Summary
Background
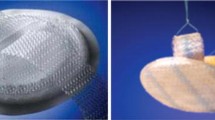
Laparoscopic hernioplasty is the method of choice for the repair of certain types of incisional and ventral hernias; however, complications from intraperitoneally implanted inappropriate meshes can be life threatening. On the other hand, the appropriate meshes are costly and that limit their routine use. The aim of these experiments was to create a simple mesh which generates adhesions in the abdominal wall but prevents adhesion formations intra-abdominally.
Methods
The behaviour of different materials covering routinely used macroporous meshes were investigated in a rabbit model (n = 48) in which two disks of meshes were implanted in the abdominal wall in a way that the covered side faced the abdominal cavity. Depending on the mesh and the material covering it, the rabbits were divided into four groups of 12. The animals from each group were studied at 30, 60, 90 and 120 days to determine the presence and degree of adhesion formation macroscopically.
Results
Non-coated polypropylene mesh caused massive adhesions, but coating with silicone-layer adhesion formation was highly decreased.
Conclusions
Intraperitoneal implantation of silicon impregnated low-weight polypropylene mesh decreased the incidence of adhesions. Use of silicone-covered mesh may provide a cheap alternative means for laparoscopic hernia repair.





Similar content being viewed by others
References
Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–1.
Sugerman HJ, Kellum JM Jr., Reines HD, et al. Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg. 1996;171:80–4.
Read RC, Yoder G. Recent trends in the management of incisional herniation. Arch Surg. 1989;124:485–8.
Manninen MJ, Lavonius M, Perhoniemi VJ. Results of incisional hernia repair: a retrospective study of 172 unselected hernioplasties. Eur J Surg. 1991;157:29–31.
Luijendijk RW, Hop WCJ, van den Tol P, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343:392–8.
Paul A, Korenkov M, Peters S, et al. Unacceptable results of the Mayo procedure for repair of abdominal incisional hernias. Eur J Surg. 1998;164:361–7.
Anthony T, Bergen PC, Kim LT, et al. Factors affecting recurrence following incisional herniorrhaphy. World J Surg. 2000;24:95–101.
Leber GE, Garb JL, Alexander AI, Reed WP. Long-term complications associated with prosthetic repair of incisional hernias. Arch Surg. 1998;133:378–82.
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240(4):578–83; discussion 583–5.
Baracs J, Takacs I, Horvarth S, Horváth Örs P, Weber G. Higher recurrence rate at sublay than onlay mesh reconstruction in abdominal hernias: five-years results of a randomised, multicentric clinical trial. Br J Surg. 2009;96(S5):8.
McCormack K, Scott NW, Go PM, Ross S, Grant AM. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003:CD001785.
Wéber G, Baracs J, Horváth OP. “Onlay” mesh provides significantly better results than “sublay” reconstruction. Prospective randomized multicenter study of abdominal wall reconstruction with sutures only, or with surgical mesh—results of a five-years follow-up. Magy Seb. 2010;63(5):302–11.
Adetayo OA, Salcedo SE, Bahjri K, Gupta SC. A meta-analysis of outcomes using acellular dermal matrix in breast and abdominal wall reconstructions: event rates and risk factors predictive of complications. Ann Plast Surg. 2011. Epub ahead of print.
Liu F, Li J. Repair of large abdominal wall defects using the Proceed™ surgical mesh with open intra-peritonium onlay method. Saudi Med J. 2011;32(5):504–9.
Ghazi B, Deigni O, Yezhelyev M, Losken A. Current options in the management of complex abdominal wall defects. Ann Plast Surg. 2011 May;66(5):488–92.
Morris-Stiff GJ, Hughes LE. The outcomes of nonabsorbable mesh placed within the abdominal cavity: literature and clinical experience. J Am Cool Surg. 1998;186:352–67.
Novotný T, Jeřábek J, Veselý K, Staffa R, Dvořák M, Cagaš J. Evaluation of a knitted polytetrafluoroethylene mesh placed intraperitoneally in a New Zealand white rabbit model. Surg Endosc. 2012;26(7):1884–91.
Raptis DA, Vichova B, Breza J, Skipworth J, Barker S. A comparison of woven versus nonwoven polypropylene (PP) and expanded versus condensed polytetrafluoroethylene (PTFE) on their intraperitoneal incorporation and adhesion formation. J Surg Res. 2011;169(1):1–6.
Franz MG. The biology of hernia formation. Hernia. 2006;10(6):462–71.
Carbajo MA, Martin del Olmo JC, Blanco JI, et al Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc. 1999;13:250–2.
Heniford BT, Ramshaw BJ. Laparoscopic ventral hernia repair—a report of 100 consecutive cases. Surg Endosc. 2000;14:419–23.
Junge K, Klinge U, Prescher A, Giboni P, Niewiera M, Schumpelick V. Elasticity of the anterior abdominal wall and impact for reparation of incisional hernias using mesh implants. Hernia. 2001;5(3):113–8.
Lynen Jansen P, Mertens PR, Klinge U, Schumpelick V. The biology of hernia formation. Surgery. 2004;136(1):1–4.
Bellón JM, Garcia-Carranza A, Jurado F, Garcia-Honduvilla N, Carrera-San Martin A, Buján J. Peritoneal regeneration after implant of a composite prosthesis in the abdominal wall. World J Surg. 2001;25:147–52.
Dinsmore RC, Calton WC. Prevention of adhesions to polypropylene mesh in a rabbit model. Am Surg. 1999;65:383–7.
van’t Riet M, de Vos van Steenwijk PJ, Bonthuis F, Marquet RL, Steyerberg EW, Jeekel J, Bonjer HJ. Prevention of adhesion to prostetic mesh comparison of different barriers using an incisional hernia model. Ann Surg. 2003;237:123–8.
Nagy J. Production and medical use of biocompatible materials. (Biokompatibilis anyagok orvostechnikai alkalmazása és előállításuk.—Original book in Hungarian) 2011.
Shintani H, Nakamura A. Analysis of a carcinogen, 4,4′-methylenedianiline, from thermosetting polyurethane during sterilization. J Anal Toxicol. 1989;13(6):354–7.
Takács I, Horváth S, Balatonyi B, Jávor S, Molnár A, Gáspár S, Hajós R, Meczker A, Lantos J, Roth E, Wéber G. Tissue integration of various silicone-coated polypropylene surgical mesh. Magy Seb. 2010;63(5):340–6.
Conflict of interest
The authors declare that there is no actual or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baracs, J., Takacs, I., Sajjadi, S. et al. Which mesh is appropriate for laparoscopic use? Prevention of adhesions to macroporous mesh, a rabbit model. Eur Surg 44, 319–324 (2012). https://doi.org/10.1007/s10353-012-0154-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-012-0154-z