackinnon A, Jacomb T, Maxwell K, Rodgers B, Windsor TD, Cherbuin N, Jorm AF (2011) Cohort profile: The PATH Through Life project. Int J Epidemiol doi:10.1093/ije/dyr025
Australian Bureau of Statistics (2004) Australian standard geographical classification (ASGC). ABS, Canberra
Australian Bureau of Statistics (2008a) Information paper: an introduction to socio-economic indexes for areas (SEIFA), 2006 ABS, Canberra
Australian Bureau of Statistics (2008b) Socio-economic indexes for areas (SEIFA), Data only, 2006 ABS, Canberra
Bayer JK, Hiscock H, Morton-Allen E, Ukoumunne OC, Wake M (2007) Prevention of mental health problems: rationale for a universal approach. Arch Dis Child 92(1):34–38
Butterworth P, Rodgers B, Jorm AF (2006) Examining geographic and household variation in mental health in Australia. Aust New Zealand J Psychiarty 40(5):491–497
Butterworth P, Rodgers B, Windsor TD (2009) Financial hardship, socio-economic position and depression: results from the PATH Through Life Survey. Social Sci Med 69:229–237
Crump C, Sundquist K, Sundquist J, Winkleby MA (2011) Neighborhood deprivation and psychiatric medication prescription: a Swedish national multilevel study. Ann Epidemiol 21:231–237
Diez-Roux AV (2000) Multilevel analysis in public health research. Annu Rev Public Health 21:171–192
Faris REL, Dunham HW (1939) Mental disorders in urban areas. University of Chicago Press, Chicago
Fortney J, Rushton G, Wood S, Zhang L, Xu S, Dong F, Rost K (2007) Community-level risk factors for depression hospitalizations. Adm Policy Ment Health Ment Health Serv Res 34(4):343–352
Haines VA, Beggs JJ, Hurlbert JS (2011) Neighborhood disadvantage, network social capital, and depressive symptoms. J Health Soc Behav 52(1):58–73
Link BG, Phelan J (1995) Social conditions as fundamental causes of disease. J Health Soc Behav 35:80–94
Lowe B, Spitzer RL, Grafe K, Kroenke K, Quenter A, Zipfel S, Buchholz C, Witte S, Herzog W (2004) Comparative validity of three screening questionnaires for DSM-IV depressive disorders and physicians’ diagnoses. J Affect Disord 78(2):131–140
Mair C, Diez-Roux AV, Galea S (2008) Are neighbourhood characteristics associated with depressive symptoms? A review of evidence. J Epidemiol Community Health 62:940–946
Mirowsky J, Ross CE (1999) Economic hardship across the life course. Am Sociol Rev 64(4):549–569
Mirowsky J, Ross CE (2001) Age and the effect of economic hardship on depression. J Health Soc Behav 42:132–150
Page A, Morrell S, Taylor R, Carter G, Dudley M (2006) Divergent trends in suicide by socio-economic status in Australia. Soc Psychiatry Psychiatr Epidemiol 41(11):911–917
Pickett KE, Pearl M (2001) Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health 55(2):111–122
Pikhartova J, Chandola T, Kubinova R, Bobak M, Nicholson A, Pikhart H (2009) Neighbourhood socioeconomic indicators and depressive symptoms in the Czech Republic: a population based study. Int J Public Health 54:283–293
Ross CE (2000) Neighborhood disadvantage and adult depression. J Health Soc Behav 41(2):177–187
Snijders TAB, Bosker RJ (1999) Multilevel analysis: an introduction to basic and advanced multilevel modeling. Sage, Thousand Oaks, CA
Spitzer RL, Williams JBW, Kroenke K, Linzer M, Degruy FV, Hahn SR, Brody D, Johnson JG (1994) Utility of new procedure for diagnosing mental-disorders in primary-care: the Prime-MD-1000 Study. JAMA 272(22):1749–1756
Spitzer RL, Kroenke K, Williams JBW (1999) Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 282(18):1737–1744
Wainwright NWJ, Surtees PG (2004) Area and individual circumstances and mood disorder prevalence. Br J Psychiatry 185:227–232
Weich S (2005) Absence of spatial variation in rates of the common mental disorders. J Epidemiol Community Health 59:254–257
Weich S, Holt G, Twigg L, Jones K, Lewis G (2003a) Geographic variation in the prevalence of common mental disorders in Britain: a multilevel investigation. Am J Epidemiol 157(8):730–737
Weich S, Twigg L, Holt G, Lewis G, Jones K (2003b) Contextual risk factors for the common mental disorders in Britain: a multilevel investigation of the effects of place. J Epidemiol Community Health 57(8):616–621
Weiss L, Ompad D, Galea S, Vlahov D (2007) Defining neighborhood boundaries for urban health research. Am J Prev Med 32:S154–S159
Acknowledgements
Thanks to K. Anstey, H. Christensen, A. Mackinnon, S. Easteal, T. Jacomb, K. Maxwell and the team of PATH interviewers for their contribution to the research. Funding for data collection was provided by Unit Grant 973302 and Program Grant 179805 from the National Health and Medical Research Council (NHMRC). P. Butterworth was funded by NHMRC Fellowship No. 525410.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Butterworth, P., Leach, L.S. & Olesen, S.C. Mental health in the suburbs: an investigation of differences in the prevalence of depression across Canberra suburbs using data from the PATH Through Life Study. J Public Health 20, 525–531 (2012). https://doi.org/10.1007/s10389-011-0482-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-011-0482-7