Abstract
Background
Gastric cancer is the second most common malignancy, overlapping with thoracic esophageal cancer (TEC). Among them, metachronous gastric tube cancers after TEC surgery have been increasing. The aims of this study were to examine the clinicopathological factors and treatment outcomes of gastric tube cancer (GTC) after TEC surgery.
Methods
Thirty-three GTCs in 30 cases after TEC treated between 1997 and 2016 were investigated retrospectively.
Results
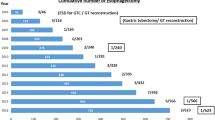
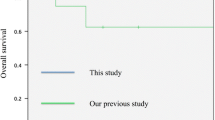
Most cases were males. The median interval from TEC surgery to GTC occurrence was 57 (6.5–107.5) months. Almost 2/3 lesions occurred in the lower third of the gastric tube (21/33); 29 lesions (in 26 cases) were superficial cancers, and 4 lesions were advanced cancers. Twenty-two lesions of superficial cancer were differentiated type, and the remaining seven lesions were undifferentiated type. Treatment for superficial cancer had previously been performed with partial gastric tube resection (10 lesions), and the number of cases undergoing endoscopic submucosal dissection (ESD) had increased recently (19 lesions). Most cases with superficial cancer survived without relapse. Four lesions of advanced cancer were found after a relatively long interval following TEC surgery. Most lesions of advanced cancer were scirrhous, undifferentiated type, and they died due to GTC.
Conclusion
GTCs may occur late in the postoperative course following TEC surgery. If they are discovered at an early stage, these lesions can be cured with ESD. Long-term periodic endoscopic examinations after TEC surgery are important.




Similar content being viewed by others
References
Poon RT, Law SY, Chu KM, et al. Multiple primary cancers in esophageal squamous cell carcinoma: incidence and implications. Ann Thorac Surg. 1998;65:1529–34.
Nagasawa S, Onda M, Sasajima K, et al. Multiple primary malignant neoplasms in patients with esophageal cancer. Dis Esophagus. 2000;13:226–30.
Kokawa A, Yamaguchi H, Tachimori Y, et al. Other primary cancers occurring after treatment of superficial oesophageal cancer. Br J Surg. 2001;88:439–43.
Okamoto N, Ozawa S, Kitagawa Y, et al. Metachronous gastric carcinoma from a gastric tube after radical surgery for esophageal carcinoma. Ann Thorac Surg. 2004;77:1189–92.
Mukasa M, Takedatsu H, Matsuo K, et al. Clinical characteristics and management of gastric tube cancer with endoscopic submucosal dissection. World J Gastroenterol. 2015;21:919–25.
Sugiura T, Kato H, Tachimori Y, et al. Second primary carcinoma in the gastric tube constructed as an esophageal substitute after esophagectomy. J Am Coll Surg. 2002;194:578–83.
Ahn HS, Kim JW, Yoo MW, et al. Clinicopathological features and surgical outcomes of patients with remnant gastric cancer after a distal gastrectomy. Ann Surg Oncol. 2008;15:1632–9.
Shigemitsu K, Naomoto Y, Shirakawa Y, et al. Five cases of early gastric cancer in the reconstructed gastric tube after radical resection for esophageal cancer. Jpn J Clin Oncol. 2002;32:425–9.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Bamba T, Kosugi S, Takeuchi M, et al. Surveillance and treatment for second primary cancer in the gastric tube after radical esophagectomy. Surg Endosc. 2010;24:1310–7.
Nonaka S, Oda I, Sato C, et al. Endoscopic submucosal dissection for gastric tube cancer after esophagectomy. Gastrointest Endosc. 2014;79:260–70.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Shirakawa Y, Noma K, Koujima T, et al. Operative technique of antethoracic esophageal reconstruction with pedicled jejunal flap. Esophagus. 2015;15:57–64.
Takenaka R, Kawahara Y, Okada H, et al. Endoscopic submucosal dissection for cancers of the remnant stomach after distal gastrectomy. Gastrointest Endosc. 2008;67:359–63.
Imagawa A, Okada H, Kawahara Y, et al. Endoscopic submucosal dissection (ESD) for early gastric cancer: results and degrees of technical difficulty as well as success. Endoscopy. 2006;38:987–90.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: part I. Esophagus. 2017;14:1–36.
Japan Esophageal Society. Japanese classification of esophageal cancer, 11th edition: part II and III. Esophagus. 2017;14:37–65.
Sobin LH, Gospodarowicz MK, Wittekind CH. TNM classification of malignant tumors (UICC international union against cancer). 7th ed. Oxford: Wiley-Blackwell; 2009.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Warren S, Gates O. Multiple primary malignant tumors. A survey of the literature and a statistical study. Am J Cancer. 1932;16:1358–414.
Osumi W, Fujita Y, Hiramatsu M, et al. Endoscopic submucosal dissection allows less-invasive curative resection for gastric tube cancer after esophagectomy—a case series. Endoscopy. 2009;41:777–80.
Suzuki H, Kitamura M, Saito R, et al. Cancer of the gastric tube reconstructed through the posterior mediastinal route after radical surgery for esophageal cancer. Jpn J Thorac Cardiovasc Surg. 2001;49:466–9.
Kise Y, Kijima H, Shimada H, et al. Gastric tube cancer after esophagectomy for esophageal squamous cell cancer and its relevance to Helicobacter pylori. Hepatogastroenterology. 2003;50:408–11.
Dixon MF, Mapstone NP, Neville PM, et al. Bile reflux gastritis and intestinal metaplasia at the cardia. Gut. 2002;51:351–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent or substitute for it was obtained from all patients for being included in the study.
Rights and permissions
About this article
Cite this article
Shirakawa, Y., Noma, K., Maeda, N. et al. Clinical characteristics and management of gastric tube cancer after esophagectomy. Esophagus 15, 180–189 (2018). https://doi.org/10.1007/s10388-018-0611-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-018-0611-2