Abstract
Timely treatment is essential in the management of glaucoma. However, subjective assessment of visual field (VF) progression is not recommended, because it can be unreliable. There are two types of artificial intelligence (AI) strong and weak (machine learning). Weak AIs can perform specific tasks. Linear regression is a method of weak AI. Using linear regression in the real-world clinic has enabled analyzing and predicting VF progression. However, caution is still required when interpreting the results, because whenever the number of VF data sets investigated is small, the predictions can be inaccurate. Several other non-ordinal, or modern AI methods have been constructed to improve prediction accuracy, such as clustering and more modern AI methods of Analysis with Non-Stationary Weibull Error Regression and Spatial Enhancement (ANSWERS), Variational Bayes Linear Regression (VBLR), Kalman Filter and sparse modeling (The least absolute shrinkage and selection operator regression: Lasso). It is also possible to improve the prediction performance using retinal thickness measured with optical coherence tomography by using machine learning methods, such as multitask learning.










Similar content being viewed by others
References
Scerri M, Grech V. Artificial intelligence in medicine. Early Hum Dev. 2020;145:105017.
Jampel HD. Target pressure in glaucoma therapy. J Glaucoma. 1997;6:133–8.
Clement CI, Bhartiya S, Shaarawy T. New perspectives on target intraocular pressure. Surv Ophthalmol. 2014;59:615–26.
The Japan Glaucoma Society. The Japan Glaucoma Society Guidelines for Glaucoma (5th edition). Nippon Ganka Gakkai Zasshi. 2022;126:85–177.
Kiuchi Y, Inoue T, Shoji N, Nakamura M, Tanito M. Glaucoma Guideline Preparation Committee, Japan Glaucoma Society. The Japan Glaucoma Society Guidelines for glaucoma. Jpn J Ophthalmol. 2023;67:189–254.
Viswanathan AC, Crabb DP, McNaught AI, Westcott MC, Kamal D, Garway-Heath DF, et al. Interobserver agreement on visual field progression in glaucoma: a comparison of methods. Br J Ophthalmol. 2003;87:726–30.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Tanna AP, Budenz DL, Bandi J, Feuer WJ, Feldman RM, Herndon LW, et al. Glaucoma progression analysis software compared with expert consensus opinion in the detection of visual field progression in glaucoma. Ophthalmology. 2012;119:468–73.
Anton A, Pazos M, Martin B, Navero JM, Ayala ME, Castany M, et al. Glaucoma progression detection: agreement, sensitivity, and specificity of expert visual field evaluation, event analysis, and trend analysis. Eur J Ophthalmol. 2013;23:187–95.
Diaz-Aleman VT, Anton A, de la Rosa MG, Johnson ZK, McLeod S, Azuara-Blanco A. Detection of visual-field deterioration by Glaucoma progression analysis and threshold Noiseless Trend programs. Br J Ophthalmol. 2009;93:322–8.
Birch MK, Wishart PK, O’Donnell NP. Determining progressive visual field loss in serial Humphrey visual fields. Ophthalmology. 1995;102:1227–34. discussion 34 – 5.
Roberti G, Michelessi M, Tanga L, Belfonte L, Del Grande LM, Bruno M et al. Glaucoma progression diagnosis: the Agreement between Clinical Judgment and Statistical Software. J Clin Med 2022;11(19):5508
Fitzke FW, Hitchings RA, Poinoosawmy D, McNaught AI, Crabb DP. Analysis of visual field progression in glaucoma. Br J Ophthalmol. 1996;80:40–8.
Viswanathan AC, Fitzke FW, Hitchings RA. Early detection of visual field progression in glaucoma: a comparison of PROGRESSOR and STATPAC 2. Br J Ophthalmol. 1997;81:1037–42.
Smith SD, Katz J, Quigley HA. Analysis of progressive change in automated visual fields in glaucoma. Invest Ophthalmol Vis Sci. 1996;37:1419–28.
Nouri-Mahdavi K, Brigatti L, Weitzman M, Caprioli J. Comparison of methods to detect visual field progression in glaucoma. Ophthalmology. 1997;104:1228–36.
Mayama C, Araie M, Suzuki Y, Ishida K, Yamamoto T, Kitazawa Y, et al. Statistical evaluation of the diagnostic accuracy of methods used to determine the progression of visual field defects in glaucoma. Ophthalmology. 2004;111:2117–25.
Katz J, Sommer A, Gaasterland DE, Anderson DR. Comparison of analytic algorithms for detecting glaucomatous visual field loss. Arch Ophthalmol. 1991;109:1684–9.
Mandava S, Zulauf M, Zeyen T, Caprioli J. An evaluation of clusters in the glaucomatous visual field. Am J Ophthalmol. 1993;116:684–91.
Gardiner SK, Crabb DP. Examination of different pointwise linear regression methods for determining visual field progression. Invest Ophthalmol Vis Sci. 2002;43:1400–7.
Gardiner SK, Crabb DP, Fitzke FW, Hitchings RA. Reducing noise in suspected glaucomatous visual fields by using a new spatial filter. Vis Res. 2004;44:839–48.
Strouthidis NG, Scott A, Viswanathan AC, Crabb DP, Garway-Heath DF. Monitoring glaucomatous visual field progression: the effect of a novel spatial filter. Invest Ophthalmol Vis Sci. 2007;48:251–7.
Chen A, Nouri-Mahdavi K, Otarola FJ, Yu F, Afifi AA, Caprioli J. Models of glaucomatous visual field loss. Invest Ophthalmol Vis Sci. 2014;55:7881–7.
Araie M. Basic and clinical studies of pressure-independent damaging factors of open angle glaucoma. Nippon Ganka Gakkai zasshi. 2011;115:213–36.
Caprioli J, de Leon JM, Azarbod P, Chen A, Morales E, Nouri-Mahdavi K, et al. Trabeculectomy can improve long-term visual function in Glaucoma. Ophthalmology. 2016;123:117–28.
Taketani Y, Murata H, Fujino Y, Mayama C, Asaoka R. How many visual Fields are required to precisely predict future test results in Glaucoma patients when using different Trend analyses? Invest Ophthalmol Vis Sci. 2015;56:4076–82.
Bryan SR, Vermeer KA, Eilers PH, Lemij HG, Lesaffre EM. Robust and censored modeling and prediction of progression in glaucomatous visual fields. Invest Ophthalmol Vis Sci. 2013;54:6694–700.
Omoto T, Asaoka R, Akagi T, Oishi A, Miyata M, Murata H, et al. The number of examinations required for the accurate prediction of the progression of the central 10-degree visual field test in glaucoma. Sci Rep. 2022;12:18843.
Flammer J, Drance SM, Fankhauser F, Augustiny L. Differential light threshold in automated static perimetry. Factors influencing short-term fluctuation. Arch Ophthalmol. 1984;102:876–9.
Flammer J, Drance SM, Zulauf M. Differential light threshold. Short- and long-term fluctuation in patients with glaucoma, normal controls, and patients with suspected glaucoma. Arch Ophthalmol. 1984;102:704–6.
Bengtsson B, Heijl A. False-negative responses in glaucoma perimetry: indicators of patient performance or test reliability? Invest Ophthalmol Vis Sci. 2000;41:2201–4.
Henson DB, Evans J, Chauhan BC, Lane C. Influence of fixation accuracy on threshold variability in patients with open angle glaucoma. Invest Ophthalmol Vis Sci. 1996;37:444–50.
Artes PH. Progression: things we need to remember but often forget to think about. Optom Vis Sci. 2008;85:380–5.
Krakau CE. A statistical trap in the evaluation of visual field decay. Acta Ophthalmol Suppl. 1985;173:19–21.
Holmin C, Krakau CE. Regression analysis of the central visual field in chronic glaucoma cases. A follow-up study using automatic perimetry. Acta Ophthalmol (Copenh). 1982;60:267–74.
Spry PG, Bates AB, Johnson CA, Chauhan BC. Simulation of longitudinal threshold visual field data. Invest Ophthalmol Vis Sci. 2000;41:2192–200.
Asman P, Heijl A. Arcuate cluster analysis in glaucoma perimetry. J Glaucoma. 1993;2:13–20.
Chauhan BC, Drance SM, Lai C. A cluster analysis for threshold perimetry. Graefes Arch Clin Exp Ophthalmol. 1989;227:216–20.
Suzuki Y, Araie M, Ohashi Y. Sectorization of the central 30 degrees visual field in glaucoma. Ophthalmology. 1993;100:69–75.
Nouri-Mahdavi K, Mock D, Hosseini H, Bitrian E, Yu F, Afifi A, et al. Pointwise rates of visual field progression cluster according to retinal nerve fiber layer bundles. Invest Ophthalmol Vis Sci. 2012;53:2390–4.
Hirasawa K, Murata H, Hirasawa H, Mayama C, Asaoka R. Clustering visual field test points based on rates of progression to improve the prediction of future damage. Invest Ophthalmol Vis Sci. 2014;55:7681–5.
Hirasawa K, Murata H, Asaoka R. Revalidating the usefulness of a “Sector-Wise Regression” Approach to predict glaucomatous visual function progression. Invest Ophthalmol Vis Sci. 2015;56:4332–5.
Van der Laan MJ, Pollard KS. A new algorithm for hybrid hierarchical clustering with visualization and the bootstrap. J Stat Plan Inference. 2003;117:275–303.
Rousseeuw PJ, Silhouettes. A graphical aid to the interpretation and validation of cluster analysis. J Comput Appl Math. 1987;20:53–65.
Pollard KS, Van der Laan MJ. A method to identify significant clusters in gene expression data. Proc SCI 2002. 2002;2:318–25.
Garway-Heath DF, Poinoosawmy D, Fitzke FW, Hitchings RA. Mapping the visual field to the optic disc in normal tension glaucoma eyes. Ophthalmology. 2000;107:1809–15.
Weber J, Dannheim F, Dannheim D. The topographical relationship between optic disc and visual field in glaucoma. Acta Ophthalmol (Copenh). 1990;68:568–74.
Asman P, Heijl A. Glaucoma hemifield test. Automated visual field evaluation. Arch Ophthalmol. 1992;110:812–9.
Rokach L, Maimon O. Chapter 15: clustering methods. In: Maimon O, Rokach L, editors. Data Mining and Knowledge Discovery Handbook. Boston, MA: Springer; 2005. pp. 325–52.
Omoto T, Murata H, Fujino Y, Matsuura M, Yamashita T, Miki A, et al. Validating the usefulness of sectorwise regression of visual field in the central 10 degrees. Br J Ophthalmol. 2022;106:497–501.
White HA. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;48:817–38.
Crabb DP, Russell RA, Malik R, Anand N, Baker H, Boodhna T, et al. editors. Frequency of visual field testing when monitoring patients newly diagnosed with glaucoma: mixed methods and modelling. Southampton (UK): NIHR Journals Library; 2014.
Zeyen TG, Zulauf M, Caprioli J. Priority of test locations for automated perimetry in glaucoma. Ophthalmology. 1993;100:518–22.
Suzuki Y, Kitazawa Y, Araie M, Yamagami J, Yamamoto T, Ishida K, et al. Mathematical and optimal clustering of test points of the central 30-degree visual field of glaucoma. J Glaucoma. 2001;10:121–8.
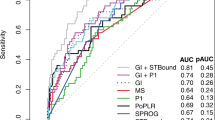
Zhu H, Russell RA, Saunders LJ, Ceccon S, Garway-Heath DF, Crabb DP. Detecting changes in retinal function: analysis with Non-Stationary Weibull Error regression and spatial enhancement (ANSWERS). PLoS ONE. 2014;9:e85654.
O’Leary N, Chauhan BC, Artes PH. Visual field progression in glaucoma: estimating the overall significance of deterioration with permutation analyses of pointwise linear regression (PoPLR). Invest Ophthalmol Vis Sci. 2012;53:6776–84.
Garway-Heath DF, Lascaratos G, Bunce C, Crabb DP, Russell RA, Shah A, et al. The United Kingdom Glaucoma treatment study: a multicenter, randomized, placebo-controlled clinical trial: design and methodology. Ophthalmology. 2013;120:68–76.
Garway-Heath DF, Crabb DP, Bunce C, Lascaratos G, Amalfitano F, Anand N, et al. Latanoprost for open-angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. Lancet. 2015;385:1295–304.
Zhu H, Crabb DP, Ho T, Garway-Heath DF. More Accurate modeling of visual field progression in Glaucoma: ANSWERS. Invest Ophthalmol Vis Sci. 2015;56:6077–83.
Murata H, Araie M, Asaoka R. A new approach to measure visual field progression in glaucoma patients using variational bayes linear regression. Invest Ophthalmol Vis Sci. 2014;55:8386–92.
Murata H, Zangwill LM, Fujino Y, Matsuura M, Miki A, Hirasawa K, et al. Validating Variational Bayes Linear Regression Method with Multi-Central Datasets. Invest Ophthalmol Vis Sci. 2018;59:1897–904.
Bengtsson B, Olsson J, Heijl A, Rootzen H. A new generation of algorithms for computerized threshold perimetry, SITA. Acta Ophthalmol Scand. 1997;75:368–75.
Murata H, Asaoka R, Fujino Y, Matsuura M, Hirasawa K, Shimada S, et al. Comparing the usefulness of a new algorithm to measure visual field using the variational Bayes linear regression in glaucoma patients, in comparison to the swedish interactive thresholding algorithm. Br J Ophthalmol. 2022;106:660–6.
Hirasawa K, Murata H, Shimada S, Matsuno M, Shoji N, Asaoka R. Faster algorithms to measure visual field using the variational Bayes linear regression model in glaucoma: comparison with SITA-Fast. Br J Ophthalmol. 2022. https://doi.org/10.1136/bjophthalmol-2021-320523.
Lefferts EJ, Markley FL, Shuster MD. Kalman Filtering for Spacecraft attitude estimation. J Guid Control Dyn. 1982;5:417–29.
Kalman RE. A New Approach to Linear filtering and prediction problems. J Basic Eng. 1960;82:35–45.
Catlin DE. The Discrete Kalman Filter. Estimation, control, and the Discrete Kalman Filter. 71st ed. Springer Science & Business Media; 2012:133–63.
Ederer F, Gaasterland DE, Sullivan EK, Investigators A. The advanced Glaucoma intervention study (AGIS): 1. Study design and methods and baseline characteristics of study patients. Control Clin Trials. 1994;15:299–325.
Musch DC, Lichter PR, Guire KE, Standardi CL. The collaborative initial Glaucoma treatment study: study design, methods, and baseline characteristics of enrolled patients. Ophthalmology. 1999;106:653–62.
Musch DC, Gillespie BW, Lichter PR, Niziol LM, Janz NK, Investigators CS. Visual field progression in the collaborative initial Glaucoma treatment study the impact of treatment and other baseline factors. Ophthalmology. 2009;116:200–7.
Garcia GP, Nitta K, Lavieri MS, Andrews C, Liu X, Lobaza E, et al. Using Kalman Filtering to Forecast Disease Trajectory for patients with normal tension Glaucoma. Am J Ophthalmol. 2019;199:111–9.
Kingma DP, Welling M. Auto-Encoding Variational Bayes. Preprint. Posted online Dec 20, 2013. arXiv:13126114 [cs, stat]. doi: https://doi.org/10.48550/arXiv.1312.6114.
Rezende DJ, Mohamed S, Wierstra D. Stochastic Backpropagation and Approximate Inference in Deep Generative Models. Preprint. Posted online Jan 16, 2014. arXiv:14014082 [cs, stat]. https://doi.org/10.48550/arXiv.1401.4082.
Aggarwal CC. Neural networks and deep learning: a Textbook. Springer; 2018. p. 207–13.
Shaojie C, Meng Z, Zhao Q, Electrocardiogram recognization based on variational AutoEncoder. In: Machine learning and biometrics. IntechOpen; 2018
Asaoka R, Murata H, Matsuura M, Fujino Y, Yanagisawa M, Yamashita T. Improving structure-function relationship in glaucomatous visual fields by using a deep learning-based noise reduction approach. Ophthalmol Glaucoma. 2020;3:210–7.
Asaoka R, Murata H, Asano S, Matsuura M, Fujino Y, Miki A, et al. The usefulness of the deep learning method of variational autoencoder to reduce measurement noise in glaucomatous visual fields. Sci Rep. 2020;10:7893.
Berchuck SI, Mukherjee S, Medeiros FA. Estimating Rates of Progression and Predicting Future Visual Fields in Glaucoma using a deep Variational Autoencoder. Sci Rep. 2019;9:18113.
Tibshirani R. Regression shrinkage and selection via the lasso. J R Stat Soc Series B Methodological. 1996;58:267–88.
Friedman J, Hastie T, Tibshirani R. Regularization Paths for generalized Linear Models via Coordinate Descent. J Stat Softw. 2010;33:1–22.
Fujino Y, Murata H, Mayama C, Asaoka R. Applying “Lasso” regression to predict future visual field progression in Glaucoma patients. Invest Ophthalmol Vis Sci. 2015;56:2334–9.
Asaoka R. Measuring visual field progression in the central 10 degrees using additional information from central 24 degrees visual fields and ‘lasso regression’. PLoS ONE. 2013;8:e72199.
Weinreb RN, Khaw PT. Primary open-angle glaucoma. Lancet. 2004;363:1711–20.
Fechtner RD, Weinreb RN. Mechanisms of optic nerve damage in primary open angle glaucoma. Surv Ophthalmol. 1994;39:23–42.
Chauhan BC, Nicolela MT, Artes PH. Incidence and rates of visual field progression after longitudinally measured optic disc change in glaucoma. Ophthalmology. 2009;116:2110–8.
Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN. Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol. 2009;127:1250–6.
Miki A, Medeiros FA, Weinreb RN, Jain S, He F, Sharpsten L, et al. Rates of retinal nerve fiber layer thinning in glaucoma suspect eyes. Ophthalmology. 2014;121:1350–8.
Wadhwani M, Bali SJ, Satyapal R, Angmo D, Sharma R, Pandey V, et al. Test-retest variability of retinal nerve fiber layer thickness and macular ganglion cell-inner plexiform layer thickness measurements using spectral-domain optical coherence tomography. J Glaucoma. 2015;24:e109–15.
Francoz M, Fenolland JR, Giraud JM, El Chehab H, Sendon D, May F, et al. Reproducibility of macular ganglion cell-inner plexiform layer thickness measurement with cirrus HD-OCT in normal, hypertensive and glaucomatous eyes. Br J Ophthalmol. 2014;98:322–8.
Mwanza JC, Oakley JD, Budenz DL, Chang RT, Knight OJ, Feuer WJ. Macular ganglion cell-inner plexiform layer: automated detection and thickness reproducibility with spectral domain-optical coherence tomography in glaucoma. Invest Ophthalmol Vis Sci. 2011;52:8323–9.
Ghasia FF, El-Dairi M, Freedman SF, Rajani A, Asrani S. Reproducibility of spectral-domain optical coherence tomography measurements in adult and pediatric glaucoma. J Glaucoma. 2015;24:55–63.
Garway-Heath DF, Zhu H, Cheng Q, Morgan K, Frost C, Crabb DP, et al. Combining optical coherence tomography with visual field data to rapidly detect disease progression in glaucoma: a diagnostic accuracy study. Health Technol Assess. 2018;22:1–106.
Zheng Y, Xu L, Kiwaki T, Wang J, Murata H, Asaoka R et al. Glaucoma Progression Prediction Using Retinal Thickness via Latent Space Linear Regression. In: Proceedings of the 25th ACM SIGKDD International Conference on Knowledge Discovery and Data Mining (KDD). 2019: 2278-86.
Zhang Y, Yang Q. A survey on multi-task learning. Natl Sci Rev. 2018;5:30–43.
Ruder R. An overview of multi-task learning in deep neural networks. Preprint. Posted online Jun 15, 2017. arXiv:1706.05098. doi: https://doi.org/10.48550/arXiv.1706.05098.
Hashimoto Y, Asaoka R, Kiwaki T, Sugiura H, Asano S, Murata H, et al. Deep learning model to predict visual field in central 10 degrees from optical coherence tomography measurement in glaucoma. Br J Ophthalmol. 2021;105:507–13.
Hashimoto Y, Kiwaki T, Sugiura H, Asano S, Murata H, Fujino Y, et al. Predicting 10 – 2 visual field from optical coherence tomography in Glaucoma using deep learning corrected with 24 – 2/30 – 2 visual field. Transl Vis Sci Technol. 2021;10:28.
Xu L, Asaoka R, Kiwaki T, Murata H, Fujino Y, Matsuura M, et al. Predicting the Glaucomatous Central 10-Degree Visual Field from Optical Coherence Tomography using Deep Learning and Tensor Regression. Am J Ophthalmol. 2020;218:304–13.
Asano S, Asaoka R, Murata H, Hashimoto Y, Miki A, Mori K, et al. Predicting the central 10 degrees visual field in glaucoma by applying a deep learning algorithm to optical coherence tomography images. Sci Rep. 2021;11:2214.
Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res. 2007;26:688–710.
Asaoka R, Xu L, Murata H, Kiwaki T, Matsuura M, Fujino Y, et al. A joint Multitask Learning Model for cross-sectional and longitudinal predictions of Visual Field using OCT. Ophthalmol Sci. 2021;1:100055.
Detry-Morel M, Jamart J, Hautenauven F, Pourjavan S. Comparison of the corneal biomechanical properties with the Ocular Response Analyzer(R) (ORA) in african and caucasian normal subjects and patients with glaucoma. Acta Ophthalmol. 2012;90:e118–24.
Susanna CN, Diniz-Filho A, Daga FB, Susanna BN, Zhu F, Ogata NG, et al. A prospective longitudinal study to investigate corneal hysteresis as a risk factor for Predicting Development of Glaucoma. Am J Ophthalmol. 2018;187:148–52.
Hirasawa K, Matsuura M, Murata H, Nakakura S, Nakao Y, Kiuchi Y, et al. Association between corneal Biomechanical Properties with Ocular Response Analyzer and also CorvisST Tonometry, and Glaucomatous Visual Field Severity. Transl Vis Sci Technol. 2017;6:18.
Medeiros FA, Meira-Freitas D, Lisboa R, Kuang TM, Zangwill LM, Weinreb RN. Corneal hysteresis as a risk factor for glaucoma progression: a prospective longitudinal study. Ophthalmology. 2013;120:1533–40.
De Moraes CV, Hill V, Tello C, Liebmann JM, Ritch R. Lower corneal hysteresis is associated with more rapid glaucomatous visual field progression. J Glaucoma. 2012;21:209–13.
Matsuura M, Hirasawa K, Murata H, Nakakura S, Kiuchi Y, Asaoka R. The usefulness of CorvisST Tonometry and the Ocular Response Analyzer to assess the progression of glaucoma. Sci Rep. 2017;7:40798.
Wolpert DH, Macready WG. No free lunch theorems for optimization. IEEE Trans Evol Comput. 1997;1:67.
Funding
Grants (nos. 19H01114: RA, 18KK0253: RA, 20K09784: RA, and 80635748: HM) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and the Translational Research Program; Strategic Promotion for practical application of Innovative medical Technology (TR-SPRINT) from the Japan Agency for Medical Research and Development (AMED) (RA), and the Japan Glaucoma Society Research Project Support Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
R. Asaoka, None; H. Murata, None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Organizer: Tetsuya Yamamoto, MD
Corresponding author: Ryo Asaoka
About this article
Cite this article
Asaoka, R., Murata, H. Prediction of visual field progression in glaucoma: existing methods and artificial intelligence. Jpn J Ophthalmol 67, 546–559 (2023). https://doi.org/10.1007/s10384-023-01009-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-023-01009-3