Abstract
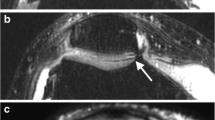
Magnetic resonance imaging (MRI) is the modality of choice for visualizing and quantifying articular cartilage thickness. However, difficulties persist in MRI of subchondral bone using spoiled gradient-echo (SPGR) and other gradient-echo sequences, primarily due to the effects of chemical-shift artifact. Fat-suppression techniques are often used to reduce these artifacts, but they prevent measurement of bone thickness. In this report, we assess the magnitude of chemical-shift effects (phase-cancellation and misregistration artifacts) on subchondral bone and cartilage thickness measurements in human femoral heads using a variety of pulse sequence parameters. Phase-cancellation effects were quantified by comparing measurements from in-phase images (TE=13.5 ms) to out-of-phase images (TE=15.8 ms). We also tested the assumption of the optimal in-phase TE by comparing thickness measures at small variations on TE (13.0, 13.5 and 14.0 ms). Misregistration effects were quantified by comparing measurements from water+fat images (water-only+fat-only images) to the measurements from in-phase (TE=13.5) images. A correction algorithm was developed and applied to the in-phase measurements and then compared to measurements from water+fat images. We also compared thickness measurements at different image resolutions. Results showed that both phase-cancellation artifact and misregistration artifact were significant for bone thickness measurement, but not for cartilage thickness measurement. Using an in-phase TE and correction algorithm for misregistration artifact, the errors in bone thickness relative to water+fat images were non-significant. This information may be useful for developing pulse sequences for optimal imaging of both cartilage and subchondral bone.



Similar content being viewed by others
References
Peterfy CG, van Dijke CF, Janzen DL, et al (1994) Quantification of articular cartilage in the knee with pulsed saturation transfer subtraction and fat-suppressed MR imaging: optimization and validation. Radiology 192:485–91
Disler DG, Marr DS, Rosenthal DI (1994) Accuracy of volume measurements of computed tomography and magnetic resonance imaging phantoms by three-dimensional reconstruction and preliminary clinical application. Invest Radiol 29:739–45
Dupuy DE, Spillane RM, Rosol MS, et al (1996) Quantification of articular cartilage in the knee with three-dimensional MR imaging. Acad Radiol 3:919–24
Eckstein F, Gavazzeni A, Sittek H, et al (1996) Determination of knee joint cartilage thickness using three-dimensional magnetic resonance chondro-crassometry (3D MR-CCM). Magn Reson Med 36:256–65
Hodler J, Trudell D, Pathria MN, Resnick D (1992) Width of the articular cartilage of the hip: quantification by using fat-suppression spin-echo MR imaging in cadavers. Am J Roentgenol 159:351–5
McGibbon CA, Palmer WE, Krebs DE (1998) A general computing method for spatial cartilage thickness from co-planar MRI. Med Eng Phys 20:169–76
Disler DG, McCauley TR, Wirth CR, Fuchs MD (1995) Detection of knee hyaline cartilage defects using fat-suppressed three-dimensional spoiled gradient-echo MR imaging: comparison with standard MR imaging and correlation with arthroscopy. Am J Roentgenol 165:377–82
Yao L, Sinha S, Seeger LL (1992) MR imaging of joints: analytic optimization of GRE techniques at 1.5 T. Am J Roentgenol 158:339–45
Dequeker J, Mokassa L, Aerssens J, Boonen S (1997) Bone density and local growth factors in generalized osteoarthritis. Microsc Res Tech 37:358–71
Allein S, Mihalopoulou E, Luypaert R, Louis O, Panayiotakis G, Eisendrath H (2000) MR phase imaging to quantify bone volume fraction: computer simulations and in vivo measurements. Magn Reson Imaging 18:275–9
Beuf O, Newitt DC, Mosekilde L, Majumdar S (2001) Trabecular structure assessment in lumbar vertebrae specimens using quantitative magnetic resonance imaging and relationship with mechanical competence. J Bone Miner Res 16:1511–9
Majumdar S, Thomasson D, Shimakawa A, Genant HK (1991) Quantitation of the susceptibility difference between trabecular bone and bone marrow: experimental studies. Magn Reson Med 22:111–27
Aigner N, Petje G, Steinboeck G, Schneider W, Krasny C, Landsiedl F (2001) Treatment of bone-marrow oedema of the talus with the prostacyclin analogue iloprost. An MRI-controlled investigation of a new method. J Bone Joint Surg Br 83:855–8
Wu Z, Yan X, Liu Z, Pan S, Cao X (1998) Avascular necrosis of the femoral head: MR imaging with radiological and histological correlation. Chin Med J (Engl) 111:599–602
McGibbon CA, Dupuy DE, Palmer WE, Krebs DE (1998) Cartilage and subchondral bone thickness distribution with MR imaging. Acad Radiol 5:20–5
Disler DG, McCauley TR, Kelman CG, et al (1996) Fat-suppressed three-dimensional spoiled gradient-echo MR imaging of hyaline cartilage defects in the knee: comparison with standard MR imaging and arthroscopy. Am J Roentgenol 167:127–32
Recht MP, Piraino DW, Paletta GA, Schils JP, Belhobek GH (1996) Accuracy of fat-suppressed three-dimensional spoiled gradient-echo FLASH MR imaging in the detection of patellofemoral articular cartilage abnormalities. Radiology 198:209–12
Frahm J, Haenicke W (1999) Rapid scan techniques. In: Stark DD, Bradley WG (eds) Magnetic resonance imaging, 3rd edn. Mosby, St. Louis, pp 87–124
Uhl M, Allmann KH, Tauer U, et al (1998) Comparison of MR sequences in quantifying in vitro cartilage degeneration in osteoarthritis of the knee. Br J Radiol 71:291–6
Snaps FR, Saunders JH, Park RD, Daenen B, Balligand MH, Dondelinger RF (1998) Comparison of spin echo, gradient echo and fat saturation magnetic resonance imaging sequences for imaging the canine elbow. Vet Radiol Ultrasound 39:518–23
Disler DG, Peters TL, Muscoreil SJ, et al (1994) Fat-suppressed spoiled GRASS imaging of knee hyaline cartilage: technique optimization and comparison with conventional MR imaging. Am J Roentgenol 163:887–92
Bredella MA, Losasso C, Moelleken SC, Huegli RW, Genant HK, Tirman PF (2001) Three-point Dixon chemical-shift imaging for evaluating articular cartilage defects in the knee joint on a low-field-strength open magnet. Am J Roentgenol 177:1371–5
Kwok WE, Totterman SM, Zhong J (2001) Interleaved water and fat dual-echo spin echo imaging with intrinsic chemical-shift elimination. J Magn Reson Imaging 13:318–23
Kwok WE, Totterman SM, Zhong J (2000) 3D interleaved water and fat image acquisition with chemical-shift correction. Magn Reson Med 44:322–30
Glover GH (1991) Multipoint Dixon technique for water and fat proton and susceptibility imaging. J Magn Reson Imaging. 1:521–30
Schick F (1998) Simultaneous highly selective MR water and fat imaging using a simple new type of spectral-spatial excitation. Magn Reson Med 40:194–202
Xiang QS (1997) An L. Water-fat imaging with direct phase encoding. J Magn Reson Imaging 7:1002–15
Brown MA, Semelka RC (1999) MRI. Basic principles and applications. 2nd edn. Wiley-Liss, New York
Woodward P (2001) MRI for technologists. Ch 14 Artifact, Wheeler GL 2nd edn. McGraw-Hill, New York, pp 263–284
Cohen ZA, McCarthy DM, Kwak SD, et al (1999) Knee cartilage topography, thickness, and contact areas from MRI: in-vitro calibration and in-vivo measurements. Osteoarthritis Cartilage 7:95–109
Stammberger T, Eckstein F, Michaelis M, Englmeier KH, Reiser M (1999) Interobserver reproducibility of quantitative cartilage measurements: comparison of B-spline snakes and manual segmentation. Magn Reson Imaging 17:1033–42
Dixon WT (1984) Simple proton spectroscopic imaging. Radiology 153:189–94
Wang Y, Li D, Haacke EM, Brown JJ (1998) A three-point Dixon method for water and fat separation using 2D and 3D gradient-echo techniques. J Magn Reson Imaging 8:703–10
Glover GH, Schneider E (1991) Three-point Dixon technique for true water/fat decomposition with B0 inhomogeneity correction. Magn Reson Med 18:371–83
Ma J, Wehrli FW, Song HK, Hwang SN (1997) A single-scan imaging technique for measurement of the relative concentrations of fat and water protons and their transverse relaxation times. J Magn Reson 125:92–101
Meyer CH, Pauly JM, Kerr A, Nishimura DG (1990) Simultaneous spatial and spectral selective excitation. Magn Reson Med 15:287–304
Tomasson D, Purdy D, Finn JP (1996) Phase-modulated binomial RF pulses for fast spectrally-selective musculoskeletal imaging. Magn Reson Med 35:563–8
Hardy PA, Recht MP, Piraino DW (1998) Fat supressed MRI of articular cartilage with a spatial-spectral excitation pulse. J Magn Reson Imaging 8:1279–87
Block W, Pauly J, Kerr A, Nishimura DG (1997) Consistent fat supression with compensated spectral-spatial pulses. Magn Reson Med 38:198–206
McGibbon CA (2002) Inter-rater and intra-rater reliability of subchondral bone and cartilage thickness measurement from MRI. In press: Magn Reson Imaging
Poage DP, Lerner CA (1998) Absence of chemical shift artifact on coronal T1-weighted MR images: an undescribed finding seen in osteochondral injuries of the knee in 12 patients. Am J Roentgenol 171:1521–3
Day JS, Ding M, van der Linden JC, Hvid I, Sumner DR, Weinans H (2001) A decreased subchondral trabecular bone tissue elastic modulus is associated with pre-arthritic cartilage damage. J Orthop Res 19:914–8
Calvo E, Palacios I, Delgado E, et al (2001) High-resolution MRI detects cartilage swelling at the early stages of experimental osteoarthritis. Osteoarthritis Cartilage. 9:463–72
Burr DB, Schaffler MB (1997) The involvement of subchondral mineralized tissues in osteoarthrosis: quantitative microscopic evidence. Microsc Res Tech 37:343–57
Saied A, Cherin E, Gaucher H, et al (1997) Assessment of articular cartilage and subchondral bone: subtle and progressive changes in experimental osteoarthritis using 50 MHz echography in vitro. J Bone Miner Res 12:1378–86
Lotke PA, Ecker ML, Barth P, Lonner JH (2000) Subchondral magnetic resonance imaging changes in early osteoarthrosis associated with tibial osteonecrosis. Arthroscopy 16:76–81
Bailey AJ, Mansell JP (1997) Do subchondral bone changes exacerbate or precede articular cartilage destruction in osteoarthritis of the elderly? Gerontology 43:296–304
Dieppe P (1999) Subchondral bone should be the main target for the treatment of pain and disease progression in osteoarthritis. Osteoarthritis Cartilage 7:325–6
Panula HE, Nieminen J, Parkkinen JJ, Arnala I, Kroger H, Alhava E (1998) Subchondral bone remodeling increases in early experimental osteoarthrosis in young beagle dogs. Acta Orthop Scand 69:627–32
Acknowledgements
The authors thank Dov Goldvasser, MscE, and Michael Treat, BS, for assistance with developing and testing the MRI protocols, and Michael S. Puniello, MS, PT, for assistance with preparing specimens. This study was supported by the National Institutes of Health (R01 AR45278).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McGibbon, C.A., Bencardino, J. & Palmer, W.E. Subchondral bone and cartilage thickness from MRI: effects of chemical-shift artifact. MAGMA 16, 1–9 (2003). https://doi.org/10.1007/s10334-003-0001-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-003-0001-0