Summary
Background
Clinical decision-making around the management of liver-limited stage IV colorectal cancer involves careful assessment of the potential risks and benefits of surgery. This balance can often be optimised through appropriate patient selection to ensure long-term benefit of any operation, with fastidious perioperative care to minimize risk.
Methods
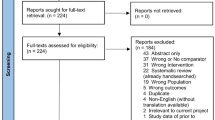
We reviewed selected relevant articles from the existing literature.
Results
Multi-platform imaging is routinely used to determine distribution of disease and whether lesions are technically resectable, but what remains less clear is how to identify patients in whom resection is likely to deliver long-term benefits. A number of prognostic markers have been identified, with growing interest in direct assessment of tumour biology; genotyping of RAS status is routine in specific situations. Following a multidisciplinary team decision to proceed to surgery, patients undergo perioperative assessment and optimisation. Cardiopulmonary exercise testing helps to stratify perioperative risk: patients with low uptake of oxygen at the anaerobic threshold are known to have worse perioperative outcomes, and prehabilitation may offer the chance to reduce this risk. Intraoperative anaesthetic management is on a patient-by-patient basis but sub-normal hydration, epidural anaesthesia and steroids play a key role. Enhanced recovery after surgery programmes have improved perioperative outcomes while providing a potential economic benefit.
Conclusion
Despite very good perioperative results, surgical management is not curative for the majority of patients, highlighting the need to further refine patient selection and definition of treatment aim on a patient-by-patient basis.
Similar content being viewed by others
References
Haraldsdottir S, Einarsdottir HM, Smaradottir A, Gunnlaugsson A, Halfdanarson TR. Colorectal cancer—review. Laeknabladid. 2014;100(2):75–82.
Cunningham D, Atkin W, Lenz HJ, et al. Colorectal cancer. Lancet. 2010;375(9719):1030–47.
Manfredi S, Lepage C, Hatem C, Coatmeur O, Faivre J, Bouvier AM. Epidemiology and management of liver metastases from colorectal cancer. Ann Surg. 2006;244(2):254–9.
Leporrier J, Maurel J, Chiche L, Bara S, Segol P, Launoy G. A population-based study of the incidence, management and prognosis of hepatic metastases from colorectal cancer. Br J Surg. 2006;93(4):465–74.
Akgül O, Çetinkaya E, Ersöz S, Tez M. Role of surgery in colorectal cancer liver metastases. World J Gastroenterol. 2014;20(20):6113–612.
Jones RP, Jackson R, Dunne DFJ, et al. Systematic review and meta-analysis of follow-up after hepatectomy for colorectal liver metastases. Br J Surg. 2012;99:477–86.
Heinemann V, von Weikersthal LF, Decker T, et al. FOLFIRI plus ce-tuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15:1065–75.
Kanas GP, Taylor A, Primrose JN, et al. Survival after liver resection in metastatic colorectal cancer: review and meta-analysis of prognostic factors. Clin Epidemiol. 2012;4:283–301.
Dunne DF, Yip VS, Jones RP, et al. Enhanced recovery in the resection of colorectal liver metastases. J Surg Oncol. 2014;110(2):197–202.
Jones RP, Brudvik KW, Franklin JM, Poston GJ. Precision surgery for colorectal liver metastases: opportunities and challenges of omics-based decision making. Eur J Surg Oncol. 2017;43(5):875–83.
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999;230(3):309–18.
Zakaria S, Donohue JH, Que FG, et al. Hepatic resection for colorectal metastases: value for risk scoring systems? Ann Surg. 2007;246(2):183–91.
Roberts KJ, White A, Cockbain A, et al. Performance of prognostic scores in predicting long-term outcome following resection of colorectal liver metastases. Br J Surg. 2014;101(7):856–66.
Schreckenbach T, Malkomes P, Bechstein WO, Woeste G, Schnitzbauer AA, Ulrich F. The clinical relevance of the Fong and the Nordlinger scores in the era of effective neoadjuvant chemotherapy for colorectal liver metastasis. Surg Today. 2015;45(12):1527–34.
Blazer DG 3rd, Kishi Y, Maru DM, et al. Pathologic response to preoperative chemotherapy: a new outcome end point after resection of hepatic colorectal metastases. J Clin Oncol. 2008;26(33):5344–51.
Andreou A, Kopetz S, Maru DM, et al. Adjuvant chemotherapy with FOLFOX for primary colorectal cancer is associated with increased somatic gene mutations and inferior survival in patients undergoing hepatectomy for metachronous liver metastases. Ann Surg. 2012;256(4):642–50.
Fernández-Medarde A, Santos E. Ras in cancer and developmental diseases. Genes Cancer. 2011;2(3):344–58.
Vauthey JN, Zimmitti G, Kopetz SE, et al. RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 2013;258(4):619–26. discussion 626–7.
Sepulveda AR, Hamilton SR, Allegra CJ, et al. Molecular biomarkers for the evaluation of colorectal cancer: guideline from the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J Clin Oncol. 2017; https://doi.org/10.1200/jco.2016.71.9807.
National Comprehensive Cancer Network. NCCN guidelines: colon cancer, version 2.2015. 2015.
Vauthey JN, Zimmitti G, Kopetz SE, et al. RAS mutation status predicts survival and patterns of recurrence in patients undergoing hepatectomy for colorectal liver metastases. Ann Surg. 2013;258(4):619–26.
Brudvik KW, Kopetz SE, Li L, Conrad C, Aloia TA, Vauthey JN. Meta-analysis of KRAS mutations and survival after resection of colorectal liver metastases. Br J Surg. 2015;102(10):1175–83.
Brudvik KW, Jones RP, Giuliante F, et al. RAS mutation clinical risk score to predict survival after resection of colorectal liver metastases. Ann Surg. 2017; https://doi.org/10.1097/sla.0000000000002319.
Dupré A, Malik HZ, Jones RP, Diaz-Nieto R, Fenwick SW, Poston GJ. Influence of the primary tumour location in patients undergoing surgery for colorectal liver metastases. Eur J Surg Oncol. 2017; https://doi.org/10.1016/j.ejso.2017.10.218.
Pugh SA, Shinkins B, Fuller A, Mellor J, Mant D, Primrose JN. Site and stage of colorectal cancer influence the likelihood and distribution of disease recurrence and postrecurrence survival: data from the FACS randomized controlled trial. Ann Surg. 2016;263(6):1143–7.
Poston GJ, Tait D, O’Connell S, Bennett A, Berendse S, Guideline Development Group. Diagnosis and management of colorectal cancer: summary of NICE guidance. BMJ. 2011;343:d6751.
Jones RP, Vauthey JN, Adam R, et al. Effect of specialist decision-making on treatment strategies for colorectal liver metastases. Br J Surg. 2012;99(9):1263–9.
Folprecht G, Gruenberger T, Bechstein WO, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11(1):38–47.
Choti MA, Thomas M, Wong SL, et al. Surgical resection preferences and perceptions among medical oncologists treating liver metastases from colorectal cancer. Ann Surg Oncol. 2015;23(2):375–81.
Dunne DF, Jones RP, Lythgoe DT, et al. Cardiopulmonary exercise testing before liver surgery. J Surg Oncol. 2014;110(4):439–44.
Snowden CP, Prentis J, Jacques B, et al. Cardiorespiratory fitness predicts mortality and hospital length of stay after major elective surgery in older people. Ann Surg. 2013;257(6):999–1004.
Kasivisvanathan R, Abbassi-Ghadi N, McLeod AD, et al. Cardiopulmonary exercise testing for predicting postoperative morbidity in patients undergoing hepatic resection surgery. HPB (Oxford). 2015;17(7):637–43.
Junejo MA, Mason JM, Sheen AJ, et al. Cardiopulmonary exercise testing for preoperative risk assessment before hepatic resection. Br J Surg. 2012;99(8):1097–104.
Dunne DF, Jack S, Jones RP, et al. Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg. 2016;103(5):504–12.
Chen H, Merchant NB, Didolkar MS. Hepatic resection using intermittent vascular inflow occlusion and low central venous pressure anesthesia improves morbidity and mortality. J Gastrointest Surg. 2000;4(2):162–7.
Melendez JA, Arslan V, Fischer ME, et al. Perioperative outcomes of major hepatic resections under low central venous pressure anesthesia: blood loss, blood transfusion, and the risk of postoperative renal dysfunction. J Am Coll Surg. 1998;187:620–5.
Feltracco P, Brezzi ML, Barbieri S, Serra E, Milevoj M, Ori C. Epidural anesthesia and analgesia in liver resection and living donor hepatectomy. Transplant Proc. 2008;40(4):1165–8.
Li H, Wei Y, Li B. Preoperative steroid administration in liver resection: a systematic review and meta-analysis. Hepatogastroenterology. 2013;60(121):160–9.
Adamina M, Kehlet H, Tomlinson GA, Senagore AJ, Delaney CP. Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery. 2011;149(6):830–40.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Ishii M, Mizuguchi T, Harada K, Ota S, Meguro M, Ueki T. Comprehensive review of post-liver resection surgical complications and a new universal classification and grading system. World J Hepatol. 2014;6(10):745–51.
Kobayashi S, Gotohda N, Nakagohri T, Takahashi S, Konishi M, Kinoshita T. Risk factors of surgical site infection after hepatectomy for liver cancers. World J Surg. 2009;33(2):312–7.
Karavokyros I, Orfanos S, Angelou A, et al. Incidence and risk factors for organ/space infection after radiofrequency-assisted hepatectomy or ablation of liver tumors in a single center: more than meets the eye. Front Surg. 2017;4:17.
Nanashima A, Arai J, Oyama S, et al. Associated factors with surgical site infections after hepatectomy: predictions and countermeasures by a retrospective cohort study. Int J Surg. 2014;12(4):310–4.
Hoekstra LT, Wakkie T, Busch OR, Gouma DJ, Beuers U, van Gulik T. Predictors of posthepatectomy ascites with or without previous portal vein embolization. Dig Surg. 2012;29(6):468–74.
Jin S, Fu Q, Wuyun G, Wuyun T. Management of post-hepatectomy complications. World J Gastroenterol. 2013;19(44):7983–91.
Guglielmi A, Ruzzenente A, Conci S, Valdegamberi A, Iacono C. How much remnant is enough in liver resection? Dig Surg. 2012;29(1):6–17.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B.D. Jones, R. Jones, D.F. Dunne, T. Astles, S.W. Fenwick, G.J. Poston and H.Z. Malik declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Jones, B.D., Jones, R., Dunne, D.F. et al. Patient selection and perioperative optimisation in surgery for colorectal liver metastases. Eur Surg 50, 87–92 (2018). https://doi.org/10.1007/s10353-018-0539-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-018-0539-8