Abstract
Purpose
To compare endonasal dacryocystorhinostomy (EN-DCR) with sheath-guided dacryoendoscopic probing and bicanalicular intubation (SG-BCI) by evaluating tear meniscus area (TMA) and total high-order aberrations (HOAs) for primary acquired nasolacrimal duct obstruction (PANDO).
Method
We retrospectively reviewed 56 eyes of 42 patients (7 men, 35 women; age, 72.7±13.1 years) who underwent EN-DCR or SG-BCI for PANDO in Toyama University Hospital from February 2020 to June 2022. In the EN-DCR and SG-BCI groups, we measured the patency of the lacrimal passage, preoperative and postoperative TMA, and HOAs of the central 4 mm of the cornea using optical coherence tomography (AS-OCT), six months postoperatively.
Results
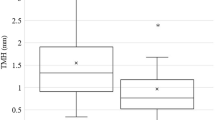
There was a positive correlation between preoperative TMA and preoperative HOAs in all cases. Postoperative patency of lacrimal passage was 100% in the EN-DCR and 80.8% in the SG-BCI group. There was a significant difference in the number of passages between the two groups (p = 0.01). Preoperative TMA and HOAs showed a significant postoperative decrease in both groups (EN-DCR group: p<0.01, p<0.01, SG-BCI group: p<0.01, p=0.03, respectively). We then calculated the rate of change of preoperative and postoperative TMA and HOAs and compared them between the two groups. The rate of change was significantly higher in the EN-DCR group than that in the SG-BCI group (TMA, p=0.03; HOAs, p=0.02).
Conclusion
Although both EN-DCR and SG-BCI are effective for PANDO, our results suggest that EN-DCR is more effective in improving TMA and HOAs.



Similar content being viewed by others
Reference
Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986;93:1055–63.
Hartikainen J, Antila J, Varpula M, Puukka P, Seppä H, Grénman R. Prospective randomized comparison of endonasal endoscopic dacryocystorhinostomy and external dacryocystorhinostomy. Laryngoscope. 1998;108:1861–6.
Hartikainen J, Grenman R, Puukka P, Seppä H. Prospective randomized comparison of external dacryocystorhinostomy and endonasal laser dacryocystorhinostomy. Ophthalmology. 1998;105:1106–13.
Tsirbas A, Davis G, Wormald PJ. Mechanical endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg. 2004;20:50–6.
Vinciguerra A, Resti AG, Rampi A, Bussi M, Bandello F, Trimarchi M. Endoscopic and external dacryocystorhinostomy: a therapeutic proposal for distal acquired lacrimal obstructions. Eur J Ophthalmol. 2023;33:1287–93.
Angrist RC, Dortzbach RK. Silicone intubation for partial and total nasolacrimal duct obstruction in adults. Ophthalmic Plast Reconstr Surg. 1985;1:51–4.
Psilas K, Eftaxias V, Kastanioudakis J, Kalogeropoulos C. Silicone intubation as an alternative to dacryocystorhinostomy for nasolacrimal drainage obstruction in adults. Eur J Ophthalmol. 1993;3:71–6.
Connell PP, Fulcher TP, Chacko E, O’ Connor MJ, Moriarty P. Long term follow up of nasolacrimal intubation in adults. Br J Ophthalmol. 2006;90:435–6.
Fulcher T, O’Connor M, Moriarty P. Nasolacrimal intubation in adults. Br J Ophthalmol. 1998;82:1039–41.
Sasaki T, Sounou T, Sugiyama K. Dacryoendoscopic surgery and tube insertion in patients with common canalicular obstruction and ductal stenosis as a frequent complication. Jpn J Ophthalmol. 2009;53:145–50.
Kabata Y, Goto S, Takahashi G, Tsuneoka H. Vision-related quality of life in patients undergoing silicone tube intubation for lacrimal passage obstructions. Am J Ophthalmol. 2011;152:147-150.e2.
Mimura M, Ueki M, Oku H, Sato B, Ikeda T. Indications for and effects of Nunchaku-style silicone tube intubation for primary acquired lacrimal drainage obstruction. Jpn J Ophthalmol. 2015;59:266–72.
Kamao T, Zheng X, Shiraishi A. Outcomes of bicanalicular nasal stent inserted by sheath-guided dacryoendoscope in patients with lacrimal passage obstruction: a retrospective observational study. BMC Ophthalmol. 2021;21:103.
Taniguchi A, Yunoki T, Oiwake T, Hayashi A. Association between tear meniscus dimensions and higher-order aberrations in patients with surgically treated lacrimal passage obstruction. Int Ophthalmol. 2023;43:1135–41.
Tachino H, Fujisaka M, Fuchizawa C, Tsubota M, Takakura H, Ishida M, et al. Endonasal flap suture-dacryocystorhinostomy (eFS-DCR): a new surgical technique for nasolacrimal duct obstruction (NLDO). Acta Otolaryngol. 2015;135:162–8.
Tachino H, Takakura H, Shojaku H, Fujisaka M, Ito S, Oi Y, et al. Flap suturing endonasal dacryocystorhinostomy assisted by ultrasonic bone aspirator. Acta Otolaryngol. 2022;142:316–22.
Fukuda R, Usui T, Miyai T, Yamagami S, Amano S. Tear meniscus evaluation by anterior segment swept-source optical coherence tomography. Am J Ophthalmol. 2013;155(620–24):624.e1-2.
Ohtomo K, Ueta T, Fukuda R, Usui T, Miyai T, Shirakawa R, et al. Tear meniscus volume changes in dacryocystorhinostomy evaluated with quantitative measurement using anterior segment optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55:2057–61.
Koh S, Inoue Y, Ochi S, Takai Y, Maeda N, Nishida K. Quality of vision in eyes with epiphora undergoing lacrimal passage intubation. Am J Ophthalmol. 2017;181:71–8.
Demirci H, Elner VM. Double silicone tube intubation for the management of partial lacrimal system obstruction. Ophthalmology. 2008;115:383–5.
Inatani M, Yamauchi T, Fukuchi M, Denno S, Miki M. Direct silicone intubation using Nunchaku-style tube (NST-DSI) to treat lacrimal passage obstruction. Acta Ophthalmol Scand. 2000;78:689–93.
Nakamura J, Kamao T, Mitani A, Mizuki N, Shiraishi A. Comparison of the efficacies of 1.0 and 1.5-mm silicone tubes for the treatment of nasolacrimal duct obstruction. Sci Rep. 2022;12:11785.
Tsurumaru N, Noda Y, Yamakawa R. Surgical outcome of lacrimal passage intubation. Jpn J Ophthalmic Surg. 2016;29:473–6 ((in Japanese)).
Ibrahim OM, Dogru M, Takano Y, Satake Y, Wakamatsu TH, Fukagawa K, et al. Application of visante optical coherence tomography tear meniscus height measurement in the diagnosis of dry eye disease. Ophthalmology. 2010;117:1923–9.
Koh S, Maeda N, Ninomiya S, Watanabe H, Fujikado T, Tano Y, et al. Paradoxical increase of visual impairment with punctal occlusion in a patient with mild dry eye. J Cataract Refract Surg. 2006;32:689–91.
Kakizaki H, Zako M, Miyaishi O, Nakano T, Asamoto K, Iwaki M. The lacrimal canaliculus and sac bordered by the Horner’s muscle form the functional lacrimal drainage system. Ophthalmology. 2005;112:710–6.
Ali MJ, Zetzsche M, Scholz M, Hahn D, Gaffling S, Heichel J, et al. New insights into the lacrimal pump. Ocul Surf. 2020;18:689–98.
Feijo ED, Limongi RM, Matayoshi S. Fluorescein transit test time as a tool to assess lacrimal pump function after diode laser transcanalicular dacryocystorhinostomy and external dacryocysto-rhinostomy. Rhinology. 2018;56:274–8.
Su PY. Comparison of endoscopic and external dacryocystorhinostomy for treatment of primary acquired nasolacrimal duct obstruction. Taiwan J Ophthalmol. 2018;8:19–23.
Mitani A, Kamao T. Lacrimal duct obstruction surgery and tear clearance. J Eye. 2021;38:59–65 ((in Japanese)).
O’Donnell BA, Clement CI. Assessing patients with epiphora who are patent to syringing: clinical predictors of response to dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg. 2007;23:173–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
T. Shiina, None; T. Yunoki, None; H. Tachino, None; A. Hayashi, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Tatsuya Yunoki
About this article
Cite this article
Shiina, T., Yunoki, T., Tachino, H. et al. Comparative study of surgical outcomes regarding tear meniscus area and high-order aberrations between two different interventional methods for primary acquired nasolacrimal duct obstruction. Jpn J Ophthalmol 68, 139–145 (2024). https://doi.org/10.1007/s10384-024-01050-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-024-01050-w