Summary
Background
The risk of thromboembolic events is increased for coronavirus disease (COVID)-19 inpatients. For severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-infected outpatients, only few data are available so far.
Methods
In our prospective single-center study, 461 SARS-CoV-2-infected outpatients were screened for the presence of deep vein thrombosis.
Results
Two outpatients had suffered a deep vein thrombosis. An association with previously known risk factors, such as preexisting thrombosis in the medical history or cardiovascular risk factors, could not be proven.
Conclusion
General thromboprophylaxis in SARS-CoV-2-infected outpatients is still not recommended.
Zusammenfassung
Grundlagen
Das Risiko für thrombembolische Ereignisse ist für stationäre COVID-19-Patienten erhöht. Für ambulant behandelte SARS-CoV-2-Infizierte liegen bisher nur wenige Daten vor.
Methodik
In der prospektiven Single-Center-Studie der Autoren wurden 461 SARS-CoV-2-Infizierte mit ambulantem Behandlungsverlauf auf das Vorliegen einer tiefen Beinvenenthrombose untersucht.
Ergebnisse
Bei 2 ambulanten Patienten war eine Beinvenenthrombose aufgetreten. Ein Zusammenhang mit bisher bekannten Risikofaktoren, wie vorbestehender Thrombose in der Anamnese oder kardiovaskulären Risikofaktoren, konnte nicht nachgewiesen werden.
Schlussfolgerung
Eine generalisierte Thromboseprophylaxe bei ambulanten SARS-CoV-2-Infizierten wird weiterhin nicht empfohlen.
Similar content being viewed by others
Introduction
An increased risk of thromboembolic events has been described several times for patients with COVID-19 disease [1, 2]. A recent meta-analysis estimates the risk for hospitalized patients at 14.1%, and for intensive care patients as high as 22.7% [3]. Little is known about the risk of outpatients. As the recently updated guidelines of various medical professional societies confirm, the evidence on thrombosis prophylaxis for outpatient infected patients is to be rated as very low [4, 5].
The primary endpoint of the present study was to survey the prevalence of thrombosis in SARS-CoV-2-infected outpatients and correlate it with the risk factors described in previous studies.
Materials and methods
The present study is a prospective single-center study. Patient acquisition was carried out via the local health offices of the city and district of Augsburg. All residents reported there with a positive SARS-CoV‑2 smear by November 2020 (n = 1600) were invited in writing to voluntarily participate in the study. At the time of examination, the positive smear had to be at least 14 days old, and the quarantine had to have been lifted.
A positive vote of the ethics committee of the Ludwig Maximilian University of Munich has been obtained (no. 20-735), and the study has also been registered with Clinical Trials (no. NCT04615026).
In the period from 11.2020 to 05.2021, a total of 525 subjects were examined at the University Hospital Augsburg after having had a SARS-CoV‑2 infection, with a focus on vascular complications such as deep vein thrombosis (DVT) or intermittent claudication. Of these subjects, 461 study participants had been treated exclusively as outpatients; the hospitalized patients were excluded for this data collection because the focus of the study was on the outpatient cohort (Fig. 1).
In addition to the course of the disease, demographic data, comorbidities, previous medication, and risk factors for severe courses and the occurrence of thromboembolic events (TE) were recorded. Clinical examinations included compression ultrasonography of the leg veins and determination of the ankle-brachial index in case of a history of intermittent claudication. The course of the disease was recorded using a standardized questionnaire. The documentation, quality assurance, and storage of the study data were pseudonymized in a database.
The descriptive statistics were compiled with the analysis program SAS (version 9.4, SAS Institute Inc., Cary, NC, USA). The metric data were tested for normal distribution; if nonnormal, the median and interquartile range were reported.
Results
The response rate after study invitation was 32.8%. Median age of the study participants was 49 years, 209 men and 252 women were included. The mean time interval between the first positive PCR test for the SARS-CoV‑2 virus and examination in the study was 238 days.
The demographic data, cardiovascular risk factors, and comorbidities are shown in Table 1.
Regarding severity, there were various clinical courses of SARS-CoV‑2 infection. In 2.8%, the infection remained asymptomatic. The frequencies of different SARS-CoV-2-associated symptoms are shown in Table 2.
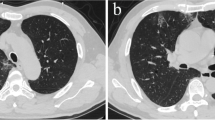
The prevalence of deep vein thrombosis (DVT) was determined for the 461 outpatients treated in the study. A total of two DVT were found (0.4%). In 3.5% of the patients, a coagulation medication was administered during the infection.
There were no differences in the classic cardiovascular risk factors between the group with DVT compared to the group without DVT.
Symptoms of leg swelling and calf pain were reported by 22 and 75 study participants, respectively. These were present in only one of the two participants with DVT.
The classic risk factors for DVT are shown in Table 3.
None of the subjects with DVT were on long-term anticoagulant medication. One of the DVT patients had a body mass index (BMI) above 30. Bleeding events were not reported. The detailed clinical characteristics of the two patients with DVT are shown in Table 4.
Arterial events did not occur. One subject complained of a new walking distance restriction since the SARS-CoV‑2 infection. In this case, the ABI was recorded and within the normal range (1.2).
Discussion
In the present study, two DVTs were detected among the 461 SARS-CoV-2-infected outpatients, which corresponds to 0.4% of the collective.
The prevalence of DVT in the overall population is age dependent and ranges from 0.9 to 10.7% [6]. Thus, there are no indications of an increased DVT prevalence in outpatients with SARS-CoV‑2 infection.
An increased incidence of TE in COVID-19 disease was observed in hospitalized patients [7]; these findings cannot be generalized to outpatients.
The course of the disease in hospitalized patients is generally more severe and complicated, especially due to the triggered immune reactions [8,9,10,11].
A total of 16 study participants reported that they had received anticoagulation medication (antiplatelet or anticoagulation) during the infection. The reasons for this were not recorded. At the time the study was conducted, there were no scientific findings on the risk of DVT in outpatients, which is why this was presumably an empirical medication based on the known increased risk for inpatients at this time.
Several risk factors for the clustered occurrence of TE in COVID inpatients have been described. These include age over 60 years, arterial hypertension, and diabetes mellitus [12]. In our data collection, however, there was no significantly increased risk of DVT for the outpatients with corresponding risk factors. The classic risk factors in the sense of the Virchow triad also did not lead to an increased incidence of thrombosis.
No DVT occurred under a pre-existing anticoagulant medication.
In a national Scottish registry study that included both inpatients and outpatients, an increased risk of TE was demonstrated, particularly in the first 7 days after a positive test result [13].
The prospective study by Connors et al. on antithrombotic therapy in outpatients was stopped because the occurrence of thromboembolic events was too rare [14]. This is confirmed by the data we collected; generalized implementation of thromboprophylaxis in SARS-CoV-2-infected outpatients can still not be recommended. In symptomatic patients with a high-risk profile, pharmacological thromboprophylaxis can be considered if there are no contraindications. The individual risk of bleeding should always be considered [5, 15].
Strengths and limitations
The strengths of the present study are the large number of patients and the high response rate after invitation, which represents a good cross section of the normal population. Limitations are the lack of a control group and the relatively young age of the patients. In addition, the data collection was carried out in during fixed period of time, thus representing different intervals to the infection and not according to a standardized interval. Therefore, it is a survey of prevalence and not incidence. The thromboses diagnosed in color-coded doppler sonography (CCDS) cannot be reliably correlated with the time of SARS-CoV‑2 infection if the clinical course is asymptomatic.
The transferability of our results to newer virus variants is limited due to the different disease courses.
References
Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–50.
Zerwes S, Hernandez Cancino F, Liebetrau D, Gosslau Y, Warm T, Märkl B, et al. Increased risk of deep vein thrombosis in intensive care unit patients with CoViD-19 infections? - Preliminary data. Chirurg. 2020;91(7):588–94.
Nopp S, Moik F, Jilma B, Pabinger I, Ay C. Risk of venous thromboembolism in patients with COVID-19: a systematic review and meta-analysis. Res Pract Thromb Haemost. 2020;4(7):1178–91.
Blankenfeld H, Kaduszkiewicz H, Kochen M, Pömsl J. S2e-Leitlinie: SARS-CoV-2/Covid-19-Informationen & Praxishilfen für niedergelassene Hausärztinnen und Hausärzte: Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin e. V. (DEGAM). 2022.
Kluge S, Janssens U, Welte T, Weber-Carstens S, Schälte G, Spinner C. S3-Leitlinie – Empfehlungen zur stationären Therapie von Patienten mit COVID-19. 2022. Deutsche Gesellschaft für Internistische Intensivmedizin und Notfallmedizin (DGIIN), Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI), Deutsche Gesellschaft für Pneumologie und Beatmungsmedizin (DGP), Deutsche Gesellschaft für Infektiologie (DGI).
Rabe E, Bauersachs RM, Pannier F, List S. Themenheft 44 „Venenerkrankungen der Beine“. Berlin: Robert Koch-Institut; 2009. p. 39.
Tzaneva S. Thrombose und COVID-19. hautnah. 2021;20(2):92–7.
Leentjens J, van Haaps TF, Wessels PF, Schutgens REG, Middeldorp S. COVID-19-associated coagulopathy and antithrombotic agents-lessons after 1 year. Lancet Haematol. 2021;8(7):e524–e33.
Miesbach W, Makris M. COVID-19: coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Clin Appl Thromb Hemost. 2020;26:1076029620938149.
Ahmed S, Zimba O, Gasparyan AY. Thrombosis in Coronavirus disease 2019 (COVID-19) through the prism of Virchow’s triad. Clin Rheumatol. 2020;39(9):2529–43.
Gu SX, Tyagi T, Jain K, Gu VW, Lee SH, Hwa JM, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol. 2021;18(3):194–209.
Gabbai-Armelin PR, de Oliveira AB, Ferrisse TM, Sales LS, Barbosa ERO, Miranda ML, et al. COVID-19 (SARS-CoV-2) infection and thrombotic conditions: a systematic review and meta-analysis. Eur J Clin Invest. 2021;51(6):e13559.
Ho FK, Man KKC, Toshner M, Church C, Celis-Morales C, Wong ICK, et al. Thromboembolic risk in hospitalized and nonhospitalized COVID-19 patients: a self-controlled case series analysis of a nationwide cohort. Mayo Clin Proc. 2021;96(10):2587–97.
Connors JM, Brooks MM, Sciurba FC, Krishnan JA, Bledsoe JR, Kindzelski A, et al. Effect of antithrombotic therapy on clinical outcomes in outpatients with clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial. JAMA. 2021;326(17):1703–12.
Darius H, Grothues J, Haas S, Heinemann M, Klamroth R, Miesbach W. Prevention of venous thromboembolism in COVID-19 outpatients. MMW Fortschr Med. 2021;163(8):56–7.
Acknowledgements
We would like to thank the health departments of Augsburg City and State for their cooperation and Mrs. Daniela Jarosch for the documentation and assistance with statistical evaluation.
Funding
Corona research projects of the Bavarian State Ministry for Science and Art.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yvonne Goßlau, Tobias Dominik Warm, Inge Kirchberger, and Christine Meisinger. The first draft of the manuscript was written by Yvonne Goßlau and Tobias Dominik Warm, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Y. Goßlau, T. D. Warm, E.F. Hernandez Cancino, I. Kirchberger, C. Meisinger, J. Linseisen, and A. Hyhlik-Duerr declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goßlau, Y., Warm, T.D., Hernandez Cancino, E.F. et al. The prevalence of vascular complications in SARS-CoV-2 infected outpatients. Wien Med Wochenschr 173, 168–172 (2023). https://doi.org/10.1007/s10354-022-00954-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-022-00954-x