Summary
Background
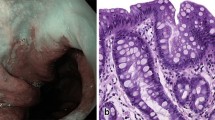
Barrett’s esophagus (BE) is the morphological consequence of gastroesophageal reflux disease (GERD). Via low- and high-grade dysplasia, nondysplastic Barrett’s esophagus (NDBE) may progress to cancer (0.1–0.6 % annual risk). We aim to summarize the impact of radiofrequency ablation (RFA) for the elimination of BE and cancer prevention.
Methods
This PUB MED search included 136 papers on the pathophysiology, diagnosis, and therapy (RFA, antireflux surgery) of BE £ T1a.
Results
The reflux of gastric acid and bile mediate a complex neurohumoral response within the esophageal mucosa, which orchestrates the formation of NDBE, dysplasia, and cancer. RFA effectively eliminates NDBE, dysplasia, and flat T1a cancer. Following 1–6 treatment sessions and 1–3.5 years follow-up, RFA for dysplastic BE effectively eliminates dysplasia and NDBE in > 80 and > 60 % of the cases, respectively, and mediates the development of a mucosa without genetic abnormalities. After 1–3 treatments for NDBE and 5 years follow-up, RFA eradicates NDBE in 92 % of the cases. NDBE expresses the genetic abnormalities of dysplasia and cancer and shares the same cancer risk as colonic polyps. Therefore, within clinical trials, RFA for NDBE should be offered to persons with NDBE and a risk profile, which predisposes them for cancer development (family history, GERD > 10 years, etc.). Antireflux surgery increases the yield of RFA for NDBE.
Conclusions
RFA (± endoscopic resection) is recommended for the elimination of BE with dysplasia and early cancer (T1a). Larger tumors are treated by surgical resection. The biological and genetic properties of NDBE justify the examination of RFA for this indication within clinical trials. Future studies will have to elucidate the combination of RFA, antireflux surgery, and medical therapy (PPI, statins, nonsteroidal antiinflammatory drugs) for cancer prevention.









Similar content being viewed by others
References
Becher A, Dent J. Systematic review: ageing and gastro-oesophageal reflux disease symptoms, esophageal function and reflux oesophagitis. Aliment Pharmacol Ther. 2011;33(4):442–54.
Kamolz T, Velanovich V. The impact of disease and treatment on health-related quality of life in patients suffering from GERD. In: Granderath FA, Kamolz T, Pointner R, editors. Gastroesophageal reflux disease, principles of disease, diagnosis and treatment. New York: Springer Wien; 2006. pp. 287–98.
Chandrasoma PT. Columnar lined esophagus: what it is and what it tells us. Eur Surg. 2006;38/3:197–209.
Lenglinger J, Eisler M, Wrba F, et al. Update: histopathology-based definition of gastroesophageal reflux disease and Barrett’s esophagus. Eur Surg. 2008;40/4:165–75.
Lenglinger J, Izay B, Eisler M, et al. Barrett’s esophagus: size of the problem and diagnostic value of a novel histopathology classification. Eur Surg. 2009;41/1:26–39.
Goldblum JR. Controversies in the diagnosis of Barrett esophagus ad Barrett-related dysplasia. Arch Pathol Lab Med. 2010;134:1479–84.
Odze RD. What the gastroenterologist needs to know about the histology of Barrett’s esophagus. Curr Opin Gastroenterol. 2011 27(4):389–96.
Chandrasoma P, Wijetunge S, DeMeester S, et al. Columnar-lined esophagus without intestinal metaplasia has no proven risk of adenocarcinoma. Am J Surg Pathol. 2012 Jan;36(1):1–7.
Hvid-Jensen F, Pedersen L, Mohr Drewes A, et al. Incidence of adenocarcinoma among patients with Barrett’s esophagus. N Engl J Med. 2011;365:1375–83.
Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett’s oesophagus: a meta-analysis. Gut. 2012 Jul;61(7):970–6.
De Jonge PJ, van Blankenstein M, Looman CW, et al. Risk of malignant progression in patients with Barrett’s oesophagus: Dutch nationwide cohort study. Gut. 2010;59(8):1030–6.
Sharma P, Falk GW, Weston AP, et al. Dysplasia and cancer in a large multicenter cohort of patients with Barrett’s esophagus. Clin Gastroenterol Hepatol. 2006;4:566–72.
Wani S, Puli SR, Shaheen NJ, et al. Esophageal adenocarcinoma in Barrett’s esophagus after endoscopic ablative therapy: a meta-analysis and systemic review. Am J Gastroenterol. 2009;104:502–13.
Kastelein F, Spaander MCW, Biermann K, et al. Nonsteroidal anti-inflammatory drugs and statins have chemopreventive effects in patients with Barrett’s esophagus. Gastroenterology. 2011 Dec;141(6):2000–8.
Fleischer DE, Odze R, Overholt BF, et al. The case for endoscopic treatment of non-dysplastic and low grade dysplastic Barrett’s esophagus. Dig Dis Sci. 2010;55:1918–31.
Spechler SJ, Fitzgerald RC, Prasad GA, Wang KK. History, molecular mechanism, and endoscopic treatment of Barrett’s esophagus. Gastroenterology. 2010;138(3):854–69.
Spechler SJ. Screening and surveillance for Barrett’s esophagus—an unresolved dilemma. Nat Clin Pract Gastroenterol & Hepatol. 2007;4(9):470–1.
Manner H, May A, Pech O, et al. Early Barrett’s carcinoma with “low risk” submucosal invasion: long-term results of endoscopic resection with a curative intent. Am J Gastroenterol. 2008;103:2589–97.
Zehetner J, DeMeester SR, Hagen JA, et al. Endoscopic resection and ablation versus esophagectomy for high-grade dysplasia and intramucosal adenocarcinoma. J Thorac Cardiovasc Surg. 2011;141:39–47.
Gordon LG, Eckermann S, Hirst NG, et al. Healthcare resource use and medical cost for the management of oesophageal cancer. Br J Surg. 2011;98(11):1589–98.
Triadafilopoulos G. Proton pump inhibitor in Barrett’s esophagus: pluripotent but controversial. Eur Surg. 2008;40/2:58–65.
Chandrasoma P, Wijetunge S, Ma Y, DeMeester S, et al. The dilated distal esophagus: a new entity that is the pathologic basis of early gastroesophageal reflux disease. Am J Surg Pathol. 2011;35(12):1873–81.
Chandrasoma P, Wijetunge S, DeMeester SR, et al. The histologic squamo-oxyntic gap: an accurate and reproducible diagnostic marker of gastroesophageal reflux disease. Am J Surg Pathol. 2010;34(11):1574–81.
Glickman JN, Spechler SJ, Souza RF, et al. Multilayered epithelium in mucosal biopsy specimens from the gastroesphageal junction region is a histologic marker of gastroesophageal reflux disease. Am J Surg Pathol. 2009;33:818–25.
Öberg S, Peters JH, DeMeester TR, et al. Inflammation and specialized intestinal metaplasia of cardiac mucosa is a manifestation of gastroesophageal reflux disease. Ann Surg. 1997;226(4):522–32.
Singh R, Yi SLC, Sethi S. Advanced endoscopic imaging in Barrett’s esophagus: a review on current practice. World J Gastroenterol. 2011;17(38):4271–6.
Coco DP, Goldblum JR, Hornick JL, et al. Interobserver variability in the diagnosis of crypt dysplasia in Barrett esophagus. Am J Surg Pathol. 2011;35:45–54.
Bennett AE, Goldblum JR, Odze R. Inflammatory disorders of the esophagus. In: Odze R, Goldblum JR, editors. Surgical pathology of the GI tract, liver, biliary tract, an pancreas. 2nd ed. Philadelphia: Saunders Elsevier; 2009. pp. 256–64.
Siewert JR, Stein HJ, Feith M. Adenocarcinoma of the esophago-gastric junction. Scand J Surg. 2006;95(4):260–9.
Schoppmann SF, Prager G, Langer FB, et al. Open versus minimally invasive esophagectomy: a single-center case controlled study. Surg Endosc. 2010;24(12):3044–53.
Curvers WL, ten Kate FJ, Krishnadad KK, et al. Low-grade dysplasia in Barrett’s esophagus: overdiagnosed and underestimated. Am J Gastroenterol. 2010;105(7):1523–30.
Ringhofer C, Lenglinger J, Izay B, et al. Histopathology of the endoscopic esophagogastric junction in patients with gastroesophageal reflux disease. Wien Klin Wochenschr. 2008;120/11:350–9.
Mueller J, Werner M, Stolte M. Barrett’s esophagus: histopathologic definitions and diagnostic criteria. World J Surg. 2004;28(2):148–54.
Müller M, Gockel I, Hedwig P, et al. Is the Schatzki ring a unique esophageal entity? World J Gastroenterol. 2011;17(23):2838–43.
Sharma P, Dent J, Armstrong D, et al. The development and validation of an endoscopic grading system for Barrett’s esophagus: the Prague C & M ctriteria. Gastroenterology. 2006;131(5):1392–9.
Oezcelik A, DeMeester SR. General anatomy of the esophagus. Thorac Surg Clin. 2011;21(2):289–97.
Ayazi S, Tanhankar A, DeMeester SR, et al. The impact of gastric distension on the lower esophageal sphincter and its exposure to acid gastric juice. Ann Surg. 2010;252:57–62.
Bredenoord AJ. High-resolution manometry—bliss upon bliss for the esophagology? Eur Surg. 2007;39/3:176–3.
Savarino E, Gemignani L, Pohl D, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34(4):476–86.
Atasoy S, Mateus D, Meining A, et al. Targeted optical biopsies for surveillance endoscopies. Med Image Comput Assist Interv. 2011;14(3):83–90.
Wijetunge S, Ma Y, DeMeester S, et al. Association of adenocarcinoma of the distal esophagus, “gastroesophageal junction”, and “gastric cardia” with gastric pathology. Am J Surg Pathol. 2010;34(10):1521–7.
Malfertheiner P, Nocon M, Vieth M, et al. Evolution of gastro-oesophageal reflux disease over 5 years under routine medical care—the ProGERD study. Aliment Pharmacol Ther. 2012;35(1):154–64.
Oh SD, DeMeester SR. Pathophysiology and treatment of Barrett’s esophagus. World J Surg. 2010;16(30):3762–72.
Rex DK, Cummings OW, Shaw M, et al. Screening for Barrett’s esophagus in colonoscopy patients with and without heartburn. Gastroenterology. 2003;125:1670–7.
Gerson LB, Shetler K, Triadafilopoulos G. Prevalence of Barrett’s esophagus in asymptomatic individuals. Gastroenterology. 2002;123:461–7.
Ronkainen J, Aro P, Storskrubb, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopy study. Gastroenterology. 2005;129:1825–31.
Hayeck TJ, Kong CY, Spechler SJ, et al. The prevalence of Barrett’s esophagus in the US: estimates from a simulation model confirmed by SEER data. Dis Esoph. 2010;23(6):451–7.
Thrift AP, Pandeya N, Smith KJ, et al. Helicobacter pylori infection and the risks of Barrett’s oesophagus: a population-based case-control study. Int J Cancer. 2012 May 15;130(10):2407–16.
Shaheen NJ, Sharma P, Overholt BF, et al. Radiofrequency ablation in Barrett’s esophagus with dysplasia. N Engl J Med. 2009;360:2277–88.
Rieder F, Biancani P, Harnett K, et al. Inflammatory mediators in gastroesophageal reflux disease: impact on esophageal motility, fibrosis, and carcinogenesis. Am J Physiol. 2010;298:G571–81.
Goldman A, Chen HD, Roesly HB, et al. Characterization of squamous esophageal cells resistant to bile acids at acidic pH: implication for Barrett’s esophagus pathogenesis. Am J Physiol. 2010;300:G292–302.
Huo X, Juergens S, Zhang X, et al. Deoxycholic acid causes DNA damage while inducing apoptotic resistance through NF-kB activation in benign Barrett’s epithelialc ells. Am J Physiol. 2011;301:G278–86.
Zhang HY, Hormi Carver K, Zhang X, et al. In benign Barrett’s epithelial cells, acid exposure generates reactive oxygen species that cause DNA double strand breaks. Cancer Res. 2009;69:9083–9.
Zhang HY, Zhang Q, Zhang X, et al. Cancer-related inflammation and Barrett’s carcinogenesis: interleukin-6 and STAT3 mediate apoptotic resistance in transformed Barrett’s cells. Am J Physiol. 2011;300:G454–60.
Tobey NA, Hosseini SS, Argote CM, et al. Dilated intercellular spaces and shunt permeability in nonerosive acid-damaged esophageal epithelium. Am J Gastroenterol. 2004;99(1):13–22.
Barlow WJ, Orlando RC. The pathogenesis of heartburn in nonerosive reflux disease: a unifying hypothesis. Gastroenterology. 2005;128(3):771–8.
Souza RF, Huo X, Mittal V, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology. 2009;137:1776–84.
Sarosi G, Brown G, Jaiswal K, et al. Bone marrow progenitor cells contribute to esophageal regeneration and metaplasia in a rat model of Barrett’s esophagus. Dis Esoph. 2008;21:43–50.
Wang X, Ouyang H, Yamamoto Y, et al. Residual embryonic cells as precursors of a Barrett’s-like metaplasia. Cell. 2011;145:1023–35.
Bobryshev YV, Freeman AK, Botelho NK, et al. Expression of the putative stem cell marker Musashi-1 in Barrett’s esophagus and esophageal adenocarcinoma. Dis Esoph. 2010;23:580–9.
Souza RF, Schwartz RE, Mashimo H. Esophageal stem cells and 3D-cell culture models. Ann NY Acad Sci. 2011;1232:316–22.
Vega KJ, May R, Sureban SM, et al. Identification of the putative intestinal stem cell marker DCAMKL-1 in Barrett’s esophagus and esophageal adenocarcinoma. J Gastroenterol Hepatol. 2012 Apr;27(4):773–80.
Milano F, van Baal JW, Buttar NS, et al. Bone morphogenetic protein 4 expressed in esophagitis induces a columnar phenotype in esophageal squamous cells. Gastroenterology. 2007;132:2412–21.
Castillo D, Puig S, Iglesias M, et al. Activation of the BMP4 pathway and early expression of CDX2 characterize non-specialized columnar metaplasia in a human model of Barrett’s esophagus. J Gastroinest Surg. 2012 Feb;16(2):227–37.
Huo X, Zhang HY, Zhang X, et al. Acid and bile salt-induced CDX2 expression differs in esophageal squamous cells from patients with and without Barrett’s esophagus. Gastroenterology. 2010;139:194–203.
Hayes S, Ahmed S, Clark P. Immunohistochemical assessment for CDx2 expression in the Barrett metaplasia-dysplasia-adenocarcinoma sequence. J Clin Pathol. 2011;64:110–3.
McIntire MG, Soucy G, Vaughan TL, et al. MUC2 is a highly specific marker of goblet cell metaplasia in the distal esophagus and the gastroesophageal junction. Am J Surg Pathol. 2011;35:1007–13.
Yamanaka Y, Shiotani A, Fujimura Y, et al. Expression of sonic hedgehog (SHH) and CDX2 in the columnar epithelium of the lower esophagus. Dig Liv Dis. 2011;43:54–9.
DeMeester SR. Reflux, Barrett’s and adenocarcinoma of the esophagus: can we disrupt the pathway? J Gastrointest Surg. 2010;14:941–54.
Riegler M. Barrett’s esophagus: filling the gap. Eur Surg. 2010;42/1:1–3.
Heijmans J, Van Den Brink GR. Morphogens and the parietal cell: shaping up acid secretion. Gastroenterology. 2010;139(6):1830–3.
Kazumori H, Ishihara S, Takahashi Y, et al. Roles of Krüppel-like factor 4 in oesophageal epithelial cells in Barrett’s espithelium development. Gut. 2011;60:608–17.
Fitzgerald RC, Omary MB, Triadafilopoulos G. Dynamic effects of acid on Barrett’s esophagus. An ex vivo proliferation and differentiation model. J Clin Invest. 1996;98:2120–8.
Goldman A, Shahidullah M, Goldman D, et al. A novel mechanism of acid and bile-induced DNA damage involving Na+/H+ exchanger: implication for Barrett’s esophagus. Gut. 2010 Dec;59(12):1606–16.
Zhang HY, Spechler SJ, Souza RF. Esophageal adenocarcinoma arising in Barrett’s esophagus. Cancer Lett. 2009;275:170–7.
Smith E, Kelly JJ, Ruskiewicz AR, et al. The effect of long-term control of reflux by fundoplication on aberrant deoxyribonucleic acid methylation in patients with Barrett’s esophagus. Ann Surg. 2010;252:63–9.
Liu W, Hahn H, Odze RD, Goyal RK. Metaplastic esophageal columnar epithelium without goblet cells shows DNA content abnormalities similar to goblet cell-containing epithelium. Am J Gastroetnerol. 2009;104(4):816–24.
Hahn HP, Blount PL, Ayub K, et al. Intestinal differentiation in metaplastic, nongoblet columnar epithelium in the esophagus. Am J Surg Pathol. 2009;33(7):1006–15.
Theodorou D, Ayazi S, DeMeester SR, et al. Intraluminal pH and goblet cell density in Barrett’s esophagus. J Gastrointest Surg. 2012 Mar;16(3):469–74.
Theisen J, Stein HJ, Feith M, et al. Preferred location for the development of esophageal adenocarcinoma within a segment of intestinal metaplasia. Surg Endosc. 2006;20(2):235–8.
Öberg S, Johansson J, Wenner J, Walther B. Metaplastic columnar mucosa in the cervical esophagus after esophagectomy. Ann Surg. 2002;235(3):338–45.
Dresner SM, Griffin SM, Bennett MK, et al. Human model of duodenogastro-oesophageal reflux in the development of Barrett’s metaplasia. Br J Surg. 2003;90:1120–8.
Franchimont D, Covas A, Brasseur C, et al. Newly developed Barrett’s esophagus after subtotal esophagectomy. Endoscopy. 2003;35(10):850–3.
Lord RVN, Wickramasinghe K, Johansson JJ, et al. Cardiac mucosa in the remnant esophagus after esophagectomy is an acquired epithelium with Barrett’s-like features. Surgery. 2004;136:633–40.
Peitz U, Vieth M, Pross M, et al. Cardia-type metaplasia arising in the remnant esophagus after cardia resection. Gastrointest Endosc. 2004;59:810–7.
Peitz U, Vieth M, Ebert M, et al. Small-bowel metaplasia arising in the remnant esophagus after esophagogastrostomy—a retrospective study in patients with a history of total gastrectomy. Am J Gastroenterol. 2005;100:2062–70.
Saadi A, Shannon NB, Lao-Sirieix, et al. Stromal genes discriminate preinvasive from invasive disease, predict outcome, and highlight inflammatory pathways in digestive cancers. Proc Natl Acad Sci U S A. 2010;107(5):2177–82.
Arora G, Basra S, Roorda AK, Triadafilopoulos G. Radiofrequency ablation for Barrett’s esophagus. Eur Surg. 2009;41/1:19–25.
Moayyedi P, Burch N, Akhtar-danesh N, et al. Mortality rates in patients with Barrett’s esophagus. Aliment Pharmacol Ther. 2008;27:316–20.
Anderson LA, Murray LJ, Murphy SJ, et al. Mortality in Barrett’s oesophagus: results from a population based study. Gut. 2003;52:1081–4.
Pouw RE, Sharma VK, Bergman JJ, Fleischer DE. Radiofrequency ablation for total Barrett’s eradication: a description of the endoscopic technique, its clinical results and future prospects. Endoscopy. 2008;40:1033–40.
Fleischer DE, Overholt BF, Sharma VK, et al. Endoscopic ablation of Barrett’s esophagus: a multicenter study with 2.5-year follow up. Gastrointest Endosc. 2008;68(5):867–76.
Lyday WD, Corbett FS, Kuperman DA, et al. Radiofrequency ablation of Barrett’s esophagus: outcomes of 429 patients from a multicenter community practice registry. Endoscopy. 2010;42:272–8.
Fleischer DE, Overholt BF, Sharma VK, et al. Endoscopic radiofrequency ablation for Barrett’s esophagus: 5-year outcomes from a prospective multicenter trial. Endoscopy. 2010;42(10):781–9.
Shaheen NJ, Overholt BF, Sampliner RE, et al. Durability of radiofrequency ablation in Barrett’s esophagus with dysplasia. Gastroenterology. 2011;141:460–8.
Van Vilsteren FGI, Pouw RE, Seewald S, et al. Stepwise radical endoscopic resection versus radiofrequency ablation for Barrett’s oesophagus with high-grade dysplasia or early cancer: a multicenter randomized trial. Gut. 2011;60(6):765–73.
Shaheen NJ, Peery AF, Hawes RH, et al. Quality of life following radiofrequency ablation of dysplastic Barrett’s esophagus. Endoscopy. 2010;42:790–9.
Alvarez Herrero L, van Vilsteren FGI, Pouw RE, et al. Endoscopic radiofrequency ablation combined with endoscopic resection for early neoplasia in Barrett’s esophagus longer than 10 cm. Gastrointest Endosc. 2011;73:682–90.
Ganz RA, Overholt BF, Sharma VK, et al. Circumferential ablation of Barrett’s esophagus that contains high-grade dysplasia: a U.S. multicenter registry. Gastrointest Endosc. 2008;68:35–40.
Inadomi JM, Somsouk M, Madanick RD, et al. A cost-utility analysis of ablative therapy for Barrett’s esophagus. Gastroenterology. 2009;136(7):2101–14.
Gray NA, Odze RD, Spechler SJ. Buried metaplasia after endoscopic ablation of Barrett’s esophagus: a systematic review. Am J Gastroenterol. 2011;106(11):1899–908.
Rabeneck L, Paszat LF, Hilsden RJ, et al. Bleeding and perforation after outpatient colonoscopy and their risk factors in usual clinical practice. Gastroenterology. 2008;135(6):1899–1906.
Merchea A, Cullinane DC, Sawyer MD, et al. Esophagogastroduodenoscopy-associated gastrointestinal perforations: a single center experience. Surgery. 2010;148(4):876–80.
Kelty CJ, Cough MD, van Wyk Q, et al. Barrett’s oesophagus: intestinal metaplasia is not essential for cancer risk. Scand J Gastroenterol. 2007;42:1271–4.
Gatenby PAC, Ramus JR, CAygill CPJ, et al. Relevance of the detection of intestinal metaplasia in non-dysplastic columnar-lined oesophagus. Scand J Gastroenterol. 2008;43:524–30.
El-Serag HB. Routine polypectomy for colorectal polyps and ablation for Barrett’s esophagus are intellectually the same. Gastroenterology. 2011;140:386–8.
Horner MJ, et al. SEER cancer statistics review, 1975-2006, National Cancer Institute. Bethesda, MD. http://seer.cancer.gov/csr/1975_2006, based on November 2008 SEER data submission, posted to the SEER web site. 2009.
Abu-Sneineh A, Tam W, Schoeman M, et al. The effects of high-dose esomeprazole on gastric and oesophageal acid exposure and molecular markers in Barrett’s oesophagus. Aliment Pharm Ther. 2010;32:1023–30.
Pouw RE, Gondrie JJ, Rygiel AM, et al. Properties of the neosquamous epithelium after radiofrequency ablation of Barrett’s esophagus containing neoplasia. Am J Gastroenterol. 2009;104(6):1366–73.
Beaumont H, Gondrie JJ, Pouw RE, et al. Stepwise radiofrequency ablation of Barrett’s esophagus preserves esophageal inner diameter, compliance, and motility. Endoscopy. 2009;41:2–8.
Semlitsch T, Jeitler K, Schoefl R, et al. A systematic review of the evidence for radiofrequency ablation for Barrett’s esophagus. Surg Endosc. 2010;24(12):2935–43.
Kahrilas P. The problems with surveillance of Barrett’s esophagus. N Engl J Med. 2010;365(15):1375–83.
Sikkema M, Looman CWN, Steyerberg EW, et al. Predictors for neoplastic progression in patients with Barrett’s esophagus: a prospective cohort study. Am J Gastroenterol. 2011;106(7):1231–8.
Rubenstein JH, Scheiman JM, Sadeghi S, et al. Esophageal adenocarcinoma incidence in individuals with gastroesophageal reflux: synthesis and estimates from population studies. Am J Gastroenterol. 2011;106(2):254–60.
Wiseman EF, Ang YS. Risk factors for neoplastic progression in Barrett’s esophagus. World J Gastroenterol. 2011;17(32):3672–83.
Rubenstein JH, Mattek N, Eisen G. Age- and sex-specific yield of Barrett’s esophagus by endoscopy indication. Gastrointest Endosc. 2010;71:21–7.
Granderath FA, Kamolz T, Schweiger UM, et al. Long-term results of laparoscopic antireflux surgery. Surgical outcome and analysis of failure after 500 laparoscopic procedures. Surg Endosc. 2002;16:753–7.
Wykypiel H, Wetscher GJ, Klingler P, Glaser K. The Nissen fundoplication: indication, technical aspects and postoperative outcome. Langenbecks Arch Surg. 2005;390:495–502.
Vallböhmer D, DeMeester SR, Oh DS, et al. Antireflux surgery normalizes cyclooxygenase-2 expression in squamous epithelium of the distal esophagus. Am J Gastroenterol. 2006;101(7):1458–66.
Koch OO, Kaindlsdorfer A, Antoniou SA, et al. Laparoscopic Nissen versus Toupet fundoplication: objective and subjective results of a prospective randomized trial. Surg Endosc. 2012 Feb;26(2):413–22.
Mabrut JY, Baulieux J, Adham M, et al. Impact of antireflux operation on columnar lined esophagus. J Am Coll Surg. 2003;196(1):60–7.
Gurski RR, Peters JH, Hagen JA, et al. Barrett’s esophagus can and does regress after antireflux surgery: a study of prevalence and predictive features. J Am Coll Surg. 2003;196(5):706–12.
Csendes A, Braghetto I, Burdiles P, et al. Late results of the surgical treatment of 125 patients with short-segment Barrett esophagus. Arch Surg. 2009;144(10):921–7.
Parrilla P, Martinez de Haro LF, Ortiz A, et al. Long-term results of a randomized prospective study comparing medical and surgical treatment of Barrett’s esophagus. Ann Surg. 2003;237(3):291–8.
Rossi M, Barreca M, de Bartoli N, et al. Efficacy of Nissen fundoplication versus medical therapy in the regression of low-grade dysplasia in patients with Barrett’s esophagus. Ann Surg. 2006;243:58–63.
Zaninotto G, Parente P, Salvador R, et al. Long-term follow-up of Barrett’s epithelium: medical versus antireflux surgical therapy. J Gastrointest Surg. 2012 Jan;16(1):7–14.
Chang EY, Morris CD, Seltman AK, et al. The effect of antireflux surgery on esophageal carcinogenesis in patients with Barrett esophagus: a systematic review. Ann Surg. 2007;246(1):11–21.
Theisen J, Peters JH, Fein M, et al. The mutagenic potential of duodenoesophageal reflux. Ann Surg. 2005;241:63–8.
McQuaid KR, Laine L, Fennerty MB, et al. Systematic review: the role of bile acids in the pathogenesis of gastro-oesophageal reflux disease and related neoplasia. Aliment Pharmacol Ther. 2011;34(2):146–65.
Lagergren J, Bergström R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Eng J Med. 1999;340(11):825–31.
Lagergren J, Ye W, Lagegren P, Lu Y. The risk of esophageal adenocarcinoma after antireflux surgery. Gastroenterology. 2010;138(4):1297–301.
Kauttu TME, Rantanen TK, Sihvo EI, et al. Esophageal adenocarcinoma arising after antireflux surgery: a population-based analysis. Eur J Cardiothor Surg. 2011;40:1450–4.
Hubbard N, Velanovich V. Endoscopic endoluminal radiofrequency ablation of Barrett’s esophagus in patients with fundoplication. Surg Endosc. 2007;21:625–8.
dos Santos RS, Bizekis C, Ebright M, et al. Radiofrequency ablation fro Barrett’s esophagus and low grade dysplasia in combination with antireflux procedure: a new paradigm. J Thorac Cardiovasc Surg. 2010;139(3):713–6.
O’Connell K, Velanovich V. Effects of Nissen fundplication on endoscopic endoluminal radiofrequency ablation of Barrett’s esophagus. Surg Endosc. 2011;25(3):830–4.
Goers TA, Leao P, Cassera MA, et al. Concomitant endoscopic radiofrequency ablation and laparoscopic reflux operative results in more effective and efficient treatment of Barrett’s esophagus. J Am Coll Surg. 2011;213(4):486–92.
Bhat S, Coleman HG, Yousef F, et al. Risk of malignant progression in Barrett’s esophagus patients: results from a large population-based study. J Natl Cancer Inst. 2011;103:1049–57.
Conflict of interest
The authors declare that there is no actual or potential conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mesteri, I., Beller, L., Fischer-See, S. et al. Radiofrequency ablation of Barrett’s esophagus and early cancer within the background of the pathophysiology of the disease. Eur Surg 44, 366–382 (2012). https://doi.org/10.1007/s10353-012-0183-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-012-0183-7