Abstract
Purpose
To elucidate how factors associated with swimming affect the lacrimal ducts of swimmers.
Study design
Prospective, interventional cohort study,
Methods
Five hundred seventy four consecutive epiphora patients were surveyed via a questionnaire regarding details of their swimming-pool usage; i.e., frequency, swim-goggles’ wear, and type of pool activity (i.e., swimming vs. waist-depth walking). In this cohort, all the swimmers over 20 years old with anatomical lacrimal duct obstruction underwent surgical reconstruction. The surgical success rates at 12-months postoperative were compared using multivariable logistic regression analyses between swimmer/non-swimmer patients, those with a history of high/low frequency of pool usage, and those with high/low amount of conjunctival contact with the swimming-pool water.
Results
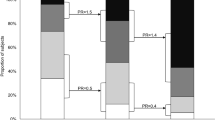
Of the patients with anatomical lacrimal duct obstruction, 6.4% were habitual swimmers; nasolacrimal duct obstruction was more common in the swimmers than in the non-swimmers’ controls (89.1%/66.7%, P = 0.025). The success rate of lacrimal surgery for the swimmers with anatomical nasolacrimal duct obstruction was lower (60.6%) than of the non-swimmers (83.3%, P = 0.048). A receiver operating characteristic curve analysis of the frequency for the prediction of surgical failure showed that the threshold was 4 days/week. The success rate was statistically lower (26.7%) in the high-frequency swimmers compared to the low-frequency swimmers (88.9%, P = 0.037). However, no statistical difference in the high/low ocular surface contact to the swimming-pool water was observed (71.4%/57.7%, P = 0.56).
Conclusion
Habitual swimmers have a high risk of nasolacrimal-duct damage retrogradely from the nasal cavity that lowers lacrimal surgery's success rate.

Similar content being viewed by others
References
World Health Organization. Guidelines for safe recreational water environments. Geneva, Switzerland: World Health Organization. 2003. https://apps.who.int/iris/bitstream/handle/10665/42591/9241545801.pdf;jsessionid=56AC409DE3055647F7F233D3CE6B563B?sequence=1. Accessed 31 May 2020.
Deitmer T, Scheffler R. Nasal physiology in swimmers and swimmers’ sinusitis. Acta Otolaryngol. 1990;110:286–91.
Gelardi M, Teresa Ventura M, Fiorella R, Luisa Fiorella M, Russo C, Candreva T, et al. Allergic and non-allergic rhinitis in swimmers: clinical and cytological aspects. Br J Sports Med. 2012;46:54–8.
Ishioka M, Kato N, Kobayashi A, Dogru M, Tsubota K. Deleterious effects of swimming pool chlorine on the corneal epithelium. Cornea. 2008;27:40–3.
Khodaee M, Edelman GT, Spittler J, Wilber R, Krabak BJ, Solomon D, et al. Medical care for swimmers. Sport Med Open. 2015;2:27.
Odaira H, Takasaki T, Sawai T. Permeability change of guinea pig nasal epithelium after exposure of hypotonic solution. Nippon Jibiinkoka Gakkai Kaiho. 1988;91:2003–10 (in Japanese).
Kabata Y, Goto S, Takahashi G, Tsuneoka H. Vision-related quality of life in patients undergoing silicone tube intubation for lacrimal passage obstructions. Am J Ophthalmol. 2011;152:147-50.e2.
Kondoh E, Watanabe A, Ueda K, Kimura N, Wakimasu K, Araki B, et al. Relation between acquired dacryostenosis and frequent pool use. J Eye. 2012;29:411–4 (in Japanese).
Ohtomo K, Ueta T, Toyama T, Nagahara M. Predisposing factors for primary acquired nasolacrimal duct obstruction. Graefes Arch Clin Exp Ophthalmol. 2013;251:1835–9.
Fernández-Luna Á, Burillo P, Felipe JL, del Corral J, García-Unanue J, Gallardo L. Perceived health problems in swimmers according to the chemical treatment of water in swimming pools. Eur J Sport Sci. 2016;16:256–65.
Paulsen FP, Thale AB, Maune S, Tillmann BN. New insights into the pathophysiology of primary acquired dacryostenosis. Ophthalmology. 2001;108:2329–36.
Mimura M, Ueki M, Oku H, Sato B, Ikeda T. Indications for and effects of Nunchaku-style silicone tube intubation for primary acquired lacrimal drainage obstruction. Jpn J Ophthalmol. 2015;59:266–72.
Schaeffer JP. Types of ostia nasolacrimalia in man and their genetic significance. Am J Anat. 1912;13:183–92.
Orhan M, Ikiz ZAA, Saylam CY. Anatomical features of the opening of the nasolacrimal duct and the lacrimal fold (Hasner’s valve) for intranasal surgery: a cadaveric study. Clin Anat. 2009;22:925–31.
Couri D, Abdel-Rahmant MS, Bull RJ. Toxicological effects of chlorine dioxide, chlorite and chlorate. Environ Health Perspect. 1982;46:13–7.
Martin JG, Campbell HR, Iijima H, Gautrin D, Malo J-L, Eidelman DH, et al. Chlorine-induced injury to the airways in mice. Am J Respir Crit Care Med. 2003;168:568–74.
Ryu M, Kobayashi T, Kawamukai E, Quan G, Furuta T. Cytotoxicity assessment of residual high-level disinfectants. Biocontrol Sci. 2013;18:217220.
World Health Organization. Chlorine dioxide (gas). Geneva, Switzerland. 2002. https://www.who.int/ipcs/publications/cicad/en/cicad37.pdf. Accessed 31 May 2020.
Canelli E, Chem D. Chemical, bacteriological, and toxicological properties of cyanuric acid and chlorinated isocyanurates as applied to swimming pool disinfection a review. Am J Public Health. 1974;64:155–63.
White CW, Martin JG. Chlorine gas inhalation: human clinical evidence of toxicity and experience in animal models. Proc Am Thorac Soc. 2010;7:257–63.
Andersson M, Backman H, Nordberg G, Hagenbjörk A, Hedman L, Eriksson K, et al. Early life swimming pool exposure and asthma onset in children—a case-control study. Environ Health. 2018;17:34.
Weisel CP, Richardson SD, Nemery B, Aggazzotti G, Baraldi E, Blatchley ER, et al. Childhood asthma and environmental exposures at swimming pools: state of the science and research recommendations. Environ Health Perspect. 2009;117:500–7.
Yildirim C, Kocoglu H, Goksu S, Cengiz B, Sari I, Bagci C. Long-term pulmonary histopathologic changes in rats following acute experimental exposure to chlorine gas. Inhal Toxicol. 2004;16:911–5.
Ministry of Health, Labor and Welfare J. Regulations for sanitation control in recreational water pool (Nortification No.0528003). Tokyo; 2007. https://ci.nii.ac.jp/naid/10030448108/. Accessed 31 May 2020 (Japanese).
Acknowledgements
The authors wish to thank John Bush for reviewing the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
M. Mimura, None; Y. Sato, None; Y. Fujita, None; H. Oku, None; B. Sato, None; T. Ikeda, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding author: Masashi Mimura
About this article
Cite this article
Mimura, M., Sato, Y., Fujita, Y. et al. Impact of habitual swimming on the success of lacrimal surgery. Jpn J Ophthalmol 65, 849–854 (2021). https://doi.org/10.1007/s10384-021-00865-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00865-1