Abstract
Purpose
To evaluate the effects of lowering intraocular pressure (IOP) on foveal avascular zone (FAZ), peripapillary and macular vessel density (VD) by optical coherence tomography angiography (OCTA) in patients with open angle glaucoma after trabeculectomy.
Study design
Prospective study
Methods
Twenty eyes of 20 patients with primary open angle glaucoma (POAG) or exfoliation glaucoma (EG) who were followed up to six months and underwent trabeculectomy were included in our study. OCTA, AngioVue (Optovue Inc.) software was used to analyse the FAZ, peripapillary VD, macular superficial capillary plexus (SCP) and deep capillary plexus (DCP) VD. The parameters of the preoperative and postoperative controls were compared statistically.
Results
Twelve of the patients (60%) had POAG and eight (40%) had EG. Mean IOP measured was 22.4±2.4 mmHg preoperatively and 14.9±2.4 mmHg in the postoperative sixth month (p <0.001). There were no significant changes in OCTA optic disc and macular SCP VD values at the end of the sixth month. In macular DCP parameters; whole image VD (WI-VD), foveal VD (F-VD), parafoveal VD (PAF-VD) and perifoveal VD (PEF-VD) values increased statistically (p=0.003; p=0.026; p=0.006; p=0.004). There was a statistically significant decrease in FAZ area (FAZ-A) and FAZ perimeter (FAZ-P); and a significant increase was found in foveal density values (FD) (p=0.026; p=0.049; p=0.005).
Conclusions
We found that reducing IOP by trabeculectomy did not affect the microcirculation of the peripapillary region and macular SCP, while there was a significant increase in the DCP parameters of the macular region.
Similar content being viewed by others
Introductıon
Glaucoma is an optic neuropathy characterized by progressive optic nerve damage and visual field loss due to the degeneration of retinal ganglion cell (RGC) axons [1]. Although the most important risk factor for glaucoma is high intraocular pressure (IOP), many other factors are involved in etiopathogenesis [2]. Different mechanisms may play a role in the pathophysiology. It is thought that mechanical stress, vascular dysregulation, immunological factors, excitotoxicity and oxidative stress may affect the development of glaucomatous optic neuropathy by causing RGC damage [3].
In the literature, studies performed with different imaging techniques, show that the optic nerve, retina and choroid perfusion parameters of glaucomatous eyes decrease compared to normal eyes [4,5,6]. Since ocular perfusion changes may be either a cause or result of the disease; many studies have examined the effect of IOP changes on ocular perfusion. With a decrease in IOP, improvements in optic nerve head (ONH), retrobulbar vascular structures and choroidal perfusion have been shown [7, 8].
In recent years, Optical Coherence Tomography Angiography (OCTA) imaging techniques have been used in the diagnosis and follow-up of glaucoma to examine vascular changes noninvasively. In studies conducted with OCTA, it has been shown that peripapillary and macular vascular density (VD) values of glaucomatous eyes decrease compared to normal eyes [9, 10]. In more recent studies, the effects of a medical or surgical reduction in IOP on peripapillary and macular VD values have been investigated. It is shown that ONH, retrobulbar vascular structures and choroidal perfusion improved with IOP reduction [7, 8].
Currently, trabeculectomy seems to be the most effective surgical procedure for reducing IOP in patients with open-angle glaucoma [11]. In this study, we followed patients with moderate-level primary open-angle glaucoma (POAG) and exfoliation glaucoma (EG) in whom IOP reduction was achieved by trabeculectomy surgery for six months. We aimed to evaluate the changes in the vascular structure of the optic disc and macula using OCTA, with the decrease in IOP observed in these patients in preoperative and postoperative period.
Although there are similar studies in the literature, they report very few and some controversial results. We wanted to see the effects of surgery in patients with moderate glaucoma. We targeted a larger number of patients but due to the limitations brought about by covid 19 were unable to recruit our target numbers.
Materıal and methods
Ethics committee approval for this prospective study was obtained from Manisa Celal Bayar University (MCBU) Faculty of Medicine Scientific Research Ethics Committee (registration number 20,478,486). This research was conducted as a thesis study in accordance with the principles of the Declaration of Helsinki.
Our study was initially planned to recruit 30 patients, but only 23 patients were evaluated. Finally, 20 eyes were evaluated and 3 cases were excluded due to poor quality of OCTA images. Twenty eyes of 20 patients who underwent trabeculectomy with a diagnosis of open angle glaucoma between January 2019-July 2020 were finally included in our study.
The inclusion criteria for the patients in the study were : open angle in gonioscopic examination, thinning or notching of the neuroretinal rim as signs of glaucomatous optic nerve damage, thinning of the retinal nerve fiber layer (RNFL) in optical coherence tomography (OCT) examination, and glaucoma in the individual without other coexistent ocular disease that may cause moderate visual field (VF) defects. Glaucomatous visual field defects we defined as two or more of the following findings: Glaucoma hemi-field test results outside normal limits; the presence of three points at the level of P <5% and one P <1% in pattern deviation plots; and PSD value of P <5%. VF defects were confirmed by two consecutive reliable tests with a loss of fixation< 20%, in addition to false positive and false negative error rate < 5%. The patients had moderate glaucoma damage. Patients with end-stage glaucoma with VF-MD values above 12 dB and with a cup / disc ratio of 0.9 or total atrophy on examination were not included, as we thought severe neural tissue damage and vessel loss due to end stage glaucoma would interfere our results.
Patients with progressive glaucomatous optic nerve damage or VF defects were offered trabeculectomy when target IOP reduction could not be achieved despite maximum tolerable medical therapy or to give a better chance to preserve vision for bilateral progressive disease.
Systemic diseases of the patients were investigated, and systemic blood pressure measurements were made in all preoperative and postoperative controls. During the follow-up period of our study, the systemic blood pressures of 5 patients (25%) with a diagnosis of systemic hypertension were monitored under medical treatment. A history of ocular surgery other than uncomplicated cataract surgery, dense cataracts which preclude good quality imaging, vitreous opacity, corneal pathology that reduced the imaging quality were not included.
Patients with retinal vascular diseases like diabetes, retinal vein occlusions that may cause false results in OCT and OCTA measurements in the macular and peripapillary area were not included in the study group.
Patients with refractive values more than spherical ± 3.00 diopters or cylindrical ± 2.00 diopters, patients with complications, hypotonia, and IOP below 10 mmHg during or after the operation were not included in the study.
The measurements were performed at four different time points: preoperatively, and at the 1st, 3rd and 6th months after surgery. Best corrected visual acuity (BCVA) examination on Snellen chart, IOP measurements by Goldmann applanation tonometer, iridocorneal angle examinations by Goldmann three mirror lens, biomicroscopy and dilated fundus examinations were performed. All measurements were performed between 08.30-10.30 hours in the morning.
Retinal nerve fiber layer thickness (RNFLT) and ganglion cell analysis (GCA) examinations with OCT (Carl Zeiss Meditec), VF examination (Humphrey Field analyzer with Swedish Interactive Threshold Algorithm standard 24-2 test; Carl Zeiss Meditec); optic disc and macula OCTA (AngioVue; Optovue Inc.) imaging were performed. The use of anti-glaucomatous drugs and current systemic diseases of the patients before and after trabeculectomy were recorded. The patients' current topical antiglaucomatous treatments were stopped after surgery.
Optical coherence tomography angiography measurements
In this study, we used the Avanti RTVue-XR with the AngioVue software (version 2018.0.0.14; Optavue, Inc.) OCTA device using the SSADA algorithm. Two OCTA volume scans were taken horizontally and vertically to avoid motion artifacts and fixation changes. Vessel density(VD) was measured using the automated density measure tool in the AngioVue Software.
Retinal and choroidal images were taken with the enhanced HD line module with 6X6 mm macula and 4.5X4.5 mm disc OCTA. The AngioVue (RTVue-XR) OCTA device calculates VD measurements by automatically dividing the images it receives from the optic disc into previously defined regions. In the peripapillary region, images are automatically segmented by the OCTA device for the evaluation of RPCP.
The macula scans were automatically segmented into two layers as superficial capillary plexus (SCP) and deep capillary plexus (DCP). The FAZ was automatically mapped by the software. Its surface area was measured in terms of mm2’s and its perimeter in mm’s. Images obtained were checked for quality (Signal Strength more than 6/10), as well as absence of artifacts.
Statistical analysis
SPSS 24 (SPSS Inc.) package program was used for statistical analysis. Numerical data is presented as mean ± standard deviation, unless otherwise noted; categorical data were expressed as numbers (%). Categorical variables were compared using the Chi-Square test. The compatibility of numerical variables to normal distribution was evaluated by Kolmogorov-Smirnov test. Independent Sample T test was used to compare independent groups in normal distribution, and Mann-Whitney U test was used for non-parametric comparisons. Friedman analysis was performed to compare the repeated measurements. Wilcoxon-Sign test with Bonferroni correction was used for pairwise comparisons. The correlation between variables was analyzed using Spearman's test. p <0.05 was considered significant.
Results
In our study, 20 eyes of 20 patients who underwent trabeculectomy with a diagnosis of open angle glaucoma were evaluated. The demographic characteristics of the patients are shown in Table 1.
BCVA in Snellen equalant and VF-MD and PSD values are shown in Table 2. While a statistically significant decrease was observed in BCVA and PSD, a statistically significant increase was observed in VF-MD values during the preoperative period to postoperative 6th month follow-up (p <0.001; p = 0.021,p = 0.039).
The mean IOP values were 22.4 ± 2.4 with medication in the preoperative IOP measurements and 13.1 ± 2.5; 14.4 ± 1.7, 14.9 ± 2.4 mmHg without glaucoma medication at postoperative 1st, 3rd and 6th months, respectively (Table 3). In the post-trabeculectomy follow-up of the patients, a statistically significant decrease of IOP values were observed at all timepoints (p <0.001).
Average and four quadrant RNFLT values measured with OCT during our follow-up, with cup / disc ratio and minimum and average GCA values are shown in Table 4. No statistically significant changes were observed in the postoperative period in the mean and four quadrant RNFLT values, cup / disc ratio, and minimum and mean GCA values (p> 0.05).
All images taken from OCTA and optic disc RPCP imaging of our patients are whole image peripapillary VD (WIP-VD), peripapillary VD (P-VD), intradisc VD (ID-VD), nasal peripapillary VD (NP-VD), superior peripapillary VD (SP-VD), inferior peripapillary VD (IP-VD) and temporal peripapillary VD (TP-VD) measurements are shown in Table 5. No statistically significant change was found in any of the optic disc RPCP measurements (p> 0.05).
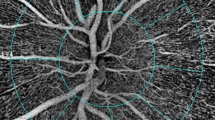
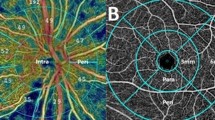
In macular VD measurements with OCTA, all images taken separately from SCP and DCP were macular whole image VD (WI-VD), foveal VD (F-VD), parafoveal VD (PAF-VD), perifoveal VD (PEF-VD) and FAZ area (FAZ-A), FAZ perimeter (FAZ-P) and foveal density (FD) values are shown in Table 6 below. In our study, no statistically significant change was found in any of the macular preoperative and postoperative OCTA measurements, in any of the SCP parameters (p> 0.05). A statistically significant increase was observed in all parameters in DCP measurements (p = 0.003; p = 0.026; p = 0.006; p = 0.004). In Figure 1a and b, the OCTA DCP VD map of one of our patients, which was taken preoperatively and in the sixth postoperative month is shown. FAZ-A and FAZ-P significantly decreased and FD significanty increased (p = 0.026; p = 0.049; p = 0.005). In Figure 2a and b, the OCTA FAZ region map of one of our patients, which was taken preoperatively and in the sixth postoperative month is shown (Table 7).
Optical coherence tomography angiography (OCTA) macula deep capillary plexus (DCP) images. a Preoperative OCTA macula DCP vascular density (VD) map; whole image VD (WI-VD): 40.2 %; foveal VD (F-VD): 25.8 %; parafoveal VD(PAF-VD): 47.3 %; perifoveal VD(PEF-VD):41.0 %. b Postoperative 6th month OCTA macula DCP-VD map; WI-VD: 47.3 %; F-VD: 27.8 %; PAF-VD: 50.6 %; PEF-VD: 48.1 %. OCTA: optical coherence tomography angiography
OCTA foveal avascular zone(FAZ) images. a Preoperative OCTA FAZ area (FAZ-A): 0.234 mm2; FAZ perimeter (FAZ-P): 1.876 mm; foveal density (FD): 46.83 %. b At 6 months control after trabeculectomy OCTA makula FAZ-A: 0.212 mm2; FAZ-P: 1.773 mm; FD: 50.46%. OCTA: optical coherence tomography angiography
Dıscussıon
In studies conducted with different imaging techniques, it is shown that the optic nerve, retina and choroid perfusion parameters of glaucomatous eyes are decreased compared to normal eyes [4,5,6]. Since ocular perfusion changes may be a cause or result of the disease; many studies have examined the effects of IOP changes on ocular perfusion. It is shown that ONH, retrobulbar vascular structures and choroidal perfusion improved with IOP reduction [7, 8].
In recent years, OCTA imaging techniques have been used in the diagnosis and follow-up of glaucoma to examine vascular changes. In studies conducted with OCTA, it is shown that peripapillary and macular VD values of glaucomatous eyes decrease compared to normal eyes [9, 10]. More recent studies have investigated the effect of a medical or surgical IOP reduction on peripapillary and macular VD values.
In our study, no statistically significant changes were observed in the optic disc VD and macular SCP VD parameters together with the decrease in IOP in our preoperative and postoperative follow-ups. This result is consistent with the studies of Zéboulon et al. and Lommatzsch et al. [12, 13].
In their study, Zéboulon et al. compared the peripapillary and macular VD measurements with OCTA in the preoperative and postoperative first month in 21 patients who underwent non-penetrating sclerotomy; they found no statistically significant change in VD values except an increase in the macular inferotemporal region [12].
Lommatzsch et al., followed 19 patients whose IOP decreased by trabeculectomy for six months; compared preoperative and postoperative RNFLT and GCA with OCTA peripapillary and macular VD values. They found no statistically significant change in the parameters they examined [13].
In a study conducted by Hollo et al., IOP values of six patients diagnosed with open angle glaucoma and ocular hypertension were reduced with topical antiglaucomatous therapy; before and after treatment with OCTA, peripapillary VD values were compared. A significant increase in peripapillary VD values was observed in five patients. In the study conducted by Hollo et al., the IOP values of the patients before treatment were between 35-42 mmHg and it was reduced below 18 mmHg with medical treatment [14]. In the study of Lommatzsch et al., the preoperative mean IOP value was 21.0, and it was reduced to 10.3 mmHg by trabeculectomy[13]. Lommatzsch et al., thought that conflicting results between the two studies might be due to the fact that the patients in their study had more advanced glaucoma and also that the topical antiglaucomatous drugs used in the study of Hollo et al., might have affected VD measurements [13, 14].
Shin et al., followed 31 patients with a diagnosis of POAG, whose IOP was reduced with trabeculectomy for three months, and evaluated the effect of OCTA and peripapillary VD values and changes in lamina cribrosa position on microcirculation. In the postoperative third month, they observed a statistically significant increase in peripapillary VD measurements and a significant decrease in the depth of lamina cribrosa. They also show that the decrease in the depth of the lamina kribrosa was associated with changes in peripapillary microcirculation [15].
In their study, Kim et al., followed 56 patients with a diagnosis of POAG who underwent trabeculectomy for three months. In their postoperative follow-up, VD values were measured separately for the prelaminar, lamina cribrosa, peripapillary retina and peripapillary choroid layers with OCTA, and they evaluated the position of the lamina cribrosa with Swept-Source OCT. At the end of the third month, they observed a significant decrease in the depth of lamina cribrosa. In OCTA parameters, they found a significant increase only in VD values in the prelaminar region, but did not observe a significant change in VD values in the peripapillary retina and choroidal region [16].
In contrast to the literature, a statistically significant increase in macular DCP VD values was found in our study. Ocular perfusion pressure increased after filtration surgery in glaucomatous eyes [17].
Ocular perfusion pressure that increased as a result of IOP reduction might have directly affected retinal venules. We thought that this may ultimately lead to an increase in VD values in the DCP layer, where retinal venules are concentrated [18]. It is known that autoregulatory mechanisms also play a role in vascular perfusion of the retina [19]. Impaired autoregulation may be a critical factor in many vascular diseases, including glaucoma [20]. Differences between studies may be due to variations in autoregulation mechanisms. It is clear that more comprehensive studies on this subject are needed.
In the postoperative follow-up in our study, at the end of the sixth month, a statistically significant decrease was observed in FAZ-A (p = 0.026) and FAZ-P values; (p= 0.049). A statistically significant increase was observed in the FD values at the end of the sixth month (p = 0.005). To the best of our knowledge, there is only one study examining changes in FAZ parameters after glaucoma surgery. In that study, Chang et al. followed 40 patients after glaucoma surgery for a year; t examined changes in VD, FAZ parameters and RNFLT values of optic disc and macula with OCTA. In their study, the mean RNFLT values increased in the first postoperative month, returned to baseline values in the third month and then remained stable throughout the follow-up period. Although they detected fluctuations in peripapillary VD values, they did not observe a statistically significant changes. They observed a significant increase in foveal VD values. They observed that there was a significant increase in FAZ-A and FAZ-P values in the first month, then these parameters tended to decrease and returned to baseline values in the twelfth month. In their study, they stated that the expansion of the FAZ area in the first month may be due to postoperative inflammation [21].
Spaide et al. state that SCP terminated farther from the fovea center than DCP and that DCP determined the FAZ limits [22]. The results of our study also suggest that the increase in DCP microcirculation may be related to the decrease in the FAZ region. In our study, it is shown that the FAZ region and DCP may be sensitive to surgically induced IOP reduction.
In recent studies, it is shown that the FAZ area in glaucomatous eyes increased compared to normal eyes [23]. In our study, the preoperative mean FAZ-A value was found to be 0.312 ± 0.099 mm at the upper limit of normal values.
In a study on glaucomatous eyes, the FAZ field was compared in patients with central and peripheral visual field defects. Eyes with central visual field defects have been shown to have a larger FAZ area [24]. In the literature, the parameters of the FAZ region have just begun to be investigated in the field of glaucoma, and there are few studies on this subject. More comprehensive studies are needed to examine the relationship between FAZ parameters and IOP changes in patients with glaucoma.
In our study, BCVA decreased significantly from the preoperative period (0.81 ± 0.18) to the postoperative sixth month (0.68 ± 18) on Snellen chart. This result was thought to be due to the high rate (90%) of our patients being phakic and the development of lens opacification in the postoperative period, consistent with the studies in the literature [25].
In our study, no significant changes were found in the inferior, superior, nasal and temporal RNFLT measurements. In the literature, there are different publications reporting no change or an increase in RNFLT after IOP-lowering medical or surgical treatment [26, 27]. In the postoperative period of our study, there was no significant change in mean cup / optic ratios in the RNFL analysis. Previous studies show that in congenital and juvenile-onset pediatric glaucoma patients, an improvement in optic disc cupping after surgical intervention is achieved with IOP reduction [28]. In adults, there are different publications showing that the rate of optic disc cupping increased or remained the same [29, 30]. Our follow-up values were consistent with studies in the literature. However, no significant change was found in mean and minimum GCA values in the postoperative period [13].
The preoperative mean VF-MD values of our patient group included in the study were 10.77 ± 6.39 dB and can be defined as moderate glaucoma. When the preoperative and postoperative VF-MD and PSD values of the patients were examined, statistically significant changes were observed. There are different publications in the literature stating that glaucomatous visual field losses may improve or stay the same after IOP-lowering medical or surgical treatment [6, 31, 32].
In patients with advanced stage glaucoma, decrease in OCTA image quality is observed due to decreased visual acuity and resultant fixation loss. Therefore, the results of the study may be limited to middle-stage glaucoma patients, we believe that these results may not be the same for patients with advanced stage glaucoma. For ethical and medical reasons, topical antiglaucomatous drugs are not discontinued in preoperative patients. Therefore, we can not exclude the possible effects of these medications on our results. Another limitation is that our study had to be completed with the number of patients less than originally planned due to the COVID-19 pandemic. Due to the low imaging quality of three patients, our evaluations were made on 20 patients.
According to the results of our study, we think that the FAZ region may be sensitive to surgically induced IOP changes. We also think that OCTA can be used especially in the evaluation of vascular perfusion in the FAZ region and in the follow-up period after glaucoma surgery. It was concluded that OCTA has the potential to improve our understanding of ocular perfusion, while also providing valuable information about the prognosis of patients with surgically reduced IOP.
References
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311:1901–11.
Gardiner SK, Fortune B, Wang L, Downs JC, Burgoyne CF. Intraocular pressure magnitude and variability as predictors of rates of structural change in non-human primate experimental glaucoma. Exp Eye Res. 2012;103:1–8.
Weinreb RN, Leung CK, Crowston JG, Medeiros FA, Friedman DS, Wiggs JL, Martin KR. Primary open-angle glaucoma. Nat Rev Dis Primers. 2016;2:16067.
Leske MC. Ocular perfusion pressure and glaucoma: clinical trial and epidemiologic findings. Curr Opin Ophthalmol. 2009;20:73–8.
Findl O, Rainer G, Dallinger S, Dorner G, Polak K, Kiss B, et al. Assessment of optic disk blood flow in patients with open-angle glaucoma. Am J Ophthalmol. 2000;130:589–96.
Bengtsson B, Heijl A. Lack of visual field improvement after initiation of intraocular pressure reducing treatment in the early manifest glaucoma trial. Invest Ophthalmol Vis Sci. 2016;57:5611–5.
Trible JR, Costa VP, Sergott RC, Spaeth GL, Smith M, Wilson RP, et al. The influence of primary open-angle glaucoma upon the retrobulbar circulation: baseline, postoperative and reproducibility analysis. Trans Am Ophthalmol Soc. 1993;91:245–61 (discussion 61-5).
Polska E, Simader C, Weigert G, Doelemeyer A, Kolodjaschna J, Scharmann O, et al. Regulation of choroidal blood flow during combined changes in intraocular pressure and arterial blood pressure. Invest Ophthalmol Vis Sci. 2007;48:3768–74.
Chen HS, Liu CH, Wu WC, Tseng HJ, Lee YS. Optical coherence tomography angiography of the superficial microvasculature in the macular and peripapillary areas in glaucomatous and healthy eyes. Invest Ophthalmol Vis Sci. 2017;58:3637–45.
Yarmohammadi A, Zangwill LM, Diniz-Filho A, Suh MH, Manalastas PI, Fatehee N, et al. Optical coherence tomography angiography vessel density in healthy, glaucoma suspect, and glaucoma eyes. Invest Ophthalmol Vis Sci. 2016;57:Oct451-9.
Rulli E, Biagioli E, Riva I, Gambirasio G, De Simone I, Floriani I, et al. Efficacy and safety of trabeculectomy vs nonpenetrating surgical procedures: a systematic review and meta-analysis. JAMA Ophthalmol. 2013;131:1573–82.
Zéboulon P, Lévêque PM, Brasnu E, Aragno V, Hamard P, Baudouin C, et al. Effect of surgical intraocular pressure lowering on peripapillary and macular vessel density in glaucoma patients: an optical coherence tomography angiography study. J Glaucoma. 2017;26:466–72.
Lommatzsch C, Rothaus K, Koch JM, Heinz C, Grisanti S. Retinal perfusion 6 months after trabeculectomy as measured by optical coherence tomography angiography. Int Ophthalmol. 2019;39:2583–94.
Holló G. Influence of large intraocular pressure reduction on peripapillary OCT vessel density in ocular hypertensive and glaucoma eyes. J Glaucoma. 2017;26:e7–10.
Shin JW, Sung KR, Uhm KB, Jo J, Moon Y, Song MK, et al. Peripapillary microvascular improvement and lamina cribrosa depth reduction after trabeculectomy in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2017;58:5993–9.
Kim JA, Kim TW, Lee EJ, Girard MJA, Mari JM. Microvascular changes in peripapillary and optic nerve head tissues after trabeculectomy in primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 2018;59:4614–21.
Kara N, Baz O, Altan C, Satana B, Kurt T, Demirok A. Changes in choroidal thickness, axial length, and ocular perfusion pressure accompanying successful glaucoma filtration surgery. Eye (Lond). 2013;27:940–5.
Dimitrova G, Chihara E. Implication of deep-vascular-layer alteration detected by optical coherence tomography angiography for the pathogenesis of diabetic retinopathy. Ophthalmologica. 2019;241:179–82.
Grunwald JE, Sinclair SH, Riva CE. Autoregulation of the retinal circulation in response to decrease of intraocular pressure below normal. Invest Ophthalmol Vis Sci. 1982;23(1):124–7.
Flammer J, Orgül S. Optic nerve blood-flow abnormalities in glaucoma. Prog Retin Eye Res. 1998;17:267–89.
Ch’ng TW, Gillmann K, Hoskens K, Rao HL, Mermoud A, Mansouri K. Effect of surgical intraocular pressure lowering on retinal structures—nerve fibre layer, foveal avascular zone, peripapillary and macular vessel density: 1 year results. Eye (Lond). 2020;34:562–71.
Spaide RF, Fujimoto JG, Waheed NK, Sadda SR, Staurenghi G. Optical coherence tomography angiography. Prog Retin Eye Res. 2018;64:1–55.
Zivkovic M, Dayanir V, Kocaturk T, Zlatanovic M, Zlatanovic G, Jaksic V, et al. Foveal avascular zone in normal tension glaucoma measured by optical coherence tomography angiography. Biomed Res Int. 2017;2017:3079141.
Kwon J, Choi J, Shin JW, Lee J, Kook MS. Alterations of the foveal avascular zone measured by optical coherence tomography angiography in glaucoma patients with central visual field defects. Invest Ophthalmol Vis Sci. 2017;58:1637–45.
Van Veldhuisen PC, Ederer F, Gaasterland DE, Sullivan EK, Beck A, Prum BE, et al. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS investigators. Am J Ophthalmol. 2000;130:429–40.
Aydin A, Wollstein G, Price LL, Fujimoto JG, Schuman JS. Optical coherence tomography assessment of retinal nerve fiber layer thickness changes after glaucoma surgery. Ophthalmology. 2003;110:1506–11.
Chang PT, Sekhon N, Budenz DL, Feuer WJ, Park PW, Anderson DR. Effect of lowering intraocular pressure on optical coherence tomography measurement of peripapillary retinal nerve fiber layer thickness. Ophthalmology. 2007;114:2252–8.
Meirelles SH, Mathias CR, Bloise RR, Stohler NS, Liporaci SD, Frota AC, et al. Evaluation of the factors associated with the reversal of the disc cupping after surgical treatment of childhood glaucoma. J Glaucoma. 2008;17:470–3.
Sanchez FG, Sanders DS, Moon JJ, Gardiner SK, Reynaud J, Fortune B, et al. Effect of trabeculectomy on OCT measurements of the optic nerve head neuroretinal rim tissue. Ophthalmol Glaucoma. 2020;3:32–9.
Raghu N, Pandav SS, Kaushik S, Ichhpujani P, Gupta A. Effect of trabeculectomy on RNFL thickness and optic disc parameters using optical coherence tomography. Eye (Lond). 2012;26:1131–7.
Spaeth GL, Ichhpujani P. Visual improvement in patients with far-advanced glaucoma. J Curr Glaucoma Pract. 2009;3:36–8.
Wild JM, Searle AE, Dengler-Harles M, O’Neill EC. Long-term follow-up of baseline learning and fatigue effects in the automated perimetry of glaucoma and ocular hypertensive patients. Acta Ophthalmol (Copenh). 1991;69:210–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
D. Güngör, None; Ö. R. Kayıkçıoğlu, None; M. Altınışık, None; S. Doğruya, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Suzan Doğruya
About this article
Cite this article
Güngör, D., Kayıkçıoğlu, Ö.R., Altınışık, M. et al. Changes in optic nerve head and macula optical coherence tomography angiography parameters before and after trabeculectomy. Jpn J Ophthalmol 66, 305–313 (2022). https://doi.org/10.1007/s10384-022-00919-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-022-00919-y