Summary
Background
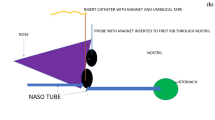
Pressure ulcers related to nasogastric tubes (NGT) are underestimated in clinical practice and rarely reported in the literature. Improper tube fixation around the nostril quickly induces tissue ischemia, possibly leading to skin ulcers and permanent full-thickness lesions. Epidemiological and clinical studies on this subject are lacking.
Methods
This was an observational, cross-sectional study performed in a tertiary-care hospital. Consecutive hospital records of patients undergoing elective surgical procedures under general anesthesia, with an NGT inserted before or during surgery and maintained in place after the operation, were examined. Demographic and clinical data were extracted to investigate factors possibly associated with the occurrence of pressure ulcers of the nostril.
Results
Between 2011 and 2015, 2131 patients underwent elective surgical procedures. The overall prevalence of NGT-induced ulcers was 4.8%, with esophagectomy being the most common index operation. Univariate analysis did not show a statistically significant association between the presence of ulcers and the examined variables, with the exception of operative time (p < 0.012). The prevalence of nostril ulcers statistically differed across operative procedure time (p < 0.001), with a positive significant linear trend (p < 0.001), and lesions were significantly more frequent when the operative procedure lasted longer than 4 h (Confidence interval [CI] 9.2–17.1). Twenty-one (20.5%) patients required plastic surgery consultation due full-thickness lesions with severe cosmetic sequelae.
Conclusions
Nostril pressure ulcers related to NGT are common in clinical practice and necessitate a high index of suspicion and vigilance during the perioperative period. The only factor significantly associated with NGT-induced pressure ulcers was the length of the operative procedure.


Similar content being viewed by others
References
Cheadle WG, Vitale GC, Mackie CR, Cuschieri A. Prophylactic postoperative nasogastric decompression. A prospective study of its requirement and the influence of cimetidine in 200 patients. Ann Surg. 1985;202:361–6.
Nelson R, Tse B, Edward S. Systematic review of prophylactic nasogastric decompression after abdominal operations. Br J Surg. 2005;92:673–80.
Tanguy M, Seguin P, Mallédant Y. Bench-to-bedside review: routine postoperative use of the nasogastric tube – utility or futility? Crit Care. 2007;11:2011.
Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248:189–98.
Black JM, Cuddigan JE, Walko MA, Didier LA, Lander MJ, Kelpe MR. Medical device related pressure ulcers in hospitalized patients. Int Wound J. 2010;7:358–65.
Apold J, Rydrych D. Preventing device-related pressure ulcers: using data to guide statewide changes. J Nurs Care Qual. 2012;27:28–34.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015.
Defloor T, Schoonhoven L. Inter-rater reliability of the EPUAP pressure ulcer classification system using photographs. J Clin Nursing. 2004;13:952–9.
Bass MJ, Phillips LG. Pressure sores. Curr Probl Surg. 2007;44:101–42.
Mistry RC, Vijayabhaskar R, Karimundackal G, Jiwnani S, Pramesh CS. Effect of short-term vs prolonged nasogastric decompression on major postesophagectomy complications. Arch Surg. 2012;147:747–51.
Tsukamoto M, Fujiwara S, Nakamura Y, Yokoyama T. The risk factors of medical device related (MDR) pressure ulcers at the nostril in oral maxillofacial surgery. Eur J Anaesthesiol. 2013;30:236.
Standring S. et al. Gray’s Anatomy, 39th ed. Edinburgh, New York: Elsevier, Churchill Livingstone; 2005.
Banerjee TS, Schneider HJ. Recommended method of attachment of nasogastric tubes. Ann R Coll Surg Engl. 2007;89:529–37.
Klinger M, Maione L, Villani F, Caviggioli F, Forcellini D, Klinger F. Reconstruction of a full-thickness alar wound using an auricular conchal composite graft. Can J Plast Surg. 2010;18:149–51.
Weijs TJ, Kumagai K, Berkelmans GHK, Nieuwenhuijzen GAP, Nilsson M, Luyer MDP. Nasogastric decompression following esophagectomy: a systematic literature review and meta-analysis. Dis Esoph. 2016; doi:10.1111/dote.12530.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Asti, A. Sironi, P. Milito, G. Bonavina, G. Bonitta and L. Bonavina declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Asti, E., Sironi, A., Milito, P. et al. Prevalence and risk factors of nasal pressure ulcers related to nasogastric intubation: an observational study. Eur Surg 49, 171–174 (2017). https://doi.org/10.1007/s10353-017-0476-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-017-0476-y