Abstract
Purpose
To compare the efficacy of bandage contact lenses with two different base curves in promoting epithelial healing after epithelial laser in situ keratomileusis (epi-LASIK).
Methods
A prospective, observer-masked study was conducted in 27 patients. Each patient randomly received one bandage contact lens with an 8.4-mm base curve in one eye and one with an 8.8-mm base curve in the fellow eye. Corneal epithelial status, pain score, spherical equivalent, and uncorrected visual acuity (UCVA) were examined during the first postoperative month.
Results
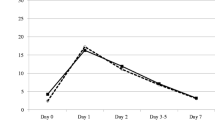
Corneal epithelial status, postoperative pain, and spherical equivalent were similar for both lenses during the first postoperative month. The eyes with lenses with an 8.8-mm base curve had better UCVA on postoperative day (POD) 4, but there was no significant difference in UCVA after POD 7. In the patients with preoperative low to moderate myopia and low keratometric values (<43.0 D), there was no significant difference in the postoperative UCVA between the lenses. On the other hand, in patients with preoperative high myopia and high keratometric values (≥43.0 D), UCVA was better in eyes with lenses with an 8.8-mm base curve on POD 4.
Conclusions
These findings suggest that the base curves of bandage contact lenses affect visual rehabilitation after epi-LASIK, particularly in patients with a steep cornea and high myopia.
Similar content being viewed by others
References
Selier T, Wollensak J. Myopic photorefractive keratectomy with the excimer laser; one-year follow-up. Ophthalmology 1991;98:1156–1163.
Epstein D, Fagerholm P, Hamberg-Nystrom H, Tengroth B. Twenty-four-month follow-up of excimer laser photorefractive keratectomy for myopia; refractive and visual results. Ophthalmology 1994;101:1558–1563.
Duffey RJ, Leaming D. US trends in refractive surgery: 2004 ISRS/AAO Survey. J Refract Surg 2005;21:742–748.
Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumdi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK. Curr Opin Ophthalmol 2003;14:207–212.
Panagopoulou SI, Pallikaris IG. Wavefront customized ablations with WASCA Asclepion workstation. J Refract Surg 2001;17:608–612.
Katsanevaki VJ, Naoumidi II, Kalyvianaki MI, Pallikaris G. epi-LASIK: histological findings of separated epithelial sheets 24 hours after treatment. J Refract Surg 2006;22:151–154.
Christie CL. Therapeutic contract lens. Cont Lens Anterior Eye 1999;22:20–25.
Cherry PMH. The treatment of pain following excimer laser photorefractive keratectomy: additive effect of local anesthetic drops, topical diclofenac, and bandage soft contact. Ophthalmic Surg Lasers 1996;27:477–480.
Tomas-Barberan S, Fagerholm P. Influence of topical treatment on epithelial wound healing and pain in the early postoperative period following photorefractive keratectomy. Acta Ophthalmol Scand 1999;77:135–138.
Donnenfeld ED, Selkin BA, Perry HD, et al. Controlled evaluation of a bandage contact lens and a topical nonsteroidal anti-inflammatory drug in treating traumatic corneal abrasions. Ophthalmology 1995;102:979–984.
Mannis MJ. Therapeutic contact lenses. In: Smolin G, Thoft RA, editors. The cornea, 3rd ed. Boston: Little Brown; 1994. v.1. chap. 26.
Smiddy WE, Hamburg TR, Kracher GP, et al. Therapeutic contact lenses. Ophthalmology 1990;97:291–295.
Kaufman H, Gasset AR. Therapeutic soft bandage lenses. Int Ophthalmol Clin 1970;10:379–385.
Engle AT, Laurent JM, Schallhorn SC, et al. Masked comparison of silicone hydrogel lotrafilcon A and etafilcon A extended-wear bandage contact lenses after photorefractive keratectomy. J Cataract Refract Surg 2005;31:681–686.
Gil-Cazorla R, Teus MA, Arranz-Márquez E. Comparison of silicone and non-silicone hydrogel soft contact lenses used as a bandage after LASEK. J Refract Surg 2008;24:199–203.
Edwards JD, Bower KS, Sediq DA, et al. Effects of lotrafilcon A and omafilcon A bandage contact lenses on visual outcomes after photorefractive keratectomy. J Cataract Refract Surg 2008 Aug; 34:1288–1294.
Szafilk JP, Ambroziak AM, Szaflik J. Therapeutic use of a latafilcon A silicone hydrogel soft contact lens as a bandage after LASEK surgery. Eye Contact Lens 2004;30:59–62.
Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: epi-LASIK. Curr Opin Ophthalmol 2003;14:207–212.
Helena MC, Baerveldt F, Kim WJ, et al. Keratocyte apoptosis after corneal surgery. Invest Ophthalmol Vis Sci 1998;39:276–283.
Moller-Pedersen T, Cavanagh HD, Petrol WM, et al. Corneal haze development after PRK is regulated by volume of stromal tissue removal. Cornea 1998;17:627–639.
Moller-Pedersen T. The cellular basis of corneal transparency and haze development. Ophthalmic Res 2002;34:1–13.
Netto MV, Mohan RR, Ambrosio R Jr, Hutcheon AE, Zieske JD, Wilson SE. Wound healing in the cornea: a review of refractive surgery complications and new prospects for therapy. Cornea 2005;24:509–522.
Tanioka H, Hieda O, Kawasaki S, Nakai Y, Kinoshita S. Assessment of epithelial integrity and cell viability in epithelial flaps prepared with the epi-LASIK procedure. J Cataract Refract Surg 2007;33:1195–1200.
Fonn D, du Toit R, Simpson TL, et al. Sympathetic swelling response of the control eye to soft lenses in the other eye. Invest Ophthalmol Vis Sci 1999;40:3116–3123.
Wang X, McCulley JP, Bowman RW, Cavanagh HD. Time to resolution of contact lens-induced corneal warpage prior to refractive surgery. CLAO J 2002;28:169–171.
Hashemi H, Firoozabadi MR, Mehravaran S, Gorouhi F. Corneal stability after discontinued soft contact lens wear. Cont Lens Anterior Eye 2008;31:122–125.
Seo JH, Wee WR, Lee JH, Kim MK. Effect of base curve radius of therapeutic lenses on epithelial healing after laser-assisted subepithelial keratectomy. Korean J Ophthalmol 2007;21:85–89.
Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Anterior Eye 2002;25:137–146.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kim, JS., Na, KS. & Joo, CK. Base curves of therapeutic lenses and their effects on post Epi-LASIK vision and pain: A prospective randomized clinical trial. Jpn J Ophthalmol 53, 368–373 (2009). https://doi.org/10.1007/s10384-009-0672-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-009-0672-9