Abstract
Purpose
To determine the cut-off points of minimum linear diameter (MLD) and base diameter (BD) at which the progression rate of idiopathic full-thickness macular holes (MHs) decreases before vitrectomy.
Study design
A retrospective study.
Methods
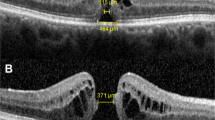
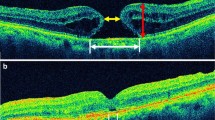
We investigated the differences in MLD and BD between baseline and operation days in patients with stages 2, 3, and 4 MHs using optical coherence tomography (OCT). Each difference in OCT parameters was divided by the time interval to calculate the MH progression rates and the cut-off points of MLD and BD.
Results
Overall, 269 patients (282 eyes) were included. It took an average of 36.02 ± 24.69 (7–197) days from baseline to operation. MLD and BD progressed faster in stages 2 and 3 without posterior vitreous detachment (PVD) than in stage 4 with PVD (MLD: p < 0.001 and p = 0.007; BD: p < 0.001 and p = 0.019, respectively). Simple linear regression showed the relationship between baseline MLD and BD, and the progression rate; the progression rate decreased as baseline MLD (p = 0.004) and BD increased ( p < 0.001). For baseline MLD and BD, the cut-off points where the progression rate decreased were 306.0 and 470.0 μm, respectively.
Conclusion
The group without PVD progressed faster than the group with PVD. Moreover, the progression rates were faster in MHs with MLD < 306.0 μm and BD < 470.0 μm. In these patients, vitrectomy without delay is expected to improve the visual prognosis.



Similar content being viewed by others
References
Eckardt C, Eckardt U, Groos S, Luciano L, Reale E. Removal of the internal limiting membrane in macular holes. Clinical and morphological findings. Ophthalmologe. 1997;94:545–51.
Abdelkader E, Lois N. Internal limiting membrane peeling in vitreo-retinal surgery. Surv Ophthalmol. 2008;53:368–96.
Madi HA, Masri I, Steel DH. Optimal management of idiopathic macular holes. Clin Ophthalmol. 2016;10:97–116.
Bae K, Kang SW, Kim JH, Kim SJ, Kim JM, Yoon JM. Extent of internal limiting membrane peeling and its impact on macular hole surgery outcomes: a randomized trial. Am J Ophthalmol. 2016;169:179–88.
Zhao PP, Wang S, Liu N, Shu ZM, Zhao JS. A review of surgical outcomes and advances for macular holes. J Ophthalmol. 2018;2018:7389412.
Ittarat M, Somkijrungroj T, Chansangpetch S, Pongsachareonnont P. Literature review of surgical treatment in idiopathic full-thickness macular hole. Clin Ophthalmol. 2020;14:2171–83.
de Bustros S. Vitrectomy for prevention of macular holes. Results of a randomized multicenter clinical trial. Vitrectomy for Prevention of Macular Hole Study Group. Ophthalmology. 1994;101:1055–9 (discussion 60).
Kim JW, Freeman WR, Azen SP, el-Haig W, Klein DJ, Bailey IL. Prospective randomized trial of vitrectomy or observation for stage 2 macular holes. Vitrectomy for Macular Hole Study Group. Am J Ophthalmol. 1996;121:605–14.
Ezra E. Idiopathic full thickness macular hole: natural history and pathogenesis. Br J Ophthalmol. 2001;85:102–8.
Kim JY, Kim RY, Kim M, Park YG, Park YH. Progression rate analysis of idiopathic macular hole using optical coherence tomography before vitrectomy: short-term results. Acta Ophthalmol. 2022;100:919–26.
Salter AB, Folgar FA, Weissbrot J, Wald KJ. Macular hole surgery prognostic success rates based on macular hole size. Ophthalmic Surg Lasers Imaging. 2012;43:184–9.
Wakely L, Rahman R, Stephenson J. A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes. Brit J Ophthalmol. 2012;96:1003–7.
Hikichi T, Yoshida A, Akiba J, Trempe CL. Natural outcomes of stage-1, stage-2, stage-3, and stage-4 idiopathic macular holes. Brit J Ophthalmol. 1995;79:517–20.
Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995;119:752–9.
Benson WE, Cruickshanks KC, Fong DS, Williams GA, Bloome MA, Frambach DA, et al. Surgical management of macular holes: a report by the American Academy of Ophthalmology. Ophthalmology. 2001;108:1328–35.
Steel DH, Lotery AJ. Idiopathic vitreomacular traction and macular hole: a comprehensive review of pathophysiology, diagnosis, and treatment. Eye (Lond). 2013;27(Suppl 1):1–21.
Venkatesh R, Mohan A, Sinha S, Aseem A, Yadav NK. Newer indices for predicting macular hole closure in idiopathic macular holes: a retrospective, comparative study. Indian J Ophthalmol. 2019;67:1857–62.
Bringmann A, Unterlauft JD, Barth T, Wiedemann R, Rehak M, Wiedemann P. Different modes of full-thickness macular hole formation. Exp Eye Res. 2021;202: 108393.
Spaide RF, Wong D, Fisher Y, Goldbaum M. Correlation of vitreous attachment and foveal deformation in early macular hole states. Am J Ophthalmol. 2002;133:226–9.
Takahashi A, Yoshida A, Nagaoka T, Takamiya A, Sato E, Kagokawa H, et al. Idiopathic full-thickness macular holes and the vitreomacular interface: a high-resolution spectral-domain optical coherence tomography study. Am J Ophthalmol. 2012;154:881-892e2.
Niwa H, Terasaki H, Ito Y, Miyake Y. Macular hole development in fellow eyes of patients with unilateral macular hole. Am J Ophthalmol. 2005;140:370–5.
Tanner V, Chauhan DS, Jackson TL, Williamson TH. Optical coherence tomography of the vitreoretinal interface in macular hole formation. Br J Ophthalmol. 2001;85:1092–7.
Haouchine B, Massin P, Gaudric A. Foveal pseudocyst as the first step in macular hole formation - a prospective study by optical coherence tomography. Ophthalmology. 2001;108:15–22.
Gaudric A, Haouchine B, Massin P, Paques M, Blain P, Erginay A. Macular hole formation: new data provided by optical coherence tomography. Arch Ophthalmol. 1999;117:744–51.
Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Arch Ophthalmol. 1988;106:629–39.
Bainbridge J, Herbert E, Gregor Z. Macular holes: vitreoretinal relationships and surgical approaches. Eye (Lond). 2008;22:1301–9.
Chen Q, Liu ZX. Idiopathic macular hole: a comprehensive review of its pathogenesis and of advanced studies on metamorphopsia. J Ophthalmol. 2019;2019:7294952.
Woon WH, Greig D, Savage MD, Wilson MC, Grant CA, Mokete B, et al. Movement of the inner retina complex during the development of primary full-thickness macular holes: implications for hypotheses of pathogenesis. Graefes Arch Clin Exp Ophthalmol. 2015;253:2103–9.
Ito Y, Terasaki H, Suzuki T, Kojima T, Mori M, Ishikawa K, et al. Mapping posterior vitreous detachment by optical coherence tomography in eyes with idiopathic macular hole. Am J Ophthalmol. 2003;135:351–5.
Uwaydat SH, Mansour A, Ascaso FJ, Parodi MB, Foster R, Smiddy WE, et al. Clinical characteristics of full thickness macular holes that closed without surgery. Brit J Ophthalmol. 2021;106:1463–8.
Mansour HA, Uwaydat SH, Parodi M, Jurgens I, Smiddy W, Ellabban AA, et al. Recovery course of foveal microstructure in the nonsurgical resolution of full-thickness macular hole. Graefes Arch Clin Exp Ophthalmol. 2022;260:3403.
Funding
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF-2020R1F1A1074898). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Statistical consultation was supported by the Department of Biostatistics of the Catholic Research Coordinating Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
J. Y. Kim, None; R. Y. Kim, None; M. Kim, None; Y. G. Park, None; H. W. Yim, None; Y. H. Park, None.
Previous posting
This manuscript was posted as a preprint on Research Square on 29 Dec, 2022. https://doi.org/10.21203/rs.3.rs-2389966/v1.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Young-Hoon Park
About this article
Cite this article
Kim, J.Y., Kim, R.Y., Kim, M. et al. Analysis of the progression rate of idiopathic macular holes and the optimal cut-off for baseline minimum linear diameter and base diameter. Jpn J Ophthalmol 68, 96–104 (2024). https://doi.org/10.1007/s10384-023-01044-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-023-01044-0