Summary
Background
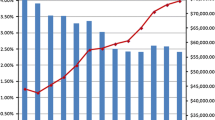
The purpose of this study was to financially profile four different types of elective colectomy resection in relation to diagnosis and complications.
Methods
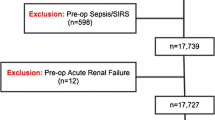
A total of 1420 colectomies from three centers within our system were analyzed for diagnostic, complications, financial, length of stay (LOS), and case mix index (CMI) data for four procedure categories: colectomy above peritoneal reflection (AR) with diversion, colectomy AR without diversion, colectomy below peritoneal reflection (BR) with diversion, and colectomy BR without diversion. The incidence of complications and costs were compared between procedure groups. Logit models were used for probabilities of complications and Poisson for rate analysis.
Results
Elective colectomies AR were performed 72% of the time for non-inflammatory diagnoses (benign tumors, polyps, rectal prolapse, malignant tumors), whereas resections BR were performed 64% of the time for inflammatory diagnoses (diverticulitis, Crohn’s, ulcerative colitis, perforation, obstruction, sepsis, fistulae). Thus, diversion was performed in a higher proportion of cases with inflammatory diagnoses and cases requiring diversion had higher complication rates in both AR (16% vs. 5%) and BR (19% vs. 6%) resections.
Conclusion
Inflammatory diagnoses appear to drive the indication for diversion following elective colectomy. Colectomies with diversion have complication rates 1.36 times higher than without diversion, as well as excess LOS and costs. Resections AR with diversion had more than twice the proportion of complications as without diversion. Preoperative mitigation of inflammatory risk factors may decrease the rate of diversion and reduce complications, financial risk, and opportunity cost.

Similar content being viewed by others
References
Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313(5):483–95.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative resection for colorectal cancer. ann Surg. 2015;261(3):497–505.
Fry DE, Pine M, Nedza SM, Locke DG, Reband AM, Pine G. Benchmarking hospital outcomes for improvement of care in medicare elective colon surgery. Am J Surg. 2016;212(1):10–5.
Tevis SE, Kennedy GD. Postoperative complications: looking forward to a safer future. Clin Colon Rectal Surg. 2016;29(3):246–52.
Morris AM, Baldwin LM, Matthews B, Dominitz JA, et al. Reoperation as a quality indicator in colorectal surgery: a population-based analysis. ann Surg. 2007;245(1):73–9.
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56(5):667–78.
Keane C, Savage S, McFarlane K, et al. Enhanced recovery after surgery versus conventional care in colonic and rectal surgery. ANZ J Surg. 2012;82(10):697–703.
Birkmeyer JD, Gust C, Dimick JB, Birkmeyer NJO, Skinner JS. Hospital quality and the cost of inpatient surgery in the United States. Ann Surg. 2012;255(1):1–5. https://doi.org/10.1097/SLA.0b013e3182402c17.
Eappen S, Lane BH, Rosenberg B. Relationship between occurrence of surgical complications and hospital finances. JAMA. 2013;309(15):1599–606.
Govaert JA, Fiocco M, van Dijk WA, et al. Costs of complications after colorectal cancer surgery in the Netherlands: building the business case for hospitals. EJSO. 2015;41:1059–67.
Antonacci AC, Lam S, Lavarias V, Homel P, Eavey RD. A morbidity and mortality conference-based classification system for adverse events: surgical outcome analysis: part I. J Surg Res. 2008;147:172–7.
Antonacci AC, Lam S, Lavarias V, Homel P, Eavey RA. A report card system using error profile analysis and concurrent morbidity and mortality review: surgical outcome analysis, part II. J Surg Res. 2009;153:95–104.
Antonacci AC, Dechario S, Husk G, Stoffels G, Antonacci CL, Jarrett M. Analysis of surgical judgment and mortality utilizing a critique algorithm-based database and morbidity/mortality conference (MMC) review. Acad Surg Congr. 2019.
Zogg CK, Najjar P, Rios Diaz AJ, et al. Rethinking priorities: cost of complications after elective colectomy. Ann Surg. 2016;264(2):312–22.
Healy MA, Mullard AJ, Campell DA, Dimick JB. Hospital and payer costs associated with surgical complications. JAMA Surg. 2016;151(9):823–30.
Vonlanthan R, Slankamenac K, Breitenstein, et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254(6):907–13.
Patel AS, Bergman A, Moore BW, Haglund U. The economic burden of complications occurring in major surgical procedures: a systematic review. Appl Health Econ Health Policy. 2013;11(6):577–92.
McIsaac DI, Hamilton GM, Abdulla K, et al. Validation of new ICD-10-based patient safety indicators for identification of in-hospital complications in surgical patients: a study of diagnostic accuracy. BMJ Qual Saf. 2020;29(3):209–16.
Marusch F, Koch A, Schmidt U, et al. Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum. 2002;45(9):1164–71.
Hüser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. 2008;248(1):52–60.
Montedori A, Cirocchi R, Farinella E, Sciannameo F, Abraha I. Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev. 2010; https://doi.org/10.1002/14651858.CD006878.pub2.
McKenna NP, Bews KA, Cima RR, Crowson CS, Habermann EB. Development of a risk score to predict anastomotic leak after left-sided colectomy: which patients warrant diversion? J Gastrointest Surg. 2020;24(1):132–43.
Fry DE, Pine M, Nedza SM, et al. Benchmarking hospital outcomes for improvement of care in Medicare elective colon surgery. Am J Surg. 2016;212(1):10–5.
Keenan JE, Speicher PJ, Thacker JKM, et al. The preventative surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg. 2014;149(10):1045–52.
Author information
Authors and Affiliations
Contributions
A. A. conceived of the original idea; A. A., G. H., and S. D. designed the database and implemented the data acquisition model; A. A., C. L. A., and S. D. performed the analytic calculations; D. C. and D. A. provided financial data; A. A., C. L. A., K. C., G. H., G. C., and M. J. contributed to the final version of the manuscript; all authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A.C. Antonacci, C.L. Antonacci, K. Carsky, S.P. Dechario, G. Husk, D. Caulfield, D. Allinger, G. Coppa, and M. Jarrett declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Antonacci, A.C., Antonacci, C.L., Carsky, K. et al. Elective colectomy financial and opportunity cost analysis: diagnosis, case type, diversion, and complications. Eur Surg 54, 104–112 (2022). https://doi.org/10.1007/s10353-021-00716-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-021-00716-w